In 2009 SENSAR started the first multicentre Critical Incident Reporting System in Spain. Ten years later, it accounts for 107 actively participating hospitals in Spain and Chile, with more than 500 local analyzers, over 9,000 critical incidents reported resulting in more than 17,000 improvement measures implemented. This article describes SENSAR’s impact on improving safety culture and patient safety, illustrating the benefits of using a multimodal strategy within healthcare organizations.
INTRODUCTION
A Critical Incident Reporting System (CIRS) collects events or circumstances that may result in unnecessary harm to patients. It is a highly useful tool for the improvement of patient safety (PS), as it prevents avoidable harm by performing a systematic analysis of the latent factors (LF) contributing to adverse events. Several organizations such as the World Health Organization (WHO) and the Agency for Healthcare Research and Quality (AHRQ) recommend the use of CIRS. Their use is founded on the modern principles of a non-punitive, open, fair and learning culture of safety (CS) and require the commitment of individuals and organizations to potentially reduce patient harm in anesthesia practice. National CIRS’s have been demonstrated to be essential elements for increasing CS.1 The most useful CIRS are those which are anonymous and voluntary, focus on learning and employ a national scope. These features facilitate the creation of local solutions to widespread problems through the adoption and execution of improvement measures (IM) designed to prevent critical incidents from recurring.2,3 A lack of potential reach of existing CIRS’s in reducing patient harm as expected by the WHO4 has been attributed to some known limitations and barriers including a lack of feedback to the professionals reporting incidents, challenges in measuring rates of adverse events, the associated costs of implementation, lack of institutional and economic support, poor implementation, as well as the challenges of analyzing the large volumes of information obtained by the systems. Despite the fact that several initiatives have been launched to increase their use,5 the potential of CIRS for promoting PS has not been fully realized.
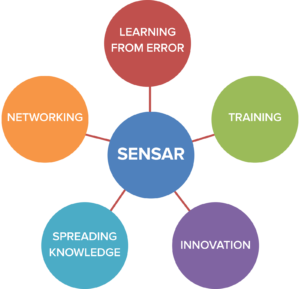
The Spanish Anesthesia and Recovery Safety Notification System (SENSAR, by its Spanish acronym) is a CIRS created in 2009 with the participation of 16 hospitals throughout Spain. It evolved from a single center system implemented in 1999 within the Hospital Universatario Fundación Alcorcón. Five years later the CIRS was enhanced with a multimodal strategy (MMS) to improve its performance in critical incident reporting, analysis and the execution of derived IM (Figure 1). After ten years of experience, SENSAR has expanded to include 107 hospitals (100 in Spain, 7 in Chile), consisting of more than 500 analyzers, who have examined 9,274 reports of critical incidents and implemented 17,056 improvement measures (Table 1). Over time, what started as a single center CIRS, has been transformed into an organization that serves as a model for improving perioperative patient safety throughout Spain, Europe, and Latin America.
Table 1: Number of Hospitals, Analyzers, Critical Incidents, and Improvement Measures During 10 Years of SENSAR´s Experience.
| Hospitals | Analyzers | Critical Incidents | Improvement Measures | |
| 2009 | 37 | 183 | 575 | 1024 |
| 2010 | 53 | 246 | 1438 | 2570 |
| 2011 | 63 | 288 | 2184 | 3914 |
| 2012 | 69 | 304 | 2785 | 5190 |
| 2013 | 75 | 335 | 3568 | 6470 |
| 2014 | 77 | 351 | 4714 | 8662 |
| 2015 | 78 | 356 | 5993 | 10930 |
| 2016 | 90 | 425 | 7170 | 13256 |
| 2017 | 101 | 484 | 8352 | 15596 |
| 2018 | 107 | 518 | 9392 | 17722 |
AN OVERVIEW OF OUR CIRS
SENSAR’s CIRS is a non-punitive, anonymous and confidential learning tool that provides agility in the management of the information received, by providing immediate feedback in the form of actionable IMs. It also promotes data sharing at a national level, as it is managed by groups of local PS experts who share their data and educational projects through professional networks and communities.
Patient safety is an essential measure of quality of care and risk management. In recent years, we have directed efforts toward developing and measuring the CS throughout our organizations, which thereby allows a wider range of action, resulting in a greater impact derived from the IMs employed. This cultural change involves a process of collective learning that focuses on the system, and not on the individual. It is based on understanding the causes of CIs in order to adopt measures that will be able to prevent them. Reason’s model of human error, which is widely accepted, serves as a foundation for the system.6 This model acknowledges that human beings are fallible and that mistakes made by individuals are therefore expected. However, these human errors must be seen as consequences and not as causes, since they originate from factors within the health care system. Therefore, individuals not only have to avoid making errors, but, in addition, the health care systems should have protective measures in place to prevent them. Employing this approach, each CI is a learning opportunity to identify and correct the contributing factors, and not a situation to blame the individual involved in making the error. The following four cultutral elements are important for achieving a PS culture: 1) Communication, in which health care providers perceive a nonpunitive atmosphere, which encourages the reporting of CIs and allows them to speak freely about them with others; 2) Justice, in which unacceptable and dangerous behavior is clearly differentiated from behavior that, although erroneous, is understandable or explainable; 3) Flexibility, which allows changes in the hierarchical structure to adapt to risk situations; and 4) Learning, with the desire to gain insight from the analysis of CIs and the willingness to implement necessary modifications.7
OUR APPROACH
SENSAR’s approach focuses on analyzing CIs using a framework to identify the associated latent factors, among which we consider: 1) the individual (anesthesia professional or other health care provider) in direct contact with the patient; 2) the team of professionals involved with the CIs, as well as the communication between them; 3) the task(s) being performed; 4) the patient, which includes his or her clinical condition; 5) the workplace; and 6) the organization. SENSAR facilitates learning from errors systematically, and thereby helps to promote safety in the health care environment, by providing a vehicle by which to analyze incidents without damage to the patient. We believe that studying and controlling latent factors is not only key to performance improvement, but also the most effective way to prevent CIs from reoccurring.
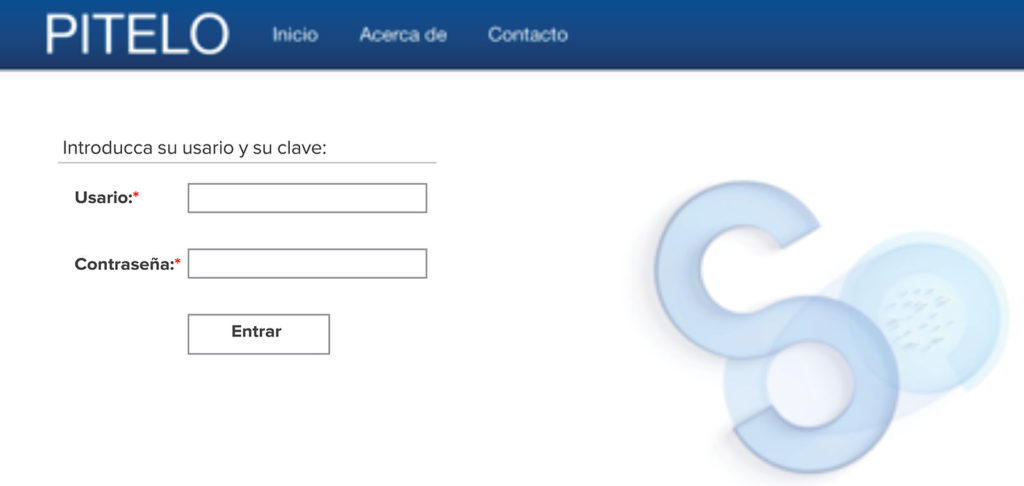
The reporting of CIs within SENSAR’s 107 member hospital collaborative occurs through an electronic form with generic access codes, unique for each center (Figure 2). Our system uses an online platform, called PITELO (an acronym for the most common latent factors Patient –Individual–Task–tEam–pLace–Organization), which is accessed through its website (www.sensar.org). The communication form is structured to facilitate the introduction of the data and avoid the loss of relevant information. (Between 2009 and April 2017 SENSAR’s CIRS was known as ANESTIC.)
The CIs of each hospital reported in SENSAR’s database are available to the local analysis group. This analysis group is composed of a minimum of three to a maximum of six anesthesia professionals; and usually includes the head or chief of staff, as a way to facilitate and expedite the implementation of IMs if needed. Each member of the analysis group assumes responsibility for the CIs reported during a designated period of time (weekly or monthly depending on the volume of communications) and acts as the “speaker” for the rest of the group. His or her function includes the comprehensive review of each incident during the assigned interval, erasure of all identifying information contained that would prevent anonymity (proper names, dates, clinical history numbers, etc.), review of the hospital’s individual database for similar CIs (as well as the database from other hospitals contributing to SENSAR if available). The analysis performed is focused on the system to determine the latent factors contributing to the occurrence of the CI, and results in the proposal of corrective measures that address each of the latent factors identified.
OUR RESULTS AFTER TEN YEARS
SENSAR has grown from its original sixteen members, to a network of 100 hospitals in Spain, and 7 hospitals in Chile. It contains more than 9,000 incidents in its database, and includes almost twice as many proposed IMs for preventing future adverse events. Despite this success, greater efforts are needed in order to keep up with the current implementation and allow for further growth. Among the biggest challenges in ongoing efforts is motivating health care providers to report CIs.
Regarding the nature of the CIs reported to the SENSAR database, clinical errors were the most common incidents reported (25%), followed by medication errors (21%) and equipment malfunction (20%). Fortunately, less than five percent of the incidents reported in our database posed a lethal threat to the patient involved. Importantly, SENSAR, allows us to learn from and develop useful IMs from incidents posing low, intermediate, or high risk to patients. Measures derived from our analysis have varied in complexity. The majority of the IMs in our database tend to be educational or informative, i.e., alerts, communications, clinical sessions, or debriefings, for staff members designed to help providers avoid factors that lead to the CI; 1,568 clinical protocols have been created or modified among our 107 member hospitals as a result of the analysis. In order to make our system sustainable and as part of our “Spreading the knowledge” MMS, we have been able to implement PS courses focused on CIRS at a local, national, and international scale (Chile); training more than 450 professionals in Spain and over 180 in Chile.
We believe the anesthesia professional is evolving towards a safer practitioner by following this system. The impact of the developed MMS utilized by SENSAR has resulted in a meaningful advancement in the field of anesthesia PS and related areas, enhancing the CS of professionals and institutions. SENSAR might serve as a model for enhancing patient safety more globally.
Dr. Alejandro Garrido Sánchez is an anesthesiologist at the Hospital General Universitario Gregorio Marañón and vice president of SENSAR, Madrid, Spain.
Dr. Rodrigo Molina Mendoza is an anesthesiologist at the Hospital Universitario Fundación Alcorcón and treasurer of SENSAR, Madrid, Spain.
Dr. Eva Romero García is an anesthesiologist at the Hospital Universitario y Politécnico La Fe, and president of SENSAR, Valencia, Spain.
Dr. Daniel Arnal Velasco is an anesthesiologist at the Hospital Universitario Fundación Alcorcón, and chairman of the ESA (European Society of Anesthesia) Patient Safety and Quality Committee, Madrid, Spain.
The authors have no conflict of interest pertaining to this article. SENSAR is a non-profit and public advantage organization.
NOTE: Tables and figures are original from SENSAR.
REFERENCES
- Hutchinson A, Young TA, Cooper KL, et al. Trends in health care incident reporting and relationship to safety and quality data in acute hospitals: results from the National Reporting and Learning System. BMJ Publishing Group Ltd. Quality and Safety in Health Care. 2009;18:5–10.
- Reed S, Arnal D, Frank O, et al. National critical incident reporting systems relevant to anaesthesia: a European survey. Br J Anaesth. 2014;112:546–55.
- Howell A-M, Burns EM, Hull L, et al. International recommendations for national patient safety incident reporting systems: an expert Delphi consensus-building process. BMJ Publishing Group Ltd. BMJ Qual Saf. 2017;26:150–63.
- Mitchell I, Schuster A, Smith K, et al. Patient safety incident reporting: a qualitative study of thoughts and perceptions of experts 15 years after “To Err is Human.” BMJ Qual Saf. 2016;25:92–9.
- Parmelli E, Flodgren G, Fraser SG, et al. Interventions to increase clinical incident reporting in health care. Cochrane Database Syst Rev. 2012;(8):CD005609.
- Reason J. Human error: models and management. BMJ. 2000;320:768-70.
- Mahajan, RP. Safety culture in anesthesiology. Revista Española de Anestesiología y Reanimación. 2011;58 (Supl.3): S10-S14.


 Issue PDF
Issue PDF