INTRODUCTION
The Society of Anesthesia and Sleep Medicine (SASM) was founded in 2010 as a collaboration between anesthesia professionals and sleep specialists focused on the perioperative safety of patients with sleep disorders. Obstructive sleep apnea (OSA) is one of the sleep disorders that has become recognized as a risk factor for perioperative complications.1,2 SASM has been involved in research and education in the management of patients with OSA and at high risk of undiagnosed OSA in the perioperative period, including development of guidelines to address provision of safe care.3-5 Other sleep disturbances can impact provision of optimal care in the perioperative period, and SASM continues to work to identify and address knowledge gaps of providers to help optimize patient outcomes.3-7
SASM continues to work to identify ongoing needs for education and further research, in addition to utilizing the expertise of sleep specialists and anesthesia professionals to provide guidance in preventing and detecting adverse events in the perioperative period (Figure 1).
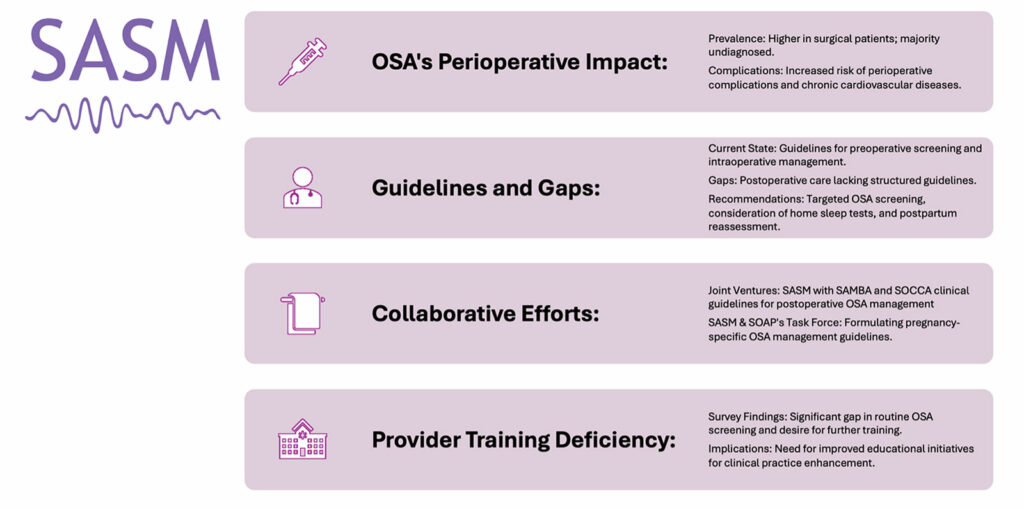
Figure 1: Heeding the “Don’t Look Up'” Call—Society of Anesthesia and Sleep Medicine Leadership, and Collaborative approach to Perioperative Sleep Health Research, and Innovation.
SAMBA: Society for Ambulatory Anesthesia; SASM: Society of Anesthesia and Sleep Medicine; SOAP: Society for Obstetric Anesthesia and Perinatology; SOCCA: Society of Critical Care Anesthesiologists.
POSTOPERATIVE MANAGEMENT, AND CLINICAL GUIDELINES
SASM Creating Guidelines of Postoperative Management For OSA Patients
Obstructive sleep apnea (OSA), a prevalent sleep-related breathing disorder in perioperative environments, is characterized by repeated upper airway collapses that may lead to reduced oxygen saturation during sleep and a heightened risk of chronic cardiovascular diseases.8 The surgical population exhibits a higher frequency of OSA compared to the general population.9 In a retrospective nested cohort study, 819 surgical patients underwent either laboratory or portable polysomnography (PSG). Clinical diagnosis of OSA was determined through chart reviews conducted by surgeons and anesthesia professionals who were blinded to the PSG results. Among the 267 patients identified with moderate-to-severe OSA prior to surgery, 92% (n=245) had not been diagnosed by surgeons, and 60% (n=159) remained undiagnosed by anesthesia professonals.10 This condition is linked to increased perioperative complications2 and consequently, increased hospital and resource utilization.11-14
Although guidelines for preoperative screening3 and intraoperative management4 of OSA patients have been disseminated, a gap persists in evidence-based directives for postoperative care. The development of an evidence-based system for triaging patients with confirmed or suspected OSA is critical when they are admitted post-surgery to ensure the judicious allocation of resources for the management and enhancement of OSA. Moreover, the post-discharge counseling for patients lacks clarity, necessitating evidence-based guidelines established in partnership with patient advocates. Such guidelines are crucial for those undergoing ambulatory surgery, who return home on the same day of the operation, often while under opioid analgesia. Moreover, a significant portion of inpatients, who are initially under close observation in the Post Anesthesia Care Unit (PACU) and Intensive Care Unit (ICU), are later transferred to general care floors where monitoring might not be sufficient for the early detection of vital ventilatory changes.15
To bridge these knowledge gaps, the Society of Anesthesia and Sleep Medicine (SASM) has embarked on a joint venture with the Society for Ambulatory Anesthesia (SAMBA) and the Society of Critical Care Anesthesiologists (SOCCA), aiming to establish evidence-based guidelines for the postoperative management of OSA patients. This initiative aims to augment the SASM’s evidence-informed recommendations for preoperative3 and intraoperative4 management of OSA, along with the SAMBA’s consensus for the ambulatory management of such patients.16 The collaborative guidelines task force is working on recommendations for risk stratification and identification of OSA, postoperative analgesia regimen, postoperative OSA treatment options, monitoring standards, and postoperative discharge considerations, including patient counseling.
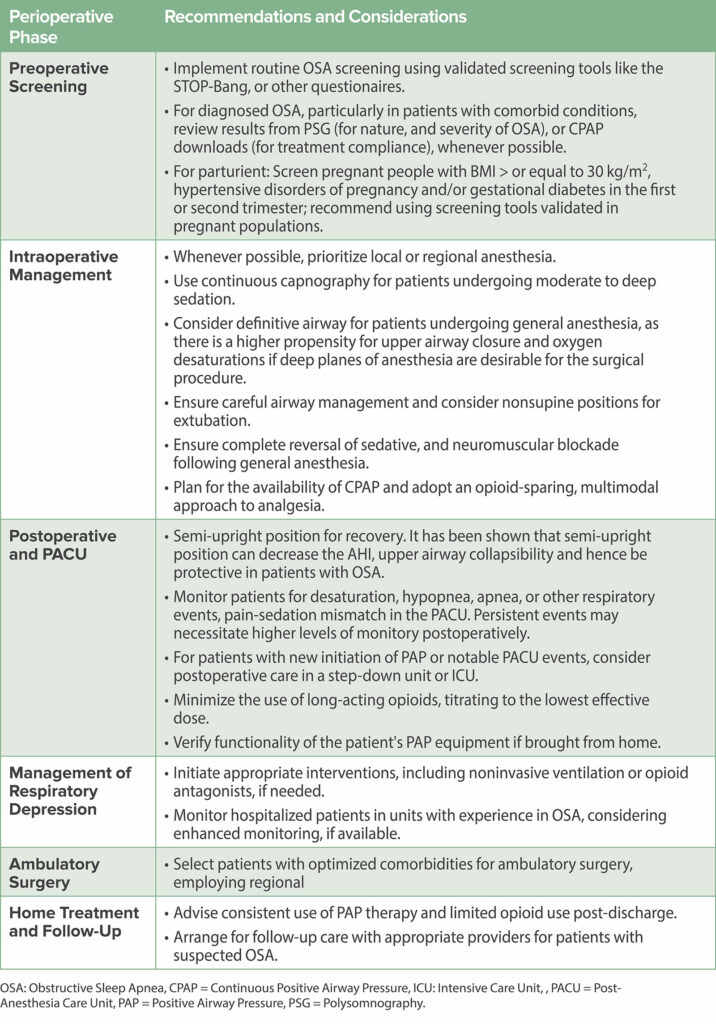
In alignment with our mission to foster collaborative, evidence-based perioperative care, SASM offers expert opinion-based recommendations for managing patients with OSA that provide a continuum of strategies from preoperative screening to postoperative follow-up17 (Table 1).
Table 1: Perioperative Management Strategies for Patients with Obstructive Sleep Apnea.17
PROVIDER KNOWLEDGE ON OSA MANAGEMENT
Assessing the awareness and practices concerning OSA among health care professionals, SASM, with the support of the American Academy of Sleep Medicine Foundation (AASM), led a multisite survey. This extensive study canvassed nine prominent academic institutions and spanned physicians in training and Advanced Practice Providers (APPs) in the fields of Anesthesiology, Internal Medicine, Family Medicine, Surgery, and Obstetrics and Gynecology (OB/GYN), bringing invaluable insights into OSA’s perioperative management.18 Both physicians-in-training and APPs reported that they did not feel their training regarding OSA was adequate. Only 51% overall with 82% in Anesthesia, 34% in Surgery, and 12% in Ob/Gyn reported they felt adequately trained. Across all specialties, 77% desired additional training. When asked about training to assess for OSA in the perioperative period, only 38% of all participants reported feeling that they had been adequately trained. This included 84% in Anesthesia, 33% in Surgery and 15% in OB/Gyn. This opportunity to improve clinical practice was reflected in the participants’ perception of their training .
CLINICAL GUIDELINES FOR MANAGEMENT OF OBSTETRIC PATIENTS WITH OSA
Maternal Morbidity is Associated with OSA
Recent studies have highlighted the maternal morbidity associated with OSA; it has been particularly associated with hypertensive disorders of pregnancy and gestational diabetes mellitus.19-23 The correlation of maternal OSA with neonatal outcomes such as pre-term birth, Apgar scores, and low birth weight, however, remains contentious.24-27 Pregnancy is a dynamic state during which physiologic changes and weight gain, along with pathophysiologic changes related to conditions such as preeclampsia present unique challenges for clinicians in the screening, diagnosis, and management of OSA that had not been addressed in the available literature. Thus, SASM and the Society for Obstetric Anesthesia and Perinatology (SOAP) assembled a task force of experts to review the available evidence and generate recommendations on the screening, diagnosis, and treatment of patients with OSA during pregnancy including expert opinion where evidence was lacking. The multidisciplinary committee was composed of anesthesia professionals, sleep medicine specialists and research scientists, maternal fetal medicine specialists, and a research librarian. These recommendations were published in Obstetrics and Gynecology in August 2023 (https://journals.lww.com/greenjournal/abstract/2023/08000/society_of_anesthesia_and_sleep_medicine_and_the.22.aspx).28
The guidelines do not recommend screening all pregnant people for OSA, but do suggest screening those people with pre-existing risk factors for OSA including BMI > 30 kg/m2; hypertensive disorders of pregnancy; and/or gestational diabetes in the index or prior pregnancy. The recommended timing of screening is between 6–29 weeks’ gestation. The Guideline committee reviewed several OSA screening tools that had been studied in pregnant populations and suggest that screening tools that have been validated in pregnant cohorts are the most promising for predicting OSA in this population. Recommendations regarding the diagnosis of OSA in parturients focus on considering home sleep tests when appropriate, as well as considering repeat postpartum testing due to the dynamic airway changes that occur during and after pregnancy. Treatment guidance emphasizes the lack of evidence that OSA treatment modulates any pregnancy-specific outcomes, but that OSA treatment is still indicated in pregnancy to treat symptoms, modify objective measures of OSA, and to improve quality of life. These are the first guidelines to address specific considerations for OSA management in those that are pregnant.
CONCLUSION
The integration of the SASM’s comprehensive approach across the continuum of OSA management—from preoperative assessment to postoperative and long-term care—underscores the necessity of a multifaceted strategy. The article has provided a cohesive narrative that aligns with the Society’s overarching goal of improving patient safety and outcomes in anesthesia and sleep medicine.
Mandeep Singh, MD, is an associate professor of anesthesiology at the University of Toronto, Toronto, Canada.
Jennifer Dominguez, MD, is an associate professor of anesthesiology at Duke University, Durham, North Carolina.
Melanie Lyons, PhD, ACNP, is an adjunct assistant professor, University of Pennsylvania School of Nursing, Philadelphia, PA.
Satya Krishna Ramachandran, MD, MBA, is an associate professor of anesthesiology, Beth Israel Deaconess Medical Center, Harvard University, Boston, MA.
Bhargavi Gali, MD, MHA, is an associate professor of anesthesiology and perioperative medicine at Mayo Clinic, Rochester, MN.
Mandeep Singh, MD, Jennifer Dominguez, MD, and Melanie Lyons, PhD, ACNP, have no conflicts of interest. Satya Krishna Ramachandran, MD, MBA, has received honoraria and research funding from Fresnius Kabi USA. Bhargavi Gali, MD, MBA, is a data monitoring committee member for Takeda.
REFERENCES
- Gupta RM, Parvizi J, Hanssen AD, Gay PC. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. Mayo Clin Proc. 2001;76:897–905. PMID: 11560300.
- Opperer M, Cozowicz C, Bugada D, et al. Does obstructive sleep apnea influence perioperative outcome? a qualitative systematic review for the Society of Anesthesia and Sleep Medicine Task Force on preoperative preparation of patients with sleep-disordered breathing. Anesth Analg. 2016;122:1321–1334. PMID: 27101493.
- Chung F, Memtsoudis S, Krishna Ramachandran S, et al. Society of Anesthesia and Sleep Medicine guideline on preoperative screening and assessment of patients with obstructive sleep apnea. Anesth Analg. 2016;123:452–473. PMID: 27442772.
- Memtsoudis SG, Cozowicz C, Nagappa M, et al. Society of Anesthesia and Sleep Medicine guideline on intraoperative management of adult patients with obstructive sleep apnea. Anesth Analg. 2018;127:967–987. PMID: 29944522.
- Hillman DR, Carlucci M, Charchaflieh JG, et al. Society of Anesthesia and Sleep Medicine position paper on patient sleep during hospitalization. Anesth Analg. 2023;136:814–824. PMID: 36745563.
- Sibley D, Sellers D, Randall I, et al. Evaluating the effect of preoperative interventions on sleep health in the perioperative period: a systematic review. J Sleep Res. December 2023. PMID: 38124447.
- Butris N, Tang E, Pivetta B, et al. The prevalence and risk factors of sleep disturbances in surgical patients: a systematic review and meta-analysis. Sleep Med Rev. 2023;69:101786. PMID: 37121133.
- Peppard PE, Hagen EW. The last 25 years of obstructive sleep apnea epidemiology—and the next 25? Am J Respir Crit Care Med. 2018;197:310–312. PMID: 29035088.
- Memtsoudis SG, Besculides MC, Mazumdar M. A rude awakening—the perioperative sleep apnea epidemic. N Engl J Med. 2013;368:2352–2353. PMID: 23782177.
- Singh M, Liao P, Kobah S, et al. Proportion of surgical patients with undiagnosed obstructive sleep apnoea. Br J Anaesth. 2013;110:629–636. PMID: 23257990.
- Kaw R, Chung F, Pasupuleti V, et al. Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br J Anaesth. 2012;109:897–906. PMID: 35231774.
- Bolden N, Posner KL, Domino KB, et al. Postoperative critical events associated with obstructive sleep apnea: results from the Society of Anesthesia and Sleep Medicine Obstructive Sleep Apnea Registry. Anesth Analg. 2020;131:1032–1041. PMID: 32925320.
- Memtsoudis SG, Stundner O, Rasul R, et al. The impact of sleep apnea on postoperative utilization of resources and adverse outcomes. Anesth Analg. 2014;118:407–418. PMID: 24445639.
- Chan MTV, Wang CY, Seet E, et al. Association of unrecognized obstructive sleep apnea with postoperative cardiovascular events in patients undergoing major noncardiac surgery. JAMA. 2019;321:1788–1798. PMID: 31087023.
- Khanna AK, Hoppe P, Saugel B. Automated continuous noninvasive ward monitoring: future directions and challenges. Crit Care. 2019;23:194. PMID: 31146792.
- Joshi GP, Ankichetty SP, Gan TJ, Chung F. Society for Ambulatory Anesthesia consensus statement on preoperative selection of adult patients with obstructive sleep apnea scheduled for ambulatory surgery. Anesth Analg. 2012;115:1060–1068. PMID: 22886843.
- Cloward T, and the SASM Clinical Committee. Recommendations for the perioperative evaluation and management of patients with sleep apnea. Educational Resources. Society of Anesthesia and Sleep Medicine. https://sasmhq.org/docs/SASM_GuidelinesRecommendations_EDIT120716.pdf. Accessed April 2024.
- Lyons MM, Gali B, Auckley D, et al. Perceptions of the need for perioperative OSA education: an interdisciplinary and multi-institutional survey. Sleep. 2022;45:A163–A164. doi.org/10.1093/sleep/zsac079.360.
- Facco FL, Parker CB, Reddy UM, et al. Association between sleep-disordered breathing and hypertensive disorders of pregnancy and gestational diabetes mellitus. Obstet Gynecol. 2017;129:31–41. PMID: 27926645.
- Yang Z, Zhu Z, Wang C, et al. Association between adverse perinatal outcomes and sleep disturbances during pregnancy: a systematic review and meta-analysis. J Matern Neonatal Med. 2022;35:166–174. PMID: 31902261.
- Bourjeily G, Danilack VA, Bublitz MH, et al. Obstructive sleep apnea in pregnancy is associated with adverse maternal outcomes: a national cohort. Sleep Med. 2017;38:50–57. PMID: 29031756.
- Bourjeily G, Danilack VA, Bublitz MH, et al. Maternal obstructive sleep apnea and neonatal birth outcomes in a population based sample. Sleep Med. 2020;66:233–240. PMID: 31981755.
- Louis JM, Mogos MF, Salemi JL, et al. Obstructive sleep apnea and severe maternal-infant morbidity/mortality in the United States, 1998–2009. Sleep. 2014;37:843–849. PMID: 24790262.
- Ding X-X, Wu Y-L, Xu S-J, et al. A systematic review and quantitative assessment of sleep-disordered breathing during pregnancy and perinatal outcomes. Sleep Breath. 2014;18:703–713. PMID: 24519711.
- Bin YS, Cistulli PA, Ford JB. Population-based study of sleep apnea in pregnancy and maternal and infant outcomes. J Clin Sleep Med. 2016;12:871–877. PMID: 27070246.
- Chen Y-H, Kang J-H, Lin C-C, et al. Obstructive sleep apnea and the risk of adverse pregnancy outcomes. Am J Obstet Gynecol. 2012;206:136.e1-136.e5. PMID: 29031756.
- Liu L, Su G, Wang S, Zhu B. The prevalence of obstructive sleep apnea and its association with pregnancy-related health outcomes: a systematic review and meta-analysis. Sleep Breath. 2019;23:399–412. PMID: 30255484.
- Dominguez JE, Cantrell S, Habib AS, et al. Society of Anesthesia and Sleep Medicine and the Society for Obstetric Anesthesia and Perinatology consensus guideline on the screening, diagnosis, and treatment of obstructive sleep apnea in pregnancy. Obstet Gynecol. 2023;142:403–423. PMID: 37411038.


 Issue PDF
Issue PDF PDF
PDF