This year the first-place Ellison C. Pierce, Jr., M.D. Award for Best Abstract in Patient Safety was awarded to Kajstura and colleagues for their work entitled “Best Practice Advisories Increase Transfusion Guideline Compliance, Reduce Blood Utilization, and Save Cost.” In this review, they describe how the patient blood management program across the Johns Hopkins Health System has had positive impacts on patient safety, guideline compliance, and cost savings.
The 2019 first-place Ellison C. Pierce, Jr., MD, Award for Best Abstract in Patient Safety was awarded to Kajstura and colleagues for their work entitled “Best Practice Advisories Increase Transfusion Guideline Compliance, Reduce Blood Utilization, and Save Cost.” In this review, they describe how the patient blood management program across the Johns Hopkins Health System has had positive impacts on patient safety, guideline compliance, and cost savings.
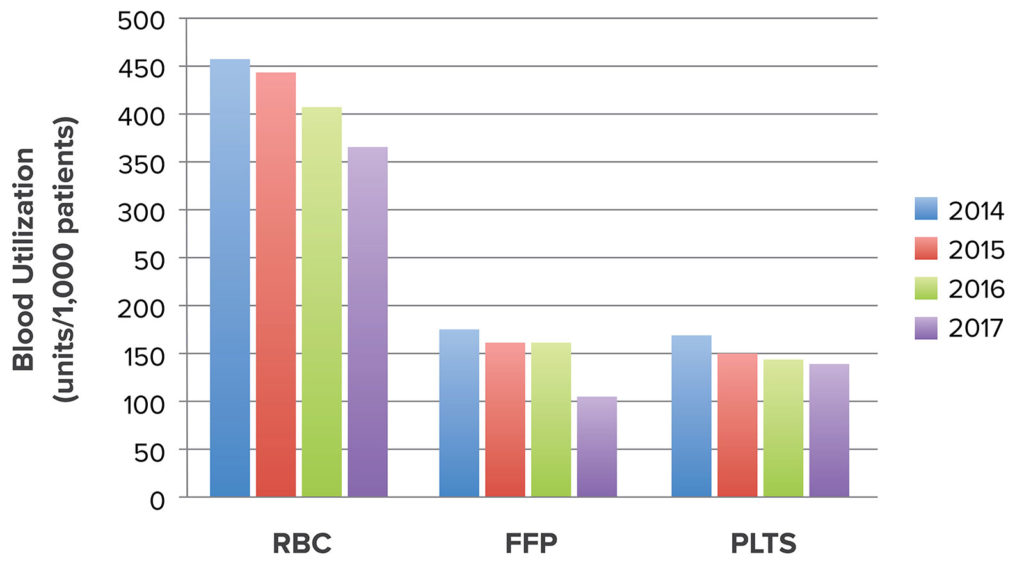
Figure 1: Across the entire health system, for each of the three blood components, changes in utilization (number of units per 1,000 patients) are shown over time. RBC–red blood cell, FFP–plasma, PLTS–platelets.
Permission to reuse granted by Wolters Kluwer Health. Reprinted from Frank SM, et al. Anesthesiology. 2017;127: 754-764.2
Within the Johns Hopkins Health System, a variety of approaches have been implemented under the patient blood management program which are summarized in Table 1.1,2 At the heart of the program is education, since over the past decade multiple landmark studies have been published supporting the concept that “less is more” when it comes to transfusion.3 In addition, transfusion guidelines were reinforced by best practice advisories (pop-up alerts) in the electronic order sets, to inform clinicians when orders were placed outside of guidelines.2,4
Table 1. Methods Used to Improve Blood Utilization Across the Health System
| 1. Obtain financial support from health system leadership. |
| 2. Assemble a multidisciplinary team for monthly meetings. |
| 3. Education: Grand rounds and on-line tutorials emphasizing evidence-based transfusion guidelines. |
| 4. Harmonizing transfusion guidelines across the health system. |
| 5. A “Why Give 2 When 1 Will Do?” single-unit red cell transfusion campaign.5 |
| 6. Screen saver images reinforcing transfusion guidelines. |
| 7. Clinical decision support with best practice advisories (best practice alerts, pop-up alerts).1 |
| 8. Data acquisition and analytics. |
| 9. Transfusion guideline compliance audits with feedback (provider specific). |
| 10. Minimizing iatrogenic blood loss (smaller phlebotomy tubes and less testing). |
| 11. Anesthetic management: (normothermia, controlled hypotension, antifibrinolytics, acute normovolemic hemodilution).6 |
| 12. Surgical methods: (minimally invasive approaches, newer electrocauteries, topical hemostatic agents). |
| 13. Cell salvage.7 |
These individual efforts have resulted in a large positive system-wide effect. Since the implementation of the patient blood management program, overall transfusion rates have decreased by 20% for red blood cells (P = 0.0001), 39% for plasma (P = 0.0002), and 16% for platelets (P = 0.04) (Figure 1).2 Guideline compliance has increased, with 35% fewer out-of-guideline transfusion orders for red blood cells, 9% fewer for plasma, and 3% fewer for platelets. By reducing unnecessary transfusions, the hospital system has seen a significant cost savings; comparing fiscal year 2017 (after most of these efforts were implemented) to 2014. There was an annual savings of $2.4 million for the three blood products combined, representing a 400% return on investment for support of the program.2 Most importantly, these changes are having a positive impact on patient safety with measures such as length of stay showing no change, morbidity/mortality decreasing from 1.5% to 0.75% (P = 0.035), and 30-day readmission rate decreasing from 9.0% to 5.8% (P = 0.0002).8 The success of this initiative at the Johns Hopkins Health System in patient blood management was in part predicated on the diverse array of health care professionals and allies coming together with the common goal of optimizing the care of patients who may need transfusion.
Tymoteusz J. Kajstura is a medical student at Johns Hopkins University and Dr. Frank is professor in the Department of Anesthesiology and Critical Care Medicine and medical director of the Blood Management Program at The Johns Hopkins Health System.
The authors have no conflicts of interest.
References
- Sadana D, Pratzer A, Scher LJ, et al. Promoting high-value practice by reducing unnecessary transfusions with a patient blood management program. JAMA Intern Med. 2018;178:116–122.
- Frank SM, Thakkar RN, Podlasek SJ, et al. Implementing a health system-wide patient blood management program with a clinical community approach. Anesthesiology. 2017;127:754–764.
- Carson JL, Guyatt G, Heddle NM, et al. Clinical Practice Guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA. 2016;316:2025–2035.
- Yang WW, Thakkar RN, Gehrie EA, et al. Single-unit transfusions and hemoglobin trigger: relative impact on red cell utilization. Transfusion. 2017;57:1163–1170.
- Podlasek SJ, Thakkar RN, Rotello LC, et al. Implementing a “Why give 2 when 1 will do?” Choosing Wisely campaign. Transfusion. 2016;56:2164.
- Grant MC, Resar LM, Frank SM. The efficacy and utility of acute normovolemic hemodilution. Anesth Analg. 2015;121:1412–1414.
- Frank SM. Who benefits from red blood cell salvage?–Utility and value of intraoperative autologous transfusion. Transfusion. 2011;51:2058–2060.
- Gupta PB, DeMario VM, Amin RM, et al. Patient blood management program improves blood use and clinical outcomes in orthopedic surgery. Anesthesiology. 2018;129:1082–91.


 Issue PDF
Issue PDF