INTRODUCTION
Anesthesiology as a specialty has a long history of innovation in technology development linked to improvements in patient safety. However, the speed of technological development in the past 20 years has been unprecedented. This is mostly related to the exponential growth of data and computer power leading to the application of artificial intelligence (AI) tools to the perioperative setting. Today, emerging technology in anesthesiology and perioperative medicine has a tremendous potential to improve patient safety and quality of care even further. The application of AI will improve patient safety by helping the individual clinician rapidly navigate data from disparate sources and by effectively assisting the clinician to synthesize and make better, more informed medical decisions within a complex health care system.1-3 Furthermore, AI will be used to improve patient safety by its integration into the workflow of perioperative patient safety and quality leaders, patient safety scientists, and health care system leaders. The role of AI towards improving patient safety extends from its ability to augment policy decisions designed to identify, assess, and mitigate threats to patient safety at scale.4,5 In this brief review, we provide an overview of AI as an emerging technology and provide a practical framework for anesthesia professionals to understand the important relationship between AI and perioperative patient safety.
PATIENT SAFETY AND EMERGING TECHNOLOGIES IN A COMPLEX WORLD
Patient safety can be defined as the absence of preventable harm to a patient and minimizing the risk of harm in health care delivery.6 As leaders in patient safety, anesthesia professionals have been at the forefront of research, quality improvement, adoption of technology, and incorporation of engineering principles to reduce harm and risk to patients. The challenge of delivering safe anesthesia care in modern-day perioperative medicine can become a patient safety concern on its own, as the complexity of patient conditions, speed of care delivery, scale of health systems, challenges in multispecialty communication, and sheer volume of data generated increases over time. The need for anesthesia care teams to scale their knowledge, presence, and effectiveness across the perioperative and health care environment has never been greater, especially at a time when the stress on the workforce is tremendous.
To respond to the current health care delivery challenges and continue to deliver on the promise of patient safety, anesthesia care teams need to understand emerging technologies and those that are available to help improve patient safety. AI is one of the major emerging technologies that has already changed the world outside health care and is on the precipice of more widespread adoption within health care. To responsibly advance the field of perioperative patient safety, anesthesia professionals need to understand the principles of AI, the possibilities, the risks, the ethics, and the use of AI in clinical practice. This will require the partnership and collaboration of a diverse team within health care including the ability for anesthesia professionals to communicate effectively with data scientists, computer scientists, data analysts, and artificial intelligence experts.
OVERVIEW OF ARTIFICIAL INTELLIGENCE APPLICATIONS IN ANESTHESIOLOGY
AI can be broadly defined as the ability of a computer or device to analyze a large volume of complex health care data, reveal knowledge, identify risks and opportunities, and support improved decision-making.7 While the field of AI is rapidly evolving, major techniques used in health care include machine learning, natural language processing,3 and combining AI with clinical decision support through the development of graphic user interfaces.
Machine learning is one of the most common forms of AI and can be considered a statistical technique for fitting models to data with the computer “learning” how to understand the data by using training datasets as examples.8 Advanced forms of machine learning include neural networks and deep learning. Recent examples of machine learning in anesthesiology include studying which variables were predictive of postinduction hypotension using electronic health record data,9 forecasting the bispectral index (BIS™, Medtronic, Dublin, Ireland) value based on the infusion history of propofol and remifentanil,10 or prediction of postoperative in-hospital mortality using preoperative and intraoperative data.11
Natural language processing is a form of AI that can be used to extract relevant information from unstructured text data. For example, natural language processing was recently used in a retrospective study to assess whether unstructured free text of medical conditions in the electronic medical records could be extracted by a computer and used to generate an automated preanesthetic evaluation report. The results focused on how often the natural language processing software recognized medical conditions as compared to an anesthesia professional. The study suggested that natural language processing was able to pick up relevant conditions missed by the clinician in 16.57% of the cases, and missed relevant conditions noted by clinicians in only 2.19% of the cases.12 The opportunities for using natural language processing to scale and augment the ability of an individual anesthesia professional in a complex care environment with limited staffing resources is a compelling use of AI for patient safety.
Artificial intelligence can also be used with clinical decision support systems, which can be found in modern anesthesia care where the anesthesia information management system can provide electronic reminders to the anesthesia team on perioperative antibiotic dosing, use of postoperative nausea and vomiting prophylaxis in high-risk patients, and assist with blood glucose management. A recent meta-analysis demonstrated that clinical decision support can enhance compliance with perioperative antibiotic prophylaxis.13 Future roles of AI in clinical decision support to improve patient safety would include providing recommendations on the ideal antibiotic given the patient’s electronic medical record information, medical history, and surgical procedure. AI can also be used to advance perioperative patient safety through earlier detection of clinical deterioration and provide clinical decision support for the optimal management of intraoperative physiologic changes.
THE QUINTUPLE AIM
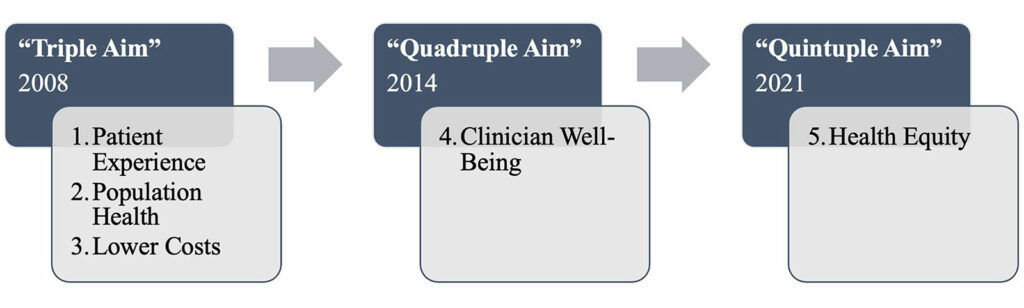
Understanding the direct impact AI will have on perioperative patient safety can be seen through the lens of the Quintuple Aim (Figure 1). The Quintuple Aim is the proposed next step in improving patient safety and quality of care delivered. The Institute for Healthcare Improvement introduced the Triple Aim in 2008, as a framework to improve the patient experience, address population health, and lower costs as keys to health care transformation.14 In 2014, the Quadruple Aim was introduced to include clinician well-being, in response to research demonstrating that clinician engagement and burnout led to more safety events and reduced quality of care.15 Many accrediting groups such as the National Committee for Quality Assurance and the Joint Commission recognized the importance of delivering on the Triple and Quadruple Aim. In 2022, the Quintuple Aim was proposed to add a fifth aim: advancing health equity. This was a recognition that delivering high-quality and safe patient care for populations, and to achieve the other aims, meant a focus on actively measuring, studying, and addressing disparities.16
AI has a critical role to play in perioperative patient safety through the lens of the Quintuple Aim. In the complex modern health care delivery system, AI can help anesthesia professionals address the five aims of the Quintuple Aim, which could then translate to improved safety and quality of care in the perioperative continuum. Figure 2 provides a variety of potential examples of AI applications within the framework of the Quintuple Aim to improve patient safety and quality.
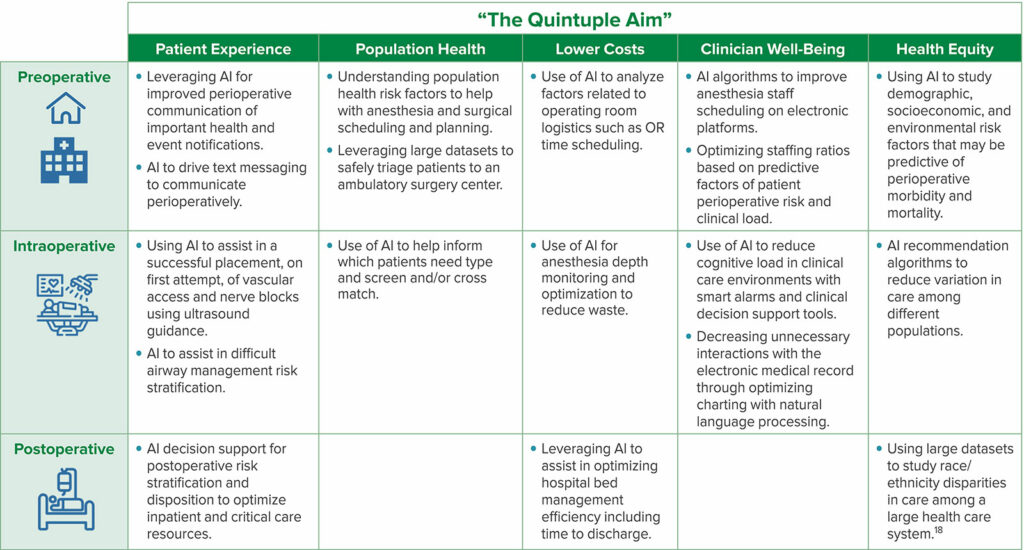
Figure 2: Framework applying the Quintuple Aim in applications of artificial intelligence in anesthesiology addressing patient safety across the perioperative continuum.
BRINGING IT ALL TOGETHER
Harnessing AI to improve patient safety in anesthesiology will take a significant amount of work from individual clinicians, anesthesiology groups, health care systems, and regulatory agencies such as the US Food and Drug Administration (FDA). AI is not as widespread in clinical practice as some would have expected only five years ago. Furthermore, adoption of AI with patient safety science and practice will still require time to mature. Many events are portending the real integration of AI and perioperative patient safety. New regulatory pathways developed by the FDA in 2019 have reduced the regulatory barriers and subsequent financial uncertainty to allow companies to develop AI application in health care. Unlike traditional medical devices, the nature of software updates and other differences meant that AI and machine learning software needed to be regulated under its own pathway as a medical device. With more clarity on regulation and improved research and development in AI within health care, it is likely that deploying AI at the individual and health system level will increase.
Other important considerations of AI in healthcare include ensuring transparent levels of understanding about how algorithms are designed as well as minimizing and eliminating bias associated with AI algorithms.17 For example, AI algorithms that help improve the performance of clinicians need to also be understood by the teams using them, which include a level of transparency in how the algorithms function.18 In addition, particular attention to the foundational development of AI algorithms and the data used to generate AI tools needs to take place to reduce risks of race/ethnicity, socioeconomic, and statistical bias.18-20
CONCLUSION
To advance the field of anesthesiology and perioperative patient safety, emerging technologies such as AI will need to be learned and incorporated into the field of clinical anesthesiology. For AI to be effective, implementation of data-driven analytics with patient safety paradigms in anesthesiology will require organizations to innovate by supporting the development and building of multidisciplinary teams of clinicians, data scientists, engineers, informaticians, and patient safety scientists. As anesthesia care delivery continues to evolve, the multidisciplinary nature of perioperative patient safety will need to respond with an innovative multidisciplinary approach, team, and solution—one that harnesses the scalability and strengths of AI through the lens of the Quintuple Aim.
Jonathan Tan, MD, MPH, MBI, FASA, is an assistant professor of Clinical Anesthesiology and Spatial Science at the Children’s Hospital Los Angeles, the Keck School of Medicine at the University of Southern California, and Spatial Sciences Institute at the University of Southern California, Los Angeles, CA.
Maxime Cannesson, MD, PhD, is a professor of anesthesiology and chair of the Department of Anesthesiology and Perioperative Medicine at the David Geffen School of Medicine at the University of California, Los Angeles, CA.
Disclosures: Jonathan Tan, MD, MPH, MBI, FASA, receives research grant funding from the Anesthesia Patient Safety Foundation (APSF) and the Foundation for Anesthesia Education and Research (FAER).
Maxime Cannesson, MD, PhD, is a consultant for Masimo and Edwards Lifesciences, receives research support from Masimo and Edwards Lifesciences, is a shareholder for Sironis and Perceptive Medical, and receives Royalties from Edwards Lifesciences.
References
- Grossman LV, Choi SW, Collins S, et al. Implementation of acute care patient portals: recommendations on utility and use from six early adopters. J Am Med Inform Assoc. 2018;25:370–379. PMID: 29040634.
- Macrae C. Governing the safety of artificial intelligence in healthcare. BMJ Qual Saf. 2019;28:495–498. PMID: 30979783.
- Choudhury A, Asan O. Role of artificial intelligence in patient safety outcomes: systematic literature review. JMIR Med Inform. 2020;8:e18599. PMID: 32706688.
- Dalal AK, Fuller T, Garabedian P, et al. Systems engineering and human factors support of a system of novel EHR-integrated tools to prevent harm in the hospital. J Am Med Inform Assoc. 2019;26:553–560. PMID: 30903660.
- Maddox TM, Rumsfeld JS, Payne PRO. Questions for artificial intelligence in health care. JAMA. 2019;321:31–32. PMID: 30535130
- World Health Organization. Patient Safety. Sept 13, 2019. Accessed November 8, 2022. https://www.who.int/news-room/fact-sheets/detail/patient-safety#:~:text=What%20is%20Patient%20Safety%3F,during%20provision%20of%20health%20care.
- Hashimoto DA, Rosman G, Rus D, Meireles OR. Artificial intelligence in surgery: promises and perils. Ann Surg. 2018;268:70–76. PMID: 29389679.
- Bi Q, Goodman KE, Kaminsky J, Lessler J. What is machine learning? A primer for the epidemiologist. Am J Epidemiol. 2019; 188: 2222–2239. PMID: 31509183.
- Kendale S, Kulkarni P, Rosenberg AD, Wang J. Supervised machine-learning predictive analytics for prediction of postinduction hypotension. Anesthesiology. 2018;129:675–688. PMID: 30074930.
- Lee HC, Ryu HG, Chung EJ, Jung CW. Prediction of bispectral index during target-controlled infusion of propofol and remifentanil: a deep learning approach. Anesthesiology. 2018;128:492–501. PMID: 28953500.
- Lee CK, Hofer I, Gabel E, et al. Development and validation of a deep neural network model for prediction of postoperative in-hospital mortality. Anesthesiology. 2018;129:649–662. PMID: 29664888.
- Suh HS, Tully JL, Meineke MN, et al. Identification of preanesthetic history elements by a natural language processing engine [published online ahead of print, 2022 Jul 15]. Anesth Analg. 2022 Dec 1;135:1162–1171. PMID: 35841317.
- Simpao AF, Tan JM, Lingappan AM, et al. A systematic review of near real-time and point-of-care clinical decision support in anesthesia information management systems. J Clin Monit Comput. 2017;31:885–894. PMID: 27530457.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27:759–769. PMID: 18474969.
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573–576. PMID: 25384822.
- Nundy S, Cooper LA, Mate KS. The quintuple aim for health care improvement: a new imperative to advance health equity. JAMA. 2022;327:521–522. PMID: 35061006.
- Canales C, Lee C, Cannesson M. Science without conscience is but the ruin of the soul: the ethics of big data and artificial intelligence in perioperative medicine. Anesth Analg. 2020;130:1234–1243. PMID: 32287130.
- Diallo MS, Tan JM, Heitmiller ES, Vetter TR. Achieving greater health equity: an opportunity for anesthesiology. Anesth Analg. 2022;134:1175–1184. PMID: 35110516.
- Amann J, Blasimme A, Vayena E, et al. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak. 2020; 310 (20). PMID: 33256715.
- Parikh RB, Teeple S, Navathe AS. Addressing bias in artificial intelligence in health care. JAMA. 2019; 322:2377–2378. PMID: 31755905.


 Issue PDF
Issue PDF PDF
PDF