Non-operating room anesthesia (NORA) comprises an increasing share of modern anesthesia practice. NORA presents setting-specific challenges to safe anesthesia care, but protocols and interdisciplinary teamwork can facilitate safe, efficient, and cost-effective procedural care in the NORA suite.
Introduction
As case volumes increase year after year, Non-Operating Room Anesthesia (NORA) continues to evolve,1 with NORA-based procedures comprising a larger share of modern anesthesia practice than ever before.2 Growth in NORA-based procedures can be attributed to many driving influences, including the advent of less invasive procedures, an aging population with increasing comorbidity burden, the introduction of new technology expanding the indications for and complexity of NORA cases, and the economics of a health care environment that looks to improve value by decreasing costs. With these advances and growth, new demands on the anesthesia team are challenging conventional methods. Increasingly, NORA cases may require more invasive monitoring techniques and deeper levels of sedation that carry the potential for increased patient risk and injury. As Woodward et al. noted, we are seeing an “evolution in patient and procedure complexity in NORA.”3
Closed Claims Data
Examination of closed claims databases provides insight into the potential adverse outcomes and vulnerabilities related to NORA procedures. The majority of NORA closed claims cases originated in the gastrointestinal endoscopy suite.3 This might be related to the sheer volume of cases performed there as compared to other venues.
Patients undergoing NORA procedures, compared to those performed in the operating room, have a higher frequency of severe injury and death.4–6 In more than half of NORA-related claims involving deaths, patients were deemed to have received substandard anesthesia care preventable by improved monitoring techniques.5 Suboptimal care and failure to provide safe practice were seen as the leading cause of poor outcomes.3 Most claims were related to respiratory events, specifically inadequate oxygenation and/or ventilation.5,6 Monitored anesthesia care was the most common anesthetic technique used, contributing to 50% of claims.5 Oversedation leading to respiratory depression was implicated in a third of all claims. In most claims related to oversedation, there was limited use of monitoring expired carbon dioxide or any respiratory monitoring at all.5,6
How Risky is NORA?
Despite intriguing findings from the closed claims work, there remain limited data related to NORA-based outcomes, confounding efforts to mitigate risk and improve safety.5,6 Conventional teaching has been that patients have increased risk with NORA-based procedures compared to those done in the traditional operating room. However, recent findings from the National Anesthesia Clinical Outcomes Registry (NACOR) suggest that NORA-based procedures, as a whole, have a lower rate of complications, morbidity, and mortality compared to traditional operating room procedures.2 Importantly, though, NORA venues may differ in the frequency of adverse events. Specifically, Chang et al. observed a higher incidence of complications and higher mortality in patients undergoing NORA procedures in the cardiology and radiology suites as compared to the operating room or the gastroenterology suite.2 This analysis did not control for differences in age and comorbidity burden, so caution should be taken interpreting the findings.
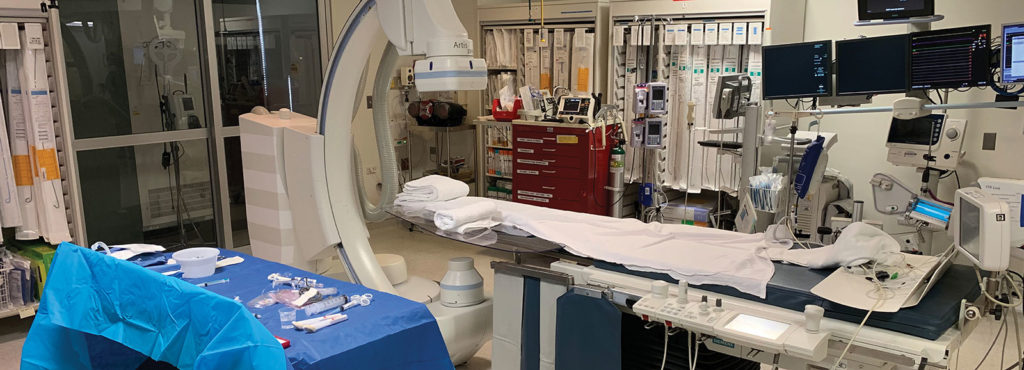
Both NORA-specific and more general procedural issues influence the risk of NORA-based procedures (Table 1). NORA-specific issues are related to concerns within the NORA suite itself, including location and procedure-related challenges. NORA procedures are often performed in crowded rooms with limited patient access. These rooms may not have been originally designed for an anesthetic. They may be retrofitted with outdated anesthesia equipment. They may be small in size with an inadequate power supply and may be equipped with poor lighting. Additional issues to address in NORA procedures are supply lines of equipment (e.g., appropriate monitoring devices) and the adequacy and availability of support staff. NORA cases are also more likely to start after normal working hours compared to the operating room.1 These “off-hour” starts may limit the availability of critical resources and force unfamiliar personnel to assist with the procedure and anesthesia. Also, compared to the traditional operating room, a greater percentage of NORA procedures are being performed on an emergency basis.6 Whether off-hour starts and emergency status translate to poorer patient outcomes is unknown.
Table 1: Challenges to providing safe care in NORA settings
| NORA-specific challenges |
| Remote location far from pharmacy and supplies |
| Noisy environments |
| Limited workspace, small procedure room |
| Inadequate lighting |
| Minimal temperature regulation |
| Electrical / magnetic interference |
| Older, possibly unfamiliar equipment |
| Lack of skilled anesthesia support staff |
| Limited patient access during procedures |
| Inadequate power supply |
| Radiation safety |
| Challenges relevant to NORA and OR anesthesia |
| Supply of equipment |
| Appropriate monitoring devices |
| Inadequate support staff |
| Patient-related illness |
| More cases after normal working hours |
| Increased percentage of “emergency” procedures |
Patient Issues
Statistically, the NORA patient population is older than the population of patients undergoing traditional surgery in the operating room, and the average age of NORA patients is increasing more rapidly than in the group undergoing traditional surgery. NORA patients also tend to be more medically complex than those in the traditional operating room cohort, adding to overall patient risk.1,6 A greater percentage of patients receiving NORA are classified as ASA physical status III-V compared to those in the traditional operating room.1 Often these patients are not candidates for traditional operative procedures and their only option is a NORA intervention.2
As the number of older and medically complex patients receiving NORA grows, the anesthesia team must maintain an emphasis on the preprocedure evaluation for assessment of patient safety and procedural feasibility. Our ability to adequately assess these patients prior to their procedure may be limited or difficult, as many clinicians performing NORA procedures do not have either a pre-operative clinic or the dedicated space to examine patients preoperatively. Patient-specific comorbidities unique to each NORA specialty must be assessed prior to every procedure. For example, the anesthesia professional must evaluate the impact of esophageal stricture or reflux prior to endoscopy, the significance of heart failure prior to an electrophysiology study, or the severity of obstructive sleep apnea prior to an MRI study in which the ability to rapidly address airway obstruction may be limited. NORA patients may be critically ill, and procedures may need to be performed emergently. This urgency may result in a diminished ability of the patient to provide informed consent. Invasive monitoring may be necessary and should be prepared and available when needed. Fasting status must be evaluated prior to every procedure and must be considered when prescribing an anesthetic technique.
Additional concerns across the NORA spectrum include airway management during procedures that require a shared airway. Some procedures may involve placing the patient in a position other than supine, such as the prone and lateral positions for various gastrointestinal procedures, including colonoscopy and endoscopic retrograde cholangiopancreatography. In all situations, an emphasis must be placed on real-time communication between the anesthesia team, the proceduralist, nursing and other support staff. Open, multidisciplinary communication should begin prior to the start of the procedure (e.g., to discuss anesthetic choice and safety concerns), continue through the procedure, and into the recovery area always emphasizing patient safety.
Personnel/Support Team Issues
The traditional operating room is an area that has clearly delineated roles and practices. Anesthesia professionals are specifically trained to operate within this area. In contrast, non-operating procedure rooms are usually individualized and customized for specific procedures. Personnel working in the NORA environment may be unfamiliar with operating room protocols and be uncomfortable or unfamiliar with patients under anesthesia. They may have a focused medical or clinical background and are unfamiliar with anesthesia related problems and emergency protocols. Similarly, the anesthesia team may be treated as “outsiders,” in that they may not be familiar with a specialized facility, its environment, staff organization, and workflow. Open, free communication among the staff is paramount to safe practice, and barriers to sharing information should be identified and addressed. Compliance by staff to patient safety protocols should be augmented by regular instruction and evaluation.
Equipment and Monitoring
NORA equipment and monitoring should be held to the same standards as the traditional operating room. Appropriate equipment and standard monitoring are key to safety in the NORA suite. NORA cases are often performed in remote locations far from needed resources and with varying levels of typical anesthesia equipment. Anesthesia equipment may be outdated or retrofitted and, as previously stated, optimal workspace and patient access can be limited by both the actual procedure being performed and the physical constraints of the NORA room.6
In 2013, the ASA published guidelines to encourage safe, high quality care for NORA locations.7 These guidelines provide anesthesia professionals with minimum standards to providing safe care by mandating the use of standard monitoring equipment similar to the traditional operating room including monitoring oxygenation, ventilation, circulation and temperature.8 When providing NORA, anesthesia professionals should demand appropriate time to setup and check all necessary equipment and have access to the necessary resources to provide safe NORA. Improperly functioning equipment, suboptimal workspace, and inadequate support should not be tolerated in the NORA suite.
Improving Patient Safety for NORA Procedures
As NORA grows, patient safety and the quality of anesthesia provided must continue to be emphasized to decrease risk to patients. Reasonable first steps to improve patient safety for NORA cases include adequate case preparation and a familiarization with the location, equipment, and available staff. Overall, the anesthesia provider must work with the procedural team to assure the safety of the NORA environment for patient care. Additional preparation measures should include the routine maintenance of all anesthesia related equipment, an adequate supply of rescue medications, and the development of appropriate safety protocols. Establishing protocols for emergency procedures as well as establishing an appropriate response to adverse events add to the safety of NORA based practice.
Recent evidence strongly suggests that many NORA-related complications would be prevented through appropriate, vigilant monitoring and maintaining the same standard of care as used in the operating room.2 As stated above, a closed claims analysis showed that the majority of adverse outcomes in NORA are related to respiratory depression and inadequate monitoring. ASA monitoring standards should be instituted in all NORA environments whenever feasible, specifically emphasizing the assurance of adequate ventilation through clinical evaluation and monitoring expired carbon dioxide. As in the operating room, protocols and checklists ensuring the availability of personnel and equipment may help to standardize care to produce reliable and consistently safe results. These measures are helpful to manage both familiar and unfamiliar cases and may aid in providing uniform care even with unfamiliar staff. Each step of every protocol and pathway must be evaluated to create a consistent, safe, and uniform NORA environment for both practitioners and patients.
Adverse events can occur despite our best efforts to anticipate and prevent them. When these events do occur, it is essential to have a system in place to examine them and prevent future occurrences. Such a system must rely on a method to define and examine potential errors and near misses. Such systems should be proactive, rather than reactive. Quality improvement programs should be established and reinforced by debriefings, root cause analysis and continuing education programs.
The Future and Beyond
With the continued growth of NORA creating novel, complex procedures and utilizing advanced technology that require new and deeper levels of sedation, anesthesia professionals are well positioned to guide a multidisciplinary team approach, to improve practice, to increase value, and maintain patient safety.
Anesthesia professionals need to continue to define safe practices, establish appropriate guidelines, direct efficient resource management and establish risk related data. A continued emphasis must be placed on the education of our specialty through NORA specific trainee education and lifelong learning. As we look to provide efficient and safe NORA, we need to continue to evolve, utilizing advances in technology to improve our ability to preoperatively assess patients, monitor patients during and after procedures, and provide targeted anesthetics for a multitude of increasingly complex cases.9
Conclusion
NORA is an emerging field that is at the forefront of increasing the availability of procedural care for a wider variety of patients. Utilizing new technology to treat a wide variety of patient ailments will continue to lead to new challenges for the anesthesia professional providing NORA. Better understanding of safe practice and the risks associated with NORA will allow anesthesia professionals to be at the frontline of this rapidly evolving and expanding sub-specialty.
Dr. Walls is assistant professor of Clinical Anesthesiology and Critical Care at the University of Pennsylvania School of Medicine.
Dr. Weiss is assistant professor of Clinical Anesthesiology and Critical Care at the University of Pennsylvania School of Medicine.
The authors have no conflicts of interest pertaining to this article.
The information provided is for safety-related educational purposes only, and does not constitute medical or legal advice. Individual or group responses are only commentary, provided for purposes of education or discussion, and are neither statements of advice nor the opinions of APSF. It is not the intention of APSF to provide specific medical or legal advice or to endorse any specific views or recommendations in response to the inquiries posted. In no event shall APSF be responsible or liable, directly or indirectly, for any damage or loss caused or alleged to be caused by or in connection with the reliance on any such information.
References
- Nagrebetsky A, Gabriel RA, Dutton RP, Urman RD. Growth of nonoperating room anesthesia care in the United States: a contemporary trends analysis. Anesth Analg. 2017; 124:1261–7.
- Chang B, Kaye AD, Diaz JH, et al. Interventional procedures outside of the operating room: results from the National Anesthesia Clinical Outcomes Registry. J Patient Saf. 2018;14:9–16
- Woodward ZG, Urman RD, Domino KB. Safety of non-operating room anesthesia: a closed claims update. Anesthesiol Clin. 2017;35:569-581.
- Melloni C. Anesthesia and sedation outide the operating room: how to prevent risk and maintain good quality. Curr Opin Anaesthesiol. 2007;20:513–519.
- Metzner J, Domino KB. Risks of anesthesia or sedation outside the operating room: the role of the anesthesia care provider. Curr Opin Anaesthesiol. 2010;23:523–31.
- Metzner J, Posner KL, Domino KB. The risk and safety of anesthesia at remote locations: the US closed claims analysis. Curr Opin Anaesthesiol. 2009;22:502–508.
- American Society of Anesthesiologists Committee on Standards and Practice Parameters. Statement on nonoperating room anesthetizing locations. October 17, 2018. Available at: https://www.asahq.org/standards-and-guidelines/statement-on-nonoperating-room-anesthetizing-locations. Accessed March 15, 2019.
- American Society of Anesthesiologists Committee on Standards and Practice Parameters. Standards of basic anesthetic monitoring. October 25, 2015. Available at: https://www.asahq.org/standards-and-guidelines/standards-for-basic-anesthetic-monitoring. Accessed March 15, 2019.
- Lu AC, Wald SH, Sun EC. Into the wilderness?:the growing importance of nonoperating room anesthesia care in the United States. Anesth Analg. 2017;124:1044–46.


 Issue PDF
Issue PDF