2017 APSF/ASA Ellison C. Pierce, Jr., MD, Patient Safety Memorial Lecture: Anesthesia Patient Safety: Closing the Gap Between Perception and Reality
Robert K. Stoelting, MD, Past President, APSF

Dr. Robert Stoelting, Past President of the APSF, giving the APSF/ASA Ellison C. Pierce, Jr., MD, Patient Safety Memorial Lecture, entitled “Anesthesia Patient Safety: Closing the Gap Between Perception and Reality,” at the 2017 ASA Annual Meeting in Boston, MA.

Figure 1: Ellison C. Pierce, Jr., MD, founding President of APSF.
The APSF/ASA Ellison C. Pierce Patient Safety Memorial lecture is dedicated to recognizing the contributions to anesthesia patient safety of Ellison C. Pierce, Jr., MD, the founding president of the Anesthesia Patient Safety Foundation (APSF) in 1985 (Figure 1). The APSF is a proud example of anesthesia’s contributions to medicine and the history of APSF’s formation deserves to be part of the heritage for all anesthesia professionals.
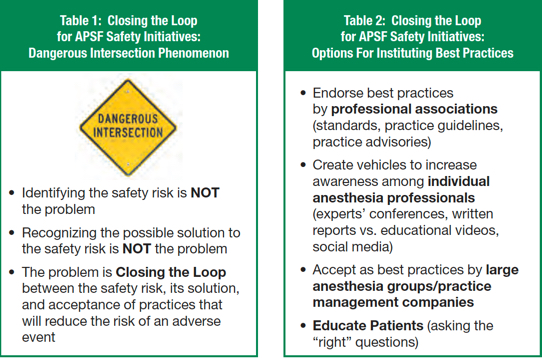
A challenge in addressing anesthesia patient safety issues is closing the gap between what we know (perception and recognition of the safety issue) and the institution of best practices (change in behavior, investment in technology) that will decrease the likelihood of adverse events (reality). Too often the “dangerous intersection” phenomenon persists where the risk of an adverse event is recognized (e.g., flash fire in at-risk patients, opioid-induced ventilator impairment in patients receiving opioids), but the steps for creating a safer intersection (limited open delivery of supplemental oxygen, objective monitoring of oxygenation in the postoperative period) do not occur until after the adverse event (Table 1).
Closing the loop on identified patient safety issues is reflected by changes in behavior and/or investment in technology that facilitates institution of best practices that should predictably decrease the likelihood of an adverse event. This goal may be approached by different paths based on the unique needs, resources, and patient population of each anesthetic practice (Table 2). Endorsement as best practice by anesthesia professional associations in the form of standards, practice guidelines, and practice advisories is a traditional approach and one in which our professional associations have been recognized as leaders by organized medicine.
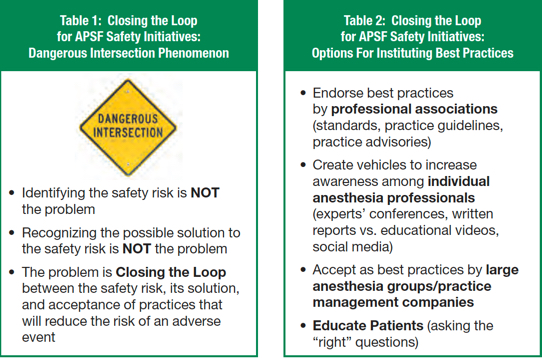
In addition to statements from professional anesthesia associations, an effective approach to bringing best practices to everyday patient care could be endorsement by individual anesthesia groups and practice management companies (Table 2). For example, objective monitoring of neuromuscular blockade could become a “policy” for all members of a group independent of personal views on the need for this strategy. The reality of leaving a safety intervention to individual choice is no longer reasonable. Alternatively, a policy for monitoring neuromuscular blockade would not be relevant for a practice profile that did not include patients routinely receiving neuromuscular blocking drugs.
Ultimately, closing the gap between perception and reality for instituting best practices that will most likely decrease the likelihood of adverse anesthesia events depends on the individual anesthesia professional’s “buy-in” to known safety practices and recommendations. “Only you can help (Figure 2).”
Dr. Stoelting is immediate Past President of the APSF.
He has no disclosures as it relates to this article.




 Issue PDF
Issue PDF