Introduction
 Combined clinical and basic science efforts over several decades have enhanced our understanding of the underlying mechanisms and clinical spectrum of local anesthetic systemic toxicity (LAST). The APSF Newsletter has played an important role in educating clinicians and increasing awareness of the various presentations and optimal treatment of LAST, undoubtedly improving patient outcomes from this life-threatening iatrogenic complication. The changing landscape of regional anesthesia, characterized by new uses and forms of local anesthetics, has led to recent shifts in the clinical features and context of LAST.
Combined clinical and basic science efforts over several decades have enhanced our understanding of the underlying mechanisms and clinical spectrum of local anesthetic systemic toxicity (LAST). The APSF Newsletter has played an important role in educating clinicians and increasing awareness of the various presentations and optimal treatment of LAST, undoubtedly improving patient outcomes from this life-threatening iatrogenic complication. The changing landscape of regional anesthesia, characterized by new uses and forms of local anesthetics, has led to recent shifts in the clinical features and context of LAST.
In particular, the adoption of ultrasound guidance, catheter and intravenous infusions, local infiltration, and the expanding roles of regional anesthesia and local anesthetics in ERAS, multimodal analgesia, and possible cancer risk modification, require attention to the changing features of LAST.
Incidence
LAST can happen in any practice setting, but it is often ignored or underappreciated by practitioners until experienced firsthand. Reported estimates of its frequency vary greatly. Although some single-site studies at academic institutions report extremely low rates of LAST,1 recent analyses of large registry2 and administrative3,4 databases generally agree on a rate of approximately 1 per 1000 peripheral nerve blocks. However, given the strong likelihood of under-reporting, misdiagnosis, or other causes of failed case capture, it is possible the actual rate is higher.
Notably, Morwald et al. identified an overall rate for signs and symptoms consistent with LAST of 1.8/1000 peripheral nerve blocks during joint replacement; however, for the use of lipid emulsion, considered a surrogate for LAST, in the same population, they identified, for 2014, a rate during knee replacement of 2.6/1000 or 1 in 384 surgeries with a block.3 For a “rare event,” that’s not so rare! This reminds us of the need to remain vigilant for the possibility of LAST in virtually any patient receiving local anesthetic.
Risk
Understanding factors that increase risk is vital, as identifying patients with an elevated susceptibility to LAST enables clinicians to modify treatment and reduce the risk. Hypoxia and acidosis were recognized decades ago as factors predisposing to LAST.5 More recently identified co-morbidities include pre-existing heart disease (especially ischemia, arrhythmias, conduction abnormalities, and low ejection fraction), extremes of age, frailty, and conditions that cause mitochondrial dysfunction (e.g., carnitine deficiency); liver or kidney disease can also increase the risk of delayed LAST by depressing local anesthetic metabolism or disposition.5 Interestingly, Barrington and Kruger2 examined a registry of ~25,000 peripheral nerve blocks performed in Australia from January 2007 to May 2012 and identified 22 cases of LAST (overall incidence, 0.87 per 1000). They found that ultrasound guidance lowered the risk of LAST (odds ratio, 0.23, CI: 0.088–0.59, p=0.002)—presumably a result of fewer unidentified intravascular injections and possibly lower volumes of the drug used to achieve a block. Nevertheless, no single method can completely eliminate these events and roughly 16% of reported LAST occurred despite the use of ultrasound. Barrington and Kruger also noted that small patient size was a risk factor for LAST. The role of skeletal muscle as a large reservoir compartment for local anesthetic may explain this phenomenon and was confirmed in a rat model by Fettiplace et al.6 It is reasonable to adjust local anesthetic dose in all such “at-risk” patients or possibly avoid peripheral nerve block or local anesthetic infusion entirely if the risk is deemed too consequential. Surprisingly, Barrington and Kruger found 16 cases involving ropivacaine and the remainder were lidocaine-induced; notably, the LAST rate with lidocaine was approximately 5 times greater than that for ropivacaine.
Setting
Three large-scale studies have reviewed published case reports to identify the clinical spectrum of LAST over the past 40 years: DiGregorio et al.7 (Oct 1979–Oct 2009); Vasques et al.8 (March 2010–March 2014); and Gitman and Barrington9 (January 2014–November 2016). Data from these papers paints a picture of the evolving context of LAST with the latter two specifically covering the past decade. Between 1979 and 2009, epidural anesthesia and brachial plexus block each comprised around one-third of LAST cases. However, over the last decade, neuraxial (epidural and caudal) anesthesia has contributed only about 15% of published cases of LAST. Extremity blocks now make up about 20% of cases, and there are signals of concern related to both the penile block and local infiltration, each accounting for roughly 20% of reported cases. Interestingly, one institution reported a spike in LAST associated with dorsal penile block.10 They adopted system improvements in administering local anesthesia that led to an abrupt cessation of these events. The reviews indicate LAST has also been described after continuous intravenous infusion; paravertebral, peribulbar, transabdominis plane, and maxillary nerve blocks; topical administration in gel form; and after oral, esophageal, or tracheal mucosal application. A recent report described cardiac arrest after submucosal nasal injection of 120 mg of lidocaine.11 Clearly, LAST can occur anytime local anesthetics are used.
Roughly 80% of LAST cases over the past decade occurred in hospitals, ~10% in offices, and the remainder in emergency rooms or even at home. Anesthesia professionals or trainees were involved in about 60% of cases, with surgeons involved in approximately 30%, and the remainder spread among dentists, emergency physicians, pediatricians, cardiologists, and dermatologists. This reminds us of the need to take every opportunity to educate our colleagues about the risks and management of LAST.
Timing
The three large-scale studies show a trend to progressive delay in the onset of LAST over the past 40 years, reflecting the advent of both ultrasound guidance and catheter-based techniques. Competent use of ultrasound can reduce the chance of intravascular injection and immediate-onset LAST. Delays of more than 10 minutes in single-shot blocks occurred in only ~12% of cases before 2009 but in ~40% of those published in the last decade. Recent reports describe LAST with an onset that is temporally removed from the start of treatment by several hours or even days for catheter or intravenous infusion. This presumably occurs as the result of drug accumulation in target tissues and is a particular concern since both the timing and setting are problematic. The long interval can obscure the connection to local anesthetic administration; moreover, when LAST occurs “off-site,” away from the operating rooms, where it is rarely seen, the responsible caregivers are probably less mindful or knowledgeable of the problem, its detection, and treatment.
Presentation
LAST provokes a variable array of signs and symptoms of central nervous system (CNS) and cardiovascular (CV) toxicity (Table 1). These can be mild or severe and can occur separately or together. Isolated CNS symptoms occur in approximately half of reported cases, combined CNS and CV symptoms in about one-third and isolated CV symptoms in the remainder. Many of the latter occurred under general anesthesia or heavy sedation where CNS toxicity is difficult to ascertain. Seizure was the most common initial sign overall, occurring in roughly 50% of cases. Minor CNS features or “prodromes” such as tinnitus, metallic taste, hallucinations, slurred speech, limb twitching, extremity paresthesia, intention tremor, facial sensorimotor, and eye movement abnormalities were noted in only about 16% of patients by DiGregorio et al., but about 30% in combined data from Vasques et al. and Gitman et al.; this is consistent with an increase in LAST secondary to absorption or gradual onset during infusion. The most common presenting features of CV toxicity were arrhythmias (including bradycardia, tachycardia, VT/VF), conduction disturbances (bundle branch block, AV conduction block, widened QRS), hypotension, and cardiac arrest (including nonshockable rhythms, PEA, and asystole). Progressive toxicity (especially hypotension and bradycardia) with rapid deterioration over minutes is typical of severe LAST. It is impossible to predict which patients will progress. However, early treatment can delay or prevent progression; therefore, it is important to be prepared to intervene early in any patient receiving local anesthetic who has signs or symptoms consistent with LAST.
Table 1: Management of LAST
CLINICAL FEATURES OF LOCAL ANESTHETIC TOXICITY
| Risk Factors |
|
| Prevention |
|
| Presenting Symptoms and Signs | ||
| Prodrome | Major CNS | Major CV |
|
|
|
| Treatment of Local Anesthetic Systemic Toxicity |
|
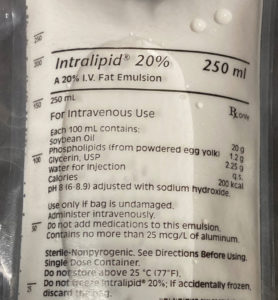
Initial resuscitation of LAST differs from standard CPR by focusing on reversing underlying toxicity rather than or in addition to sustaining coronary perfusion. Hence, initial emphasis is on seizure suppression and establishing normal arterial oxygen saturation since both acidosis and hypoxia aggravate LAST. For severe LAST, contact a perfusion team early to assure a path to extracorporeal support should CPR fail. During CPR, avoid local anesthetic anti-arrhythmics (they worsen LAST), beta blockers and calcium channel blockers (they depress contractility), and vasopressin (increasing afterload alone is undesirable since the poisoned heart doesn’t contract well). Epinephrine is acceptable for treating hypotension but should be used in small doses since it can impair lipid resuscitation, e.g., boluses <1 mcg/kg. Following the initial bolus of lipid emulsion given over 2–3 minutes, persistent LAST can be managed with repeated boluses and/or infusing lipid (0.25 mL/kg/min until stable or 200–250 mL/15–20 min). MAX DOSE: 12 mL/kg, ideal body weight. Propofol is not a substitute for lipid emulsion.
Liposomal formulation
 Liposomal bupivacaine (LB) harbors local anesthetic in a nanoparticle carrier matrix designed to prolong its action by slow release. Exparel® (Pacira Pharmaceuticals, San Diego, CA) comes in a 20-mL vial containing a total of 266 mg (1.3%) bupivacaine, which is the manufacturer’s maximum recommended dose for an adult patient. It was approved by the Food and Drug Administration (FDA) in 2011 for injection directly into the operative site to augment postoperative analgesia and later in 2018 for interscalene brachial plexus block.12 Three percent of the drug is free and presumably initiates a certain level of analgesia upon administration. Blood levels of bupivacaine can last up to 96 hours after injection of LB; therefore, patients must be adequately monitored for delayed toxicity. As with any local anesthetic, patients with specific co-morbidities are at an increased risk for developing acute or delayed toxicity, either as a result of increased sensitivity (e.g., ischemic heart disease) or impaired metabolism (e.g., liver disease) with resulting increased plasma levels of bupivacaine.
Liposomal bupivacaine (LB) harbors local anesthetic in a nanoparticle carrier matrix designed to prolong its action by slow release. Exparel® (Pacira Pharmaceuticals, San Diego, CA) comes in a 20-mL vial containing a total of 266 mg (1.3%) bupivacaine, which is the manufacturer’s maximum recommended dose for an adult patient. It was approved by the Food and Drug Administration (FDA) in 2011 for injection directly into the operative site to augment postoperative analgesia and later in 2018 for interscalene brachial plexus block.12 Three percent of the drug is free and presumably initiates a certain level of analgesia upon administration. Blood levels of bupivacaine can last up to 96 hours after injection of LB; therefore, patients must be adequately monitored for delayed toxicity. As with any local anesthetic, patients with specific co-morbidities are at an increased risk for developing acute or delayed toxicity, either as a result of increased sensitivity (e.g., ischemic heart disease) or impaired metabolism (e.g., liver disease) with resulting increased plasma levels of bupivacaine.
Administration of non-bupivacaine local anesthetics within 20 minutes of Exparel, which can occur when a surgeon and an anesthesia professional fail to communicate, may cause a sudden release of liposomal bupivacaine, dangerously increasing free plasma bupivacaine concentrations; the exact mechanism of this phenomenon is not elucidated. Toxicity of the two local anesthetics is then additive. Burbridge and Jaffe13 emphasize the importance of safety measures such as educating the operating room staff as well as a “time-out” label on the drug vial to prompt discussion around avoiding simultaneous administration of other local anesthetics within 20 minutes of Exparel injection.
The FDA Adverse Event Reporting System (FAERS) database contains reports submitted by practitioners and consumers. An analysis of FAERS data received between January 1, 2012, and March 31, 2019, where Exparel was listed as the suspect medicinal product and signs or symptoms of LAST occurred (seizure or both CNS symptoms and CV disturbance), were studied by disproportionality analysis—a pharmacovigilance tool that measures the “Information Component” (IC025) and is used by the World Health Organization.14 This compares the rate at which a particular event of interest co-occurs with a given drug versus the rate this event occurs without the drug in the event database. If the lower limit of the 95% confidence interval of the IC025 is greater than zero, then there is a statistically significant signal. Such an adverse event signal was found between LAST and liposomal bupivacaine. From January 1, 2012, to March 31, 2019, the analysis yielded an overall IC025 of 1.65. Splitting the dataset into two time periods (January 2012 to December 2015 and January 2016 to March 2019) showed persistence of a significant signal in both time periods. While this does not prove a causal relationship, it nevertheless points to a statistically significant signal between Exparel and signs or symptoms of LAST.
Reporting of LAST is problematic
A recent Cochrane Library update of perioperative intravenous lidocaine infusion by Weibel et al.15 found that of 68 clinical trials comparing lidocaine infusion with thoracic epidural analgesia, 18 did not comment on adverse events at all. Unfortunately, the degree of heterogeneity in the reporting methods of the remaining 50 studies precluded a meta-analysis of these data. There is clearly a need to improve and standardize ascertainment and reporting of LAST in clinical trials involving local anesthetics. This applies particularly to studies of catheter and intravenous infusions where systems for identifying LAST are not as robust as in the operating room. Until this occurs, understanding the associated risks will remain hampered by reliance on anecdotal reports and personal experience.
Treatment
In 2010 the Association of Anaesthetists of Great Britain and Ireland (AAGBI) and the American Society of Regional and Pain Medicine (ASRA) Working Group on Local Anesthetic Toxicity separately published first-ever recommendations for a systematic approach to treating LAST.16 Both groups focused on airway management and seizure suppression along with the rapid infusion of lipid emulsion as key elements specific to treating LAST (Table 1).
Interestingly, the rate of published reports increased from ~3 LAST cases per year before 2009 to ~16/year in the last decade. If reporting bias is constant, this could reflect greater willingness to report events as patient outcomes improved over the past decade. ASRA has updated their advisory twice since 2010 with modifications that include the adoption of a checklist approach and a simpler method for infusing lipid emulsion.5 Two key points deserve mention. First, mechanism informs method. Infusing lipid emulsion reverses LAST by accelerating the redistribution of local anesthetic.6 This results from partitioning and a direct inotropic effect exerted by lipid emulsion17 that combine to “shuttle” drug away from sensitive organs (brain, heart) to reservoir organs (skeletal muscle, liver). This requires infusing a relatively large quantity of lipid quickly (e.g., ~1.5 mL/kg over ~2 minutes) to establish a lipid “bulk phase” in the plasma. The bolus infusion may be repeated or followed by an infusion at a slower rate—the difference in method is likely not as important as the need to sustain a bulk phase. An important study by Liu et al.18 showed in a rat model of bupivacaine toxicity that repeated bolus dosing is superior to bolus + infusion in reversing LAST. However one chooses to deliver lipid, it is important to respect the upper dosing limit of ~10–12 mL/kg ideal body weight to avoid fat overload. That is, don’t forget to turn it off! Second, the treatment strategy for CV instability in LAST differs from that used for ischemic cardiac arrest since the underlying pathophysiology of ischemia and pharmaco-toxicity differ. Therefore, it is preferable to treat the underlying toxicity by infusing lipid and, if needed, use reduced doses of epinephrine (boluses ~1 mcg/kg) to support blood pressure.19 Vasopressin should be avoided since increasing afterload alone has no benefit and a deleterious effect has been confirmed in animal models.20 It is sensible to alert a perfusion team at the outset of a severe event so that alternative, extracorporeal methods of circulatory support can be readied should initial resuscitation fail.
Conclusions
LAST can occur anytime local anesthetics are used. Even with appropriate dosing and perfect technique, patient susceptibility, system problems, and random errors prevent its eradication. The increasing use of regional anesthesia in an agng population, and the advent of catheter and intravenous infusion of local anesthetic for opiate-sparing anesthesia, multimodal analgesia, or cancer risk modification assure that LAST will continue to occur increasingly at unexpected sites and with delayed timing despite our best efforts. Identifying “at-risk” patients and improving system safety will reduce the likelihood of LAST.
Clinicians should have a treatment plan ready for LAST wherever local anesthetics are used. Any unusual CNS signs or CV instability in the setting of regional anesthesia, anesthetic infiltration, or infusion should be considered possible LAST until proven otherwise, since early intervention can prevent or slow progression. Anesthesia professionals must actively educate other health care providers who administer local anesthetics to patients. This includes informing those in other specialties having a syringe in hand and staff on the floor responsible for care of patients receiving local anesthetic infusion. Improved models of LAST and its treatment will continue to inform measures we can adopt to improve patient safety and save lives.
Dr. Weinberg is a professor of Anesthesiology at the University of Illinois College of Medicine at Chicago and staff physician at the Jesse Brown VA Medical Center, Chicago, IL.
Dr. Rupnik is a consultant anesthetist at the Balgrist University Hospital, Zurich, Switzerland.
Dr. Aggarwal is a hospital resident at Yale New Haven hospital, New Haven, Connecticut.
Dr. Fettiplace is a resident in Anesthesiology at Massachusetts General Hospital, Boston, MA.
Dr. Gitman is an assistant professor of Anesthesiology at the University of Illinois College of Medicine, Chicago, IL.
Dr. Weinberg is an officer and shareholder of ResQ Pharma, Inc., and maintains the educational website, www.lipidrescue.org. Drs. Rupnik, Aggarwal, Fettiplace, and Gitman have no conflicts of interest.
References
- Liu SS, Ortolan S, Sandoval MV, et al. Cardiac arrest and seizures caused by local anesthetic systemic toxicity after peripheral nerve blocks: should we still fear the reaper? Reg Anesth Pain Med. 2016;41:5–21.
- Barrington MJ, Kluger R. Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth Pain Med. 2013;38:289–97.
- Morwald EE, Zubizarreta N, Cozowicz C, et al. Incidence of local anesthetic systemic toxicity in orthopedic patients receiving peripheral nerve blocks. Reg Anesth Pain Med. 2017;42:442–445.
- Rubin DS, Matsumoto MM, Weinberg G, et al. Local anesthetic systemic toxicity in total joint arthroplasty: incidence and risk factors in the United States from the national inpatient sample 1998–2013. Reg Anesth Pain Med. 2018; 43:131–137.
- Neal JM, Barrington MJ, Fettiplace MR, et al. The third American Society of Regional Anesthesia and Pain Medicine practice advisory on local anesthetic systemic toxicity: executive summary 2017. Reg Anesth Pain Med. 2018;43:113–123.
- Fettiplace MR, Lis K, Ripper R, et al. Multi-modal contributions to detoxification of acute pharmacotoxicity by a triglyceride micro-emulsion. J Control Release. 2015;198:62–70.
- Di Gregorio G, Neal JM, Rosenquist RW, et al. Clinical presentation of local anesthetic systemic toxicity: a review of published cases, 1979 to 2009. Reg Anesth Pain Med. 2010;35:181–187.
- Vasques F, Behr AU, Weinberg G, et al. A review of local anesthetic systemic toxicity cases since publication of the American Society of Regional Anesthesia recommendations: to whom it may concern. Reg Anesth Pain Med. 2015;40: 698–705.
- Gitman M, Barrington MJ. Local anesthetic systemic toxicity: a review of recent case reports and registries. Reg Anesth Pain Med. 2018;43:124–130.
- Yu RN, Houck CS, Casta A, et al. Institutional policy changes to prevent cardiac toxicity associated with bupivacaine penile blockade in infants. A A Case Rep. 2016;7:71–75.
- Weber F, Guha R, Weinberg G, et al. Prolonged pulseless electrical activity cardiac arrest after intranasal injection of lidocaine with epinephrine: a case report. A A Pract. 2019; 12:438–440.
- Balocco AL, Van Zundert PGE, Gan SS, et al. Extended release bupivacaine formulations for postoperative analgesia: an update. Curr Opin Anaesthesiol. 2018;31:636–642.
- Burbridge M, Jaffe RA. Exparel®: a new local anesthetic with special safety concerns. Anesth Analg. 2015;121:1113–1114.
- Aggarwal N. Local anesthetics systemic toxicity association with Exparel® (bupivacaine liposome)—a pharmacovigilance evaluation. Expert Opin Drug Saf. 2018;17:581–587.
- Weibel S, Jelting Y, Pace NL, et al. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery in adults. Cochrane Database Syst Rev. 2018;6: CD009642.
- Weinberg GL. Treatment of local anesthetic systemic toxicity (LAST). Reg Anesth Pain Med. 2010;35:188–93.
- Fettiplace MR, Ripper R, Lis K, et al. Rapid cardiotonic effects of lipid emulsion infusion.* Crit Care Med. 2013;41: e156–162.
- Liu L, Jin Z, Cai X, et al. Comparative regimens of lipid rescue from bupivacaine-induced asystole in a rat model. Anesth Analg. 2019;128:256–263.
- Weinberg GL, Di Gregorio G, Ripper R, et al. Resuscitation with lipid versus epinephrine in a rat model of bupivacaine overdose. Anesthesiology. 2008;108: 907–913.
- Di Gregorio G, Schwartz D, Ripper R, et al. Lipid emulsion is superior to vasopressin in a rodent model of resuscitation from toxin-induced cardiac arrest. Crit Care Med. 2009;37: 993–999.


 Issue PDF
Issue PDF