Dear Rapid Response:
A little more than a year ago, I was on-call at a mid-sized Florida community hospital. The facility was building a new wing for interventional procedures that was almost completed.
That day, three operating rooms (ORs) were running simultaneously and suddenly a “code blue” was called in one of the ORs, where a colovesicular fistula repair was finishing. I entered the room to see that CPR was underway. The anesthesia professional in the room explained that, during skin closure, he had “trouble ventilating.” He attempted manual ventilation with 100% oxygen, but the patient became bradycardic and then developed asystole. Our anesthesia care team administered one milligram of epinephrine and atropine while CPR was underway and achieved return of spontaneous circulation with an adequate blood pressure. Just then, a nurse contacted me to come to the second OR immediately. Since vital signs were stable and ventilation seemed normal at that point with normal SpO2, I left the first patient in the care of the surgeon and anesthesia professional.
I entered the second OR and the anesthesia professional in that room explained that the patient abruptly became hypoxic and then bradycardic despite being ventilated with oxygen alone. As I began to help troubleshoot, I was called emergently to the third OR. Another anesthesia professional helped resuscitaiton efforts in OR 2.
Entering the hallway, I noticed the oxygen manifold high-pressure alarm was emitting a loud noise indicating high pressure at 75 psig.
When I arrived in the third room, the anesthesia professional was ventilating that patient using a bag-valve-mask device connected to a portable oxygen E-cylinder. She stated that there was a “problem with the anesthesia machine,” and she felt most comfortable using the independent oxygen source for ventilation until help could arrive. I quickly checked the anesthesia machine in that room and found it fully functional. Still concerned about the central gas supply, I disconnected the machine from the wall oxygen source and continued the case using the cylinder supply. At that point, I hypothesized that a nitrogen source connected to the oxygen manifold could explain the findings in all three ORs. As a former nuclear engineer, I was familiar with pipe testing and errors due to incorrect valve line-ups.
Fortunately, there were no sequelae for any of the patients. However, one of the patients remained intubated and was transferred to the ICU. The ICU (one floor above the new OR) shared the same medical gas system, and therefore, I alerted the ICU staff to use only portable oxygen cylinders until the problem had been completely resolved. Our chief of medical staff and chair of surgery, along with our chief executive officer, all decided to close the ORs until the problem was evaluated and rectified. The ICU continued to operate on portable oxygen cylinders but, in the interim, planned to transfer any new ICU admissions to a sister hospital several miles away.
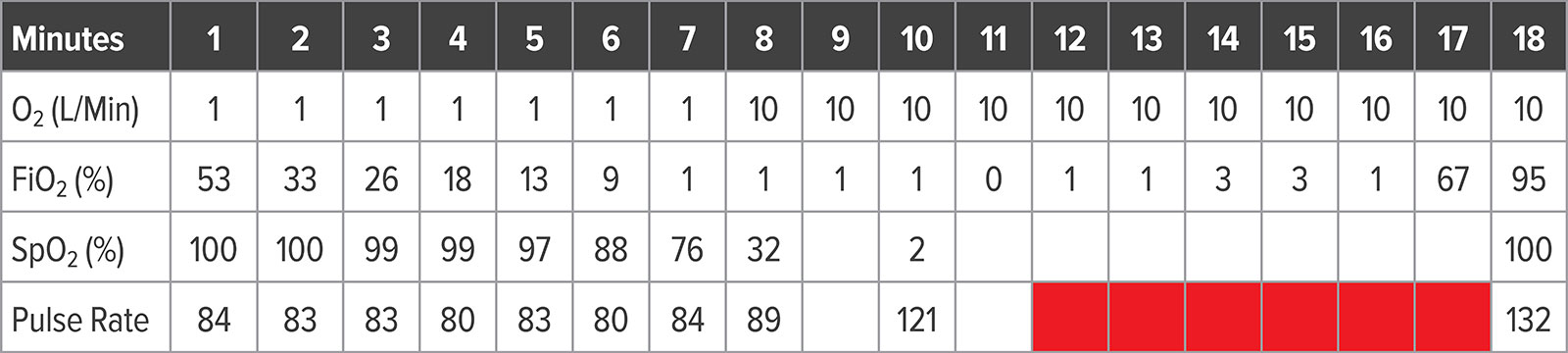
Analysis of the electronic medical record data revealed a 10-minute period where the O2 concentration dropped below 10% despite delivering “only oxygen” at 10 liters per minute (Table 1). During most of that period, the oxygen concentration was essentially 0%. When data were evaluated for each OR chronologically, it appeared that a bolus of nitrogen was introduced into the oxygen piping and traveled from room to room until it was washed out by oxygen flow. Each room dropped oxygen concentration about two minutes apart sequentially along the piping run.
Table 1: Data From Anesthesia Record System in One Affected OR
The hospital facilities manager inspected the system with our piping contractor, and next morning the system was deemed fit for use.
A Root Cause Analysis (RCA) was performed and identified the following: Contractors were testing gas piping in a new section of the hospital. Although “proper active system isolation” was in effect, “someone” doing other maintenance work in the area “opened an isolation valve briefly,” which allowed 150 psi nitrogen to displace oxygen in the active piping limb. Hospital Risk Management and the facilities manager stated that the contractor was “fully licensed and trained.”
The RCA report recommended that:
- Future medical gas testing and maintenance shall be done on “off-hours” if possible, and that management will notify all staff about planned testing.
- During any future testing, isolation valves shall be checked, tagged, and locked.
- During future pipe testing, management will allow no other maintenance work in the vicinity of isolation valves or pipe testing equipment.
I hope that this incident will raise awareness about the potential for adverse patient events that can occur during construction and maintenance of medical gas piping systems. I have been unable to locate published reports of a similar incident that have not resulted in death or serious harm to patients. There is a sharp increase planned in community hospital expansion projects over the next few years.1 I fear that, as a result, we may see more of these misadventures nationwide.
Jeffrey M. Gilfor, MD
Director of Anesthesia
Centers for Advanced Surgical Specialists
Tampa, FL
The author has no conflicts of interest pertaining to this article.
Reference
- Burmahl E, Hoppszallen S, Morgan J. 2017 hospital construction survey. Health Facilities Management; 2017. https://www.hfmmagazine.com/articles/2750-hospital-construction-survey Accessed April 22, 2019.
Reply:
Nitrogen Contamination of Oxygen Supply: Prevention and Response
Bulk oxygen delivery systems and medical gas pipelines have the potential to be a serious patient safety hazard. Reports of problems with these systems date back over 50 years. For example, Bancroft and colleagues1 reported 18 major problems with their liquid oxygen delivery system in one year.
The potential problems can involve existing systems as well as new construction. Hazards with existing systems include running out of oxygen, filling the oxygen supply with the wrong gas, and pipeline leaks. Problems with new construction include contamination of the pipeline with debris, crossed gas lines, improper construction of the pipeline and brazing of joints, and improper verification and testing of the new pipeline.
The National Fire Protection Association (NFPA) publishes codes for medical gas supplies under the title “NFPA-99 the Health Care Facilities Code.”2 Chapter 5 (Gas and Vacuum Systems) gives very specific instructions as to what procedures the installer and inspectors must follow during construction. In addition to following the codes, all personnel involved in medical gas pipeline installation must have specific training and certification. The installer must be American Society of Sanitary Engineering (ASSE) 6010 certified. Similarly, the inspector must be ASSE 6020 certified, and the verifier needs to hold an ASSE 6030 certificate. It is important to note that the installer, inspector, and verifier cannot be the same person.
When installing a new medical gas pipeline the contractor must consider two important factors: the code, which tells the installer what to do, and his certification and training, which tells him how to do it. If these rules are followed then mishaps will not occur. First, the installer does an initial purge with nitrogen. This removes debris that has accumulated in the pipeline during construction. Next, the pipeline is pressurized to 150 psi with nitrogen, and every joint is inspected for leaks. The pipeline is then depressurized and tested for cross-connections. Finally, each outlet is purged to remove particulate matter, and a 24-hour “standing pressure test” is completed. The connection to the main system cannot be done until all of the nitrogen testing is completed. Finally, a 6030 verifier shall test all installations.
If an anesthesia practitioner encounters a potential problem with the oxygen supply, what is the proper procedure to follow? The practitioner will first be alerted to a problem by the oxygen analyzer on the anesthesia machine. Events like the one reported by Dr. Gilfor in this issue of the APSF Newsletter underscore the importance of a functioning oxygen monitor with the alarms properly set prior to every anesthetic. If the inspired oxygen concentration falls below 20%, the practitioner should immediately suspect a problem. There are two options to safely care for the patient in this situation. First, the patient can be disconnected from the anesthesia machine and ventilated with a self-inflating bag or Mapleson type circuit and a portable oxygen cylinder. Alternately, the emergency oxygen tank(s) on the machine can be utilized. The anesthesia practitioner must remember that the pressure in the oxygen tanks is reduced to 45 psi, but the pressure in the hospital pipeline is 50-55 psi. A previous report of this same problem noted that turning on the oxygen tanks on the anesthesia machine did not solve the problem due to the pressure in the supply lines.3 Therefore, the hoses from the central supply must be disconnected to insure that oxygen will flow from the tank supply.
Dr. Ehrenwerth is professor emeritus, Yale University School of Medicine, New Haven, CT USA.
The author has no conflicts of interest pertaining to this article.
References
- Bancroft ML, du Moulin GC, Hedley-Whyte J. Hazards of hospital bulk oxygen systems. Anesthesiology 1980; 52:504-510..
- NFPA-99 Health care facilities code, 2018 edition: National Fire Protection Association, Quincy MA.
- It could happen to you! Construction contaminates oxygen pipeline. APSF Newsletter 2012;27:35. https://www.apsf.org/article/it-could-happen-to-you-construction-contaminates-oxygen-pipeline/. Accessed April 8, 2019.
Editor’s Note:
Unfortunately, there is a history of events like this being reported to the APSF.1–3 We will continue to publish these reports as a reminder that nitrogen contamination of oxygen supplies is completely preventable. More importantly, patient injury is completely preventable in this situation, but requires continuous oxygen monitoring, vigilance, and ready access to an alternate supply of oxygen.
Dr. Feldman is chair, APSF Committee on Technology, and professor of Clinical Anesthesiology Children’s Hospital of Philadelphia Perelman School of Medicine, Philadelphia, PA.
Dr. Feldman has received consulting compensation from Micropore, Dräger Medical, GE Medical, and Medtronic.
References
- Anonymous Author. It could happen to you! Construction contaminates oxygen pipelines. APSF Newsletter. 2012;27:35. https://www.apsf.org/article/it-could-happen-to-you-construction-contaminates-oxygen-pipeline/ Accessed April 11, 2019.
- Holland R. Foreign correspondence: “wrong gas” disaster in Hong Kong. APSF Newsletter. 1989;4. https://www.apsf.org/article/foreign-correspondence-wrong-gas-disaster-in-hong-kong/ Accessed April 11, 2019.
- Tirer S, Mahan M. Pipeline pressure primer. APSF Newsletter. 2007;22:38. https://www.apsf.org/article/pipeline-pressure-primer/ Accessed April 11, 2019.
The information provided is for safety-related educational purposes only, and does not constitute medical or legal advice. Individual or group responses are only commentary, provided for purposes of education or discussion, and are neither statements of advice nor the opinions of APSF. It is not the intention of APSF to provide specific medical or legal advice or to endorse any specific views or recommendations in response to the inquiries posted. In no event shall APSF be responsible or liable, directly or indirectly, for any damage or loss caused or alleged to be caused by or in connection with the reliance on any such information.


 Issue PDF
Issue PDF