INTRODUCTION
Surgeons operate on patients with a significant comorbidity burden. Despite this, the intraoperative period is now safer than ever. However, postoperative adverse events are astonishingly common, accounting for approximately 7.7% of all global deaths annually.1 The most common causes of postoperative mortality in the first 30 days after noncardiac surgery include major bleeding, myocardial injury after noncardiac surgery (MINS), and sepsis, in that order.2 Importantly, these three entities, taken together, account for about half of all postoperative mortality.2 Myocardial injury may be underestimated, as it is especially difficult to detect; it is essentially “silent myocardial infarction” with high-sensitivity troponin T (hsTnT) elevation being the only criteria necessary for diagnosis.3 In the postoperative period, MINS is suggested when the threshold peak hsTnT increases by at least 5 ng/L from the preoperative concentration to at least 20 ng/L or to above 65 ng/L irrespective of baseline concentration.4 MINS has a strong association with both intraoperative and postoperative hypotension; however, most MINS occurs in the first three postoperative days, which suggests that postoperative hypotension may be a major contributor.4,5
In terms of clinical presentation, when one imagines a patient suffering a significant adverse event leading to mortality in the postoperative period, it is most often assumed to be an abrupt catastrophic cardiopulmonary collapse. In actuality, the majority of patients who suffer an in-hospital cardiopulmonary arrest have aberrations in one or more vital signs during the few hours leading up to the event, with a higher risk of mortality with increasing numbers of pre-arrest vital sign abnormalities.6 At least half of such patients are admitted to wards6,7 and therefore, monitoring of their vital signs is usually intermittent8 and these foreboding perturbations often go unnoticed prior to these devastating events. As such, improved ward monitoring of vital signs with wearable devices may be a transformative perioperative patient safety measure with potential to dramatically reduce patient harm.9,10 While there is no textbook definition, a “wearable device” is generally a noninvasive, autonomous device that continuously monitors patient data using sensors. Challenges remain with evidence building, including return on investment and actual implementation of these measures on a routine basis.
RATIONALE FOR WARD MONITORING
Continuous Ward Monitoring May Improve Outcomes
Patients in hospital wards are left under-monitored due to a combination of potential factors, including, but not limited to, staffing shortages, understanding trending vital signs and deterioration on the non-ICU units, lack of adequate monitoring capabilities, and the inability to mitigate the obvious threat of alarm fatigue. In contrast to patients admitted to the ICU, whose nurses oftentimes care for at most two patients and vital signs are measured continually or at least hourly, patients admitted to the ward environment are frequently cared for by nurses who are responsible for many more patients and only receive intermittent vital sign monitoring, every four to twelve hours.8 While rapid response teams are prevalent, the afferent arm of these medical emergency teams are linked to intermittently measured vital signs. Delays of a mere 15 minutes or more in the recognition of deterioration increase the risk of adverse outcomes.11 It makes sense that better clinical outcomes after a rapid response may be seen if early warning scores are linked to continuous ward monitoring. A potential benefit of implementation of ward monitoring is early intervention and an overall decrease in rapid response calls.11 Current ward monitoring standards miss an opportunity for early pattern recognition and intervention in real time, and do not learn from recorded patterns that would help change the way we care for our patients in the future. Many members of the medical community recognize a need for continuous ward monitoring, with nearly all anesthesia professionals in one survey believing that continuous monitoring of blood pressure, heart rate, and pulse oximetry are indicated in at least high-risk patients.8
Unfortunately, subjective intermittent vital sign measurements are prone to artifact and inaccuracy due to both imprecise assessments and unrecognized device malposition.12 Some evidence suggests that heart and respiratory rate are the two vital signs that are most predictive of a future combined outcome of cardiac arrest, intensive care unit transfer, and death.13 Respiratory rate is a frequent offender for imprecise manual recordings done by bedside providers, while concurrently trending changes measured with automated wearable monitoring show a significant difference in the lead up to a critical event. More recently, machine learning analytics have been developed with age, and continuous heart rate and respiratory rate, which have been found to be predictive of transfer to an ICU and death.14 As such, intermittent ward monitoring leads to frequent misses of hemodynamic and respiratory vital sign perturbations15-18 and potentiating reactive rather than proactive patient care interventions.
MISSED DIAGNOSIS OF POSTOPERATIVE HYPOTENSION AND HYPOXEMIA
In addition to changes in respiratory and heart rate, postoperative hypotension may also play a role in postoperative adverse events such as MINS and mortality.19 It can be common, persistent, profound, and frequently undetected.15,19,20 For example, about half of all episodes of mean arterial pressures below 65 mmHg are missed with intermittent monitoring on hospital wards.15 Similarly, postoperative hypoxemia is common, prolonged and profound in both severity and duration. Twenty-one percent of postoperative noncardiac inpatients were found to have ≥10 minutes SpO2 < 90% per hour in patients with clinician-blinded monitoring. More than 90% of desaturation episodes (<90% for a continuous hour) were missed using routine measurements at 4-hour intervals.18 Unlike postoperative hypotension, the implications of prolonged undetected hypoxemia remain unclear. An important unexplored area is the concurrent trending changes in heart rate, respiratory rate, blood pressure and oxygen saturation, and the implications of such trends on organ system failure on hospital floors. For example, it is appealing to speculate that undetected tachycardia on hospital ward patients would be even more deleterious in the setting of hypotension due to the increased myocardial oxygen demand, however, these relationships have as yet not been investigated.
OPIOID-INDUCED RESPIRATORY DEPRESSION
Opioid-induced respiratory depression is an important perioperative adverse event, especially in the subset of older male patients with heart failure and sleep disordered breathing.21 About half of all patients in the PRODIGY study suffered at least one episode of opioid-induced respiratory depression that was detected using continuous capnography and oximetry and adjudicated using stringent criteria to separate artifact.21 Among a cohort of postoperative patients, about one in five suffered from a desaturation to less than 90% each hour, with the majority of these missed by intermittent vital sign monitoring.16 Approximately 40% of patients suffering an acute respiratory event on the ward will die.22 In line with this, closed claims data for opioid-induced respiratory depression suggests that about half of these occur within two hours of the last nursing check and almost all are preventable with better monitoring and education.23
There is a large and growing cohort of data supporting ward monitoring devices even though most studies examining these devices are primarily observational, retrospective, and before-and-after design studies of insufficient power to really drive dramatic change. These types of data sets help understand real-world utilization and possibly help factor in alarm fatigue and other barriers to adoption. A substantial reduction in the number of rapid response calls, rescue events, and ICU transfers as well as rates of cardiac arrest have been demonstrated after implementation of ward monitoring, including entirely wearable solutions.24-26 While appropriately powered, prospective interventional randomized trials of monitoring type with a clinical outcome may be ideal, these are yet to be performed, and are logistically challenging, especially if individual patient level randomization and intervention in an average-sized patient ward with numerous patients and limited staffing is considered.
IMPLEMENTATION
At Wake Forest University Medical Center, we implemented continuous ward monitoring using a wireless, wearable solution which captures heart rate, respiratory rate, oxygen saturation, blood pressure, atrial fibrillation, patient mobility, and body temperature every 15 seconds. A study comparing the post implementation data with a pre-implementation historical cohort showed a decrease in rapid response call frequency was statistically significant (189 to 158 per 1000 discharges, P = 0.036).27 This is in line with a historical cohort compared with currently implemented ward monitoring at a large hospital system in the United Kingdom, which reported a substantial reduction in ICU admissions and rapid response calls using the same wireless continuous monitoring technology as ours.26 Recently, we compared 12,345 patients with intermittent spot-check monitoring in 2018 and 2019 against a propensity-matched cohort of 7,955 postsurgical patients receiving continuous portable monitoring during the same time period and recovering from surgery on different hospital floors at our institution.28 Patients who received continuous ward monitoring were three-and-a-half times less likely to be transferred to the ICU or to die during index hospitalization compared to those who did not and were less likely to experience heart failure, myocardial infarction, or kidney injury.28 Interestingly, a ward cluster, randomized, pragmatic, alternative interventions trial from our institution in 2020 and 2021 also demonstrated a significant reduction in the risk of a composite of blood pressure, oxygen saturation, and heart rate changes in favor of continuous monitoring (NCT04574908, clinicaltrials.gov). We also surveyed myocardial injury after noncardiac surgery, and this did not appear to be significantly different in either group.
POSTOPERATIVE MOBILITY AND POSTURE
While traditional vital signs have been monitored on at least an intermittent basis on hospital wards, patient movement is a relatively newer paradigm that is closely linked to the improvement of the postsurgical recovery process. Mobility is, in fact, an often-underappreciated facet of postoperative monitoring in the hospital, while curiously well-tracked using a multitude of tracking devices at home. At Wake Forest, our monitoring solution also includes 3-axis accelerometers positioned on the trunk to identify posture status as upright 90°, upright 45°, supine, lying on one side, walking, and fallen. We examined patient outcomes from a dataset of nearly 9,000 patients recovering from surgery on hospital wards. Data was recorded at 15-second intervals and patients were considered mobilized when their posture was identified as upright 90° and walking posture. Our final confounder-adjusted analysis reported a significant association between each 4-minute increase in mobilization and a composite outcome (hazard ratio [HR], 0.75; 95% CI, 0.67-0.84; P < .001) which included myocardial injury, ileus, stroke, venous thromboembolism, pulmonary complications, and all-cause in-hospital mortality.
In addition, there was a reduction in hospital length of stay by 0.12 days (95% CI, 0.09-0.15; P < .001) associated with increasing mobility.29 While unobserved confounding in this data cannot be ruled out, the signal seen here should encourage future interventional trials that bundle mobility-based interventions with continuously monitored traditional vital signs.
WEARABLE WARD MONITORING SYSTEMS
The medical and ambulatory communities have been replete with wearable medical devices since the advent of wireless and compact pulse oximetry, minimally-invasive arrhythmia monitoring, continuous glucose monitoring devices, and wireless insulin infusion and breast pumps. As such, it has been a relatively simple translation to design wearable monitoring devices for the inpatient setting, though most devices struggle with accurate validation data and interventional outcome trials (Table 1).8 For those that get beyond this stage, implementation on hospital wards remains a challenge.
Table 1. Features of an Ideal Hospital Ward Monitoring System8
| Evaluation of evidence, stakeholder engagement, and education of personnel before implementation |
| Noninvasive, portable cardiorespiratory vital signs measurement including mobility and position data |
| Continuous and modifiable frequency of monitoring |
| Monitoring display that allows for integrated focused trends, unified signals, and that prevents information overload |
| Threshold-based alarms connected with rapid response paging systems and early warning scores |
| Alarm control and delays that can be adjusted at the level of the device and central monitoring station |
| Automated and high-frequency data flow into device data servers and cloud-based storage |
| Generates accurate, reliable, and reproducible data |
| Minimal artifact interference from other monitors |
| Data flow to other devices (patient monitors, central monitoring platforms, and/or other portable or mobile devices) |
| Integrated seamlessly with the electronic medical record |
| Easily extractable data (including waveform data) with accurate time stamps |
| Layered predictive analytics to guide proactive interventions |
| AI-based suggested intervention protocols tagged to various combinations of changes in vital signs and alarms |
IMPLEMENTATION CHALLENGES
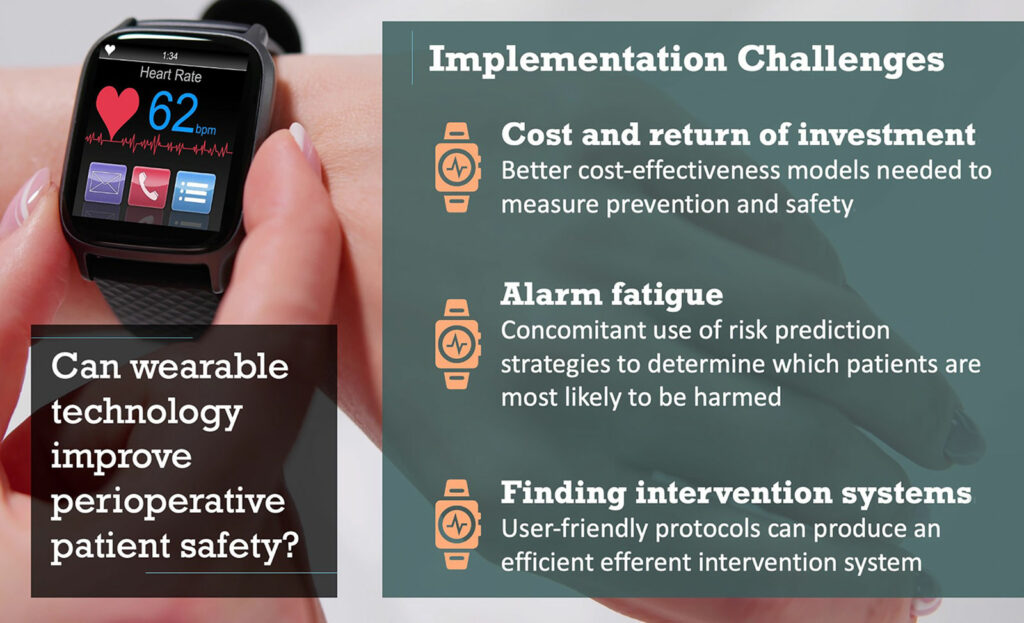
Implementation of Continuous Ward Monitoring Remains a Major Challenge
Despite what appears to be an easily deployable tool with apparent benefit, wearable monitoring devices are fraught with implementation challenges, particularly related to cost and return on investment, security risks, data handling, and technical issues, including concerns regarding artifact and connectivity.8,10 While up-front costs are significant, cost savings from even minimal reductions in poor patient outcomes are likely to overcome these initial expenditures quite quickly.21,30 However, this is also an opportunity to perform better cost-effectiveness analyses that model the set-up and annual maintenance of continuous monitoring against the cost of an unwanted ICU admission, an ICU bed that was lost, an extended hospital length of stay, and organ system failure secondary to under-recognized hemodynamic and respiratory changes.
The primary functional hurdle post implementation of these devices remains alarm fatigue due to such a dramatically increased amount of available data. As such, ward monitoring implementation requires concomitant use of risk prediction strategies to determine which patients are most likely to be harmed and thus benefit.21,31 Further, optimization of these systems may include the creation and implementation of machine learning, pattern detection technology, and artificial intelligence as well as development of minimally invasive advanced cardiac physiologic monitoring modalities.
The use of continuous monitoring on hospital units will also necessitate that we partner with our nursing colleagues and scientists who help with research and development of these wearable sensors upfront and before these are sent to the market. Finally, an appropriate and effective efferent intervention system that is protocolized and user-friendly for providers in the non-ICU clinical areas of the hospital is necessary. This may facilitate health care professionals to execute early, appropriate interventions, particularly in those patients that show persistent vital signs trending in the wrong direction.
CONCLUSION
More Research is Welcomed to Further Validate Widespread Adoption of Wearables
In summary, continuous ward monitoring with wearable devices holds significant promise in improving patient safety and outcomes. Implementation challenges persist, but may be overcome with better-conducted research to support a change in current monitoring practices.
Megan H. Hicks, MD, is an assistant professor of anesthesiology at Wake Forest University School of Medicine, Winston-Salem, NC.
Ashish K. Khanna, MD, is an associate professor of anesthesiology and vice chair of research at Wake Forest University School of Medicine, Winston-Salem, NC.
Megan H. Hicks, MD, has no conflicts of interest.
Ashish K. Khanna, MD, consults for Medtronic, Edwards Life Sciences, Philips Research North America, Fifth Eye Inc., GE Healthcare, Potrero Medical, Retia Medical and Caretaker Medical. His work on ward monitoring was funded with a Clinical and Translational Science Institute (CTSI) NIH/NCTAS KL2 TR001421 award.
REFERENCES
- Nepogodiev D, Martin J, Biccard B, et al. Global burden of postoperative death. Lancet. 2019;323(10170):401. PMID: 30722955.
- Spence J, LeManach Y, Chan MTV, et al. Association between complications and death within 30 days after noncardiac surgery. CMAJ. 2019;191:E830–837. PMID: 31358597.
- Writing Committee for the VSI, Devereaux PJ, Biccard BM, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2017;317:1642–1651. PMID: 28444280.
- Ruetzler K, Khanna AK, Sessler DI. Myocardial injury after noncardiac surgery: preoperative, intraoperative and postoperative aspects, implications, and directions. Anesth Analg. 2020;13):173–186. PMID: 31880630.
- Sessler DI, Khanna AK. Perioperative myocardial injury and the contribution of hypotension. Intensive Care Med. 2018;44:811–822. PMID: 29868971.
- Andersen LW, Berg KM, Chase M, et al. Acute respiratory compromise on inpatient wards in the United States: Incidence, outcomes, and factors associated with in-hospital mortality. Resuscitation. 2016;105:123-9. PMID: 27255952.
- Perman SM, Stanton E, Soar J, et al. Location of in-hospital cardiac arrest in the United States—variability in event rate and outcomes. J Am Heart Assoc. 2016;5:e003638. PMID: 27688235.
- Michard F, Thiele RH, Saugel B, et al. Wireless wearables for postoperative surveillance on surgical wards: a survey of 1158 anaesthesiologists in Western Europe and the USA. BJA Open. 2022;23:1:100002. PMID: 37588692.
- Hemapriya D, Viswanath P, Mithra VM, et al. Wearable medical devices—design challenges and issues. IEEE International Conference on Innovations in Green Energy and Healthcare Technologies (ICIGEHT’17). March 2017. doi: 10.1109/IGEHT.2017.8094096.
- Khanna AK, Hoppe P, Saugel B. Automated continuous noninvasive ward monitoring: future directions and challenges. Crit Care. 2019;23(1):194. doi.10.1186/s13054-019-2485-7.
- Michard F, Kalkman CJ. Rethinking patient surveillance on hospital wards. Anesthesiology. 2021;135:531–540. PMID: 34237129.
- Badawy J, Nguyen OK, Clark C, et al. Is everyone really breathing 20 times a minute? Assessing epidemiology and variation in recorded respiratory rate in hospitalised adults. BMJ Qual Saf. 2017;26:832–836. PMID: 28652259.
- Churpeck MM, Adhikari R, Edelson DP. The value of vital sign trends for detecting clinical deterioration on the wards. Resuscitation. 2016;102:1–5. PMID: 26898412.
- Akel MA, Carey KA, Winslow CJ, et al. Less is more: Detecting clinical deterioration in the hospital with machine learning using only age, heart rate, and respiratory rate. Resuscitation. 2021;168:6–10. PMID: 34437996.
- Turan A, Chang C, Cohen B, et al. Incidence, severity, and detection of blood pressure perturbations after abdominal surgery: a prospective blinded observational study. Anesthesiology. 2019;130:550–559. PMID: 30875354.
- Saab R, Wu BP, Rivas E, et al. Failure to detect ward hypoxaemia and hypotension: contributions of insufficient assessment frequency and patient arousal during nursing assessments. Br J Anaesth. 2021;127(5):760-768. PMID: 34301400.
- Sun Z, Sessler DI, Dalton JE, et al. Postoperative hypoxemia is common and persistent: a prospective blinded observational study. Anesth Analg. 2015;121:709–715.PMID: 26287299.
- Khanna AK, O’Connell NS, Ahuja S, et al. Incidence, severity and detection of blood pressure and heart rate perturbations in postoperative ward patients after noncardiac surgery. J Clin Anesth. 2023;89:111159. PMID: 37295123.
- Sessler DI, Khanna AK. Perioperative myocardial injury and the contribution of hypotension. Intensive Care Med. 2018;44:811–822. PMID: 29868971.
- Liem VGB, Hoeks SE, Mol KHJM, et al. Postoperative hypotension after noncardiac surgery and the association with myocardial injury. Anesthesiology. 2020;133:510–522. PMID: 32487822.
- Khanna AK, Bergese SD, Jungquist CR, et al. PRediction of Opioid-induced respiratory Depression on Inpatient wards using continuous capnoGraphY and Oximetry: an international prospective, observational trial (PRODIGY). Anesth Analg. 2020;131:1012–1024. PMID: 32925318.
- Morrison LJ, Neumar RW, Zimmerman JL, et al. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation. 2013;127:1538–1563. PMID: 23479672.
- Lee LA, Caplan RA, Stephens LS, et al. Postoperative opioid-induced respiratory depression: a closed claims analysis. Anesthesiology. 2015;122:659–665. PMID: 25536092.
- Taenzer AH, Pyke JB, McGrath SP, Blike GT. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010;112:282–287. PMID: 20098128.
- Brown H, Terrence J, Vasquez P, et al. Continuous monitoring in an inpatient medical-surgical unit: a controlled clinical trial. Am J Med. 2014;127:226–232. PMID: 24342543.
- Eddahchouri Y, Peelen RV, Koeneman M, et al. Effect of continuous wireless vital sign monitoring on unplanned ICU admissions and rapid response team calls: a before-and-after study. Br J Anaesth. 2022;128:857–863. PMID: 35282866.
- Weller RS, Foard KL, Harwood TN. Evaluation of a wireless, portable, wearable multi-parameter vital signs monitor in hospitalized neurological and neurosurgical patients. J Clin Monit Comput. 2018;32:945–951. PMID: 29214598.
- Rowland B, Motamedi V, Michard F, et al. Impact of continuous and wireless monitoring of vital signs on clinical outcomes: a propensity matched study in 34,636 surgical ward patients. Br J Anaesth. 2023. (accepted for publication)
- Turan A, Khanna AK, Brooker J, et al. Association between mobilization and composite postoperative complications following major elective surgery. JAMA Surg. 2023;158:825–830. PMID: 37256591.
- Khanna AK, Ahuja S, Weller RS, et al. Postoperative ward monitoring—why and what now? Best Pract Res Clin Anaesthesiol. 2019;33:229–245. PMID: 31582102.
- Greenwald S, Chamoun GF, Chamoun NG, et al. Risk stratification index 3.0, a broad set of models for predicting adverse events during and after hospital admission. Anesthesiology. 2022;137:673–686. PMID: 36129680.


 Issue PDF
Issue PDF PDF
PDF