Past and Present
Ophthalmic anesthesia dates to 1884 when ophthalmologist Karl Koller1 first introduced the use of cocaine as a local anesthetic for ophthalmic surgery. The retrobulbar blockade was first described by Herman Knapp in 1884, and later Atkinson in 19362 described a retrobulbar technique that was adopted very quickly; however, due to a high incidence of complications the technique was abandoned over time.3 Currently, at Massachusetts Eye and Ear Infirmary (MEEI), Boston, MA, we provide anesthesia services under local, regional, and general anesthesia for more than 16,000 ophthalmic procedures a year in both adult and pediatric patients.
Safe Ophthalmic Anesthesia
The basic tenets for safe anesthesia care during elective eye procedures are to facilitate maximal pain relief, ease in the surgical procedure, quick recovery, and minimal risks associated with surgery and anesthesia.4,5 Over the past 30 years, advancement of surgical techniques has allowed for short, effective, and safe patient care.
Most of the current ophthalmic procedures can be performed in ambulatory surgery centers (ASCs) and in the office-based surgical setting. A key component to this success is through selection of the appropriate patient, procedure, and location, all determined by clinical criteria and equipment demand. At MEEI, we provide clinical care at our main hospital campus, where we have both inpatient and outpatient services, and at our free-standing ASC. This arrangement allows flexibility when scheduling cases in order to improve efficiency at both locations.
Pharmacology
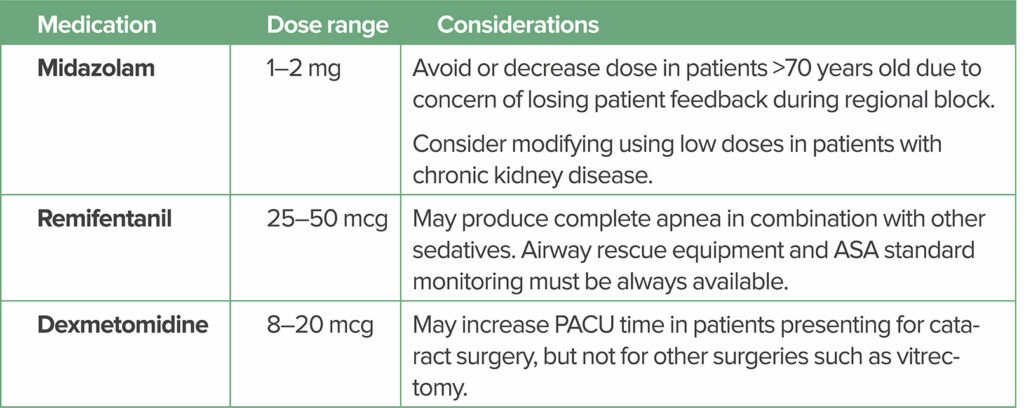
Over the years, our practice has evolved to meet the demand for faster, safer, and more efficient anesthesia. Essential to these goals has been the use of short- and long-acting local anesthetics. The goal of sedation is to decrease anxiety, while maximizing safety. Combined with the use of regional anesthesia, several choices of sedation and analgesic combination medications have been introduced to the practice within the last 25 years, such as remifentanil, dexmetomidine, and midazolam (see Table 1). These short-duration sedatives can be administered immediately before the regional block to reduce or eliminate the pain of needle insertion and injection of the local anesthetic.5 Prolonged sedation is used with caution in select patients, and is generally preferably avoided, as an awake patient is needed for surgery. Some practices use small doses of propofol until the patient loses consciousness while the block is performed.
Table 1: Potential Medications* Used for Sedation During Ophthalmic Procedures
We always provide supplemental oxygen if performing an eye block and during the surgical intervention. At MEEI, we use a nasal canula at flows not higher than 5 l/min or a face tent. The face tent sits at the level of the patient’s chin. It provides oxygenation while preventing the drapes from sitting on the patient’s lower face (helping with the feeling of claustrophobia in some cases). An important observation is there is a small risk of CO2 accumulation under the drapes. For short procedures the risk is minimal; however, for procedures longer than an hour, we recommend using CO2 suctioning.
For eye blocks, we usually use a combination of lidocaine, bupivacaine, and the hyaluronidase enzyme. The combination of lidocaine 1.5% and bupivacaine 0.375% provides a block with rapid onset (between 5–10 minutes) and a duration of about 2 hours, which is enough for most procedures. Lidocaine should not be used in concentrations higher than 2% due to the risk of myositis if injected by error into one of the extraocular muscles. Duration and onset may be related to the volume injected although this is controversial. The enzyme hyaluronidase as an ancillary agent is usually used with local anesthetics.5 Concentrations between 1 and 7.5 units/mL are most commonly used, but concentrations as low as 0.75 units/mL may be effective.6 The addition of hyaluronidase is used to increase tissue permeability of the local anesthetic, promote dispersion of the local anesthetic, reduce the increase in orbital pressure associated with the injected volume, enhance the quality of the block, and reduce the risk of injury to the extraocular muscles if local anesthetic is injected in them.5
Patients
Proper communication with the patient, surgeon, and anesthesia professionals is essential. Patients should be advised and comprehend that they must lie flat (or semi-flat due to comorbidities), remain motionless, cooperate by providing clear communication, and express any concerns regarding claustrophobia or panic attacks, as needed. A focused medical history, including use of any anticoagulant or antithrombotic therapies, previous eye operations, and overall suitability for same-day surgery is also required. The physical exam should focus on airway assessment, detection of relevant abnormalities, including any conditions that may impede the ability to lie supine comfortably (e.g., back deformities or pain, severe congestive heart failure, chronic obstructive pulmonary disease, or claustrophobia). These are more relevant when topical or regional anesthesia is planned in association with sedation.
Controversies:
NPO
Although controversial, we still recommend that our patients follow standard ASA fasting (NPO) guidelines to reduce risk of aspiration should there be a need to convert to general anesthesia.
Anticoagulation:
We recommend that patients with a high risk of clotting and embolic complications (due to cardiac or vascular pathologies) continue therapeutic doses of aspirin or warfarin throughout the perioperative period. Recent publications have shown no higher incidence of sight-threatening bleeding complications after regional anesthesia in patients taking aspirin, warfarin, or clopidogrel before cataract surgery, compared with patients not taking these drugs.7 Similarly, recent literature has been published regarding concerns of increased bleeding risk in patients taking newer oral anticoagulants, such as apixaban, rivaroxaban, and dabigatran. At MEEI in Boston, our recent retrospective study on the continuation of these medications also did not result in a higher incidence of bleeding complications in patients presenting for elective eye surgery and receiving regional anesthesia as the primary technique.8
Gas injection:
Gas injection is mainly used during retina surgery. If general anesthesia is provided, patients should not receive nitrous oxide when gas is going to be injected in the eye (e.g., SF6 or C3F8), or when gas was previously administered to create a “bubble” to internally tamponade the detached retina, unless an ophthalmologist has documented that the bubble has been completely absorbed. Although SF6 is usually completely absorbed by 10 days, and C3F8 by six weeks, there are case reports of blindness due to use of nitrous oxide after 25 days for SF6 and after 41 days for C3F8.9 Patients who have received one of these gases must be identified. At MEEI, we place a wrist band that includes the name of the gas injected as well as the date and time in order to alert any providers in case of a potential emergency.
Procedures
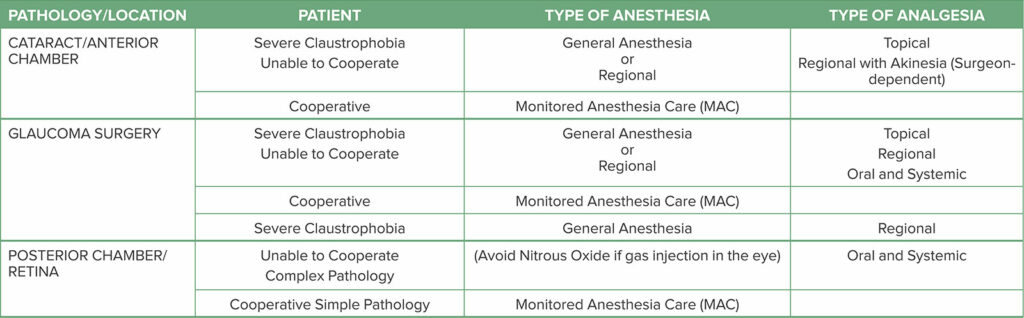
The most common procedures performed at our ASC are cataract, glaucoma, retina, oculoplastics, and strabismus surgeries. At our main campus, we include eye trauma, pediatric exams under anesthesia, transplant of limbal cells, gene therapy injections in the eye, and complex corneal transplants. For the most common ophthalmic surgical procedures, at our institution the anesthesia professional performs extraconal blocks. Other blocks such as intraconal blocks, topical, Sub-Tenon’s (episcleral), and intracameral injections of preservative-free local anesthetic are performed by the surgeon.18 Anesthesia considerations for those patients with claustrophobia or who are uncooperative are depicted in Table 2.
Table 2: Anesthesia Considerations for Common Eye Procedures for Claustrophobic and/or Uncooperative Patients
General anesthesia is more commonly provided to patients with history of claustrophobia, patients unable to lie flat for the duration of the surgery, pediatric patients, and patients presenting for complex interventions that may take more than two hours.
Training
Cataract surgery is one of the most common outpatient surgeries performed in ASCs, and the risk of complications related to eye blocks as well as a wrong-side surgery is always present. Although uncommon in the hands of well-trained skilled anesthesia professionals, these complications can carry devastating effects in the life of any patient. Therefore, we suggest that proper training in anesthesia for ophthalmic surgery is essential and should be included in all residency programs.
Regional anesthesia techniques for the eye are safe when performed by experienced providers or under the supervision of someone properly trained. Presently, there is a lack of training in anesthesia residency and regional anesthesia fellowships programs with regards to ophthalmic procedural regional anesthesia techniques. At MEEI, we have instituted a regional anesthesia rotation for residents and regional anesthesia fellows. The regional anesthesia fellows spend two weeks learning how to perform eye blocks. At the same time, they learn how to handle our high patient workflow while maintaining safety and efficiency. Anesthesia professionals should be very well versed in both the anesthetic performance and patient management for eye surgeries.
Complications
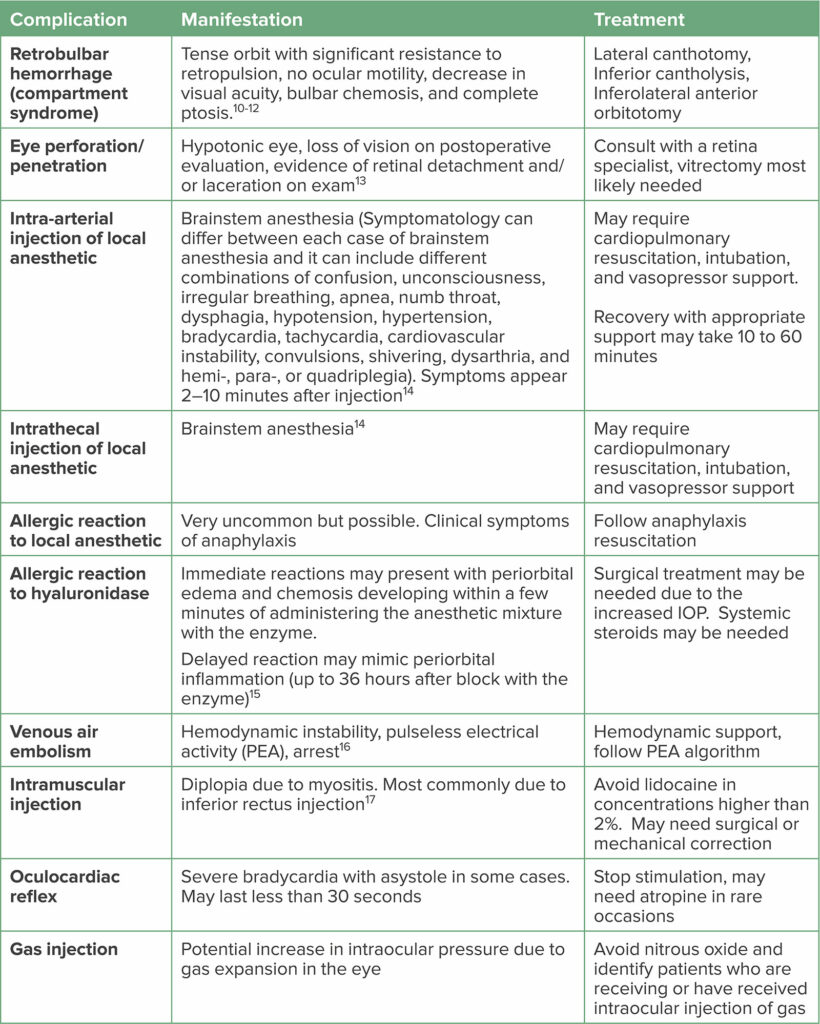
As with any other intervention, complications can occur when performing eye blocks. Table 3 depicts eye procedure complications and the associated treatment strategies.
Table 3: Eye Procedure Complications and Management Strategies9
Special Considerations During COVID-19 Pandemic
The COVID-19 pandemic has affected the way we provide anesthesia to our ophthalmic population like other specialties. In our institution, PCR testing is mandatory for any patient requiring general anesthesia, and it is optional for any patient going under sedation as there is a potential need for mask ventilation (an aerosol-generating procedure [AGP]) if oversedation takes place. It is crucial to ensure that patients undergoing office procedures have stable medical conditions, are not experiencing any symptoms of COVID-19, have not had close contact with a confirmed COVID-19 patient (i.e., less than 6 feet distance with at least 15 minutes of exposure), and present with a negative COVID-19 test within 72 hours of the procedure.19 In Figure 1, Young et al. suggest a testing and screening algorithm for the office-based setting.
Figure 1: COVID-19 Testing and Screening Algorithm
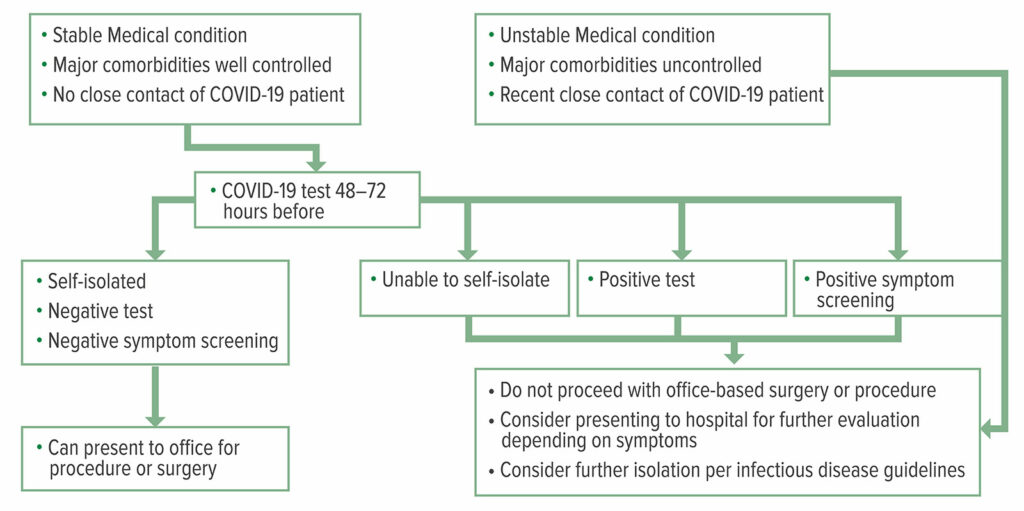
Reproduced and modified with permission from: Young et al. Patients, Procedures, and PPE: Safe Office-Based Anesthesia Recommendations in the COVID-19 Era. Best Prac Research Clin Anaesthesiol. 2020 Nov. (article in press) https://doi.org/10.1016/j.bpa.2020.11.006
Recommendations in the COVID-19 Era
Another challenge involves deciding the amount of PPE to be used, considering that the number of COVID-19 cases is constantly in flux with some areas experiencing more cases than others. There are two algorithms to address areas of low prevalence and high prevalence of COVID-19 cases (less than and greater than 4 cases per 100,000 population, respectively) (see Figure 2).
Figure 2: COVID-19 Personal Protective Equipment (PPE) Algorithms for Low Versus High Prevalence COVID-19 Areas
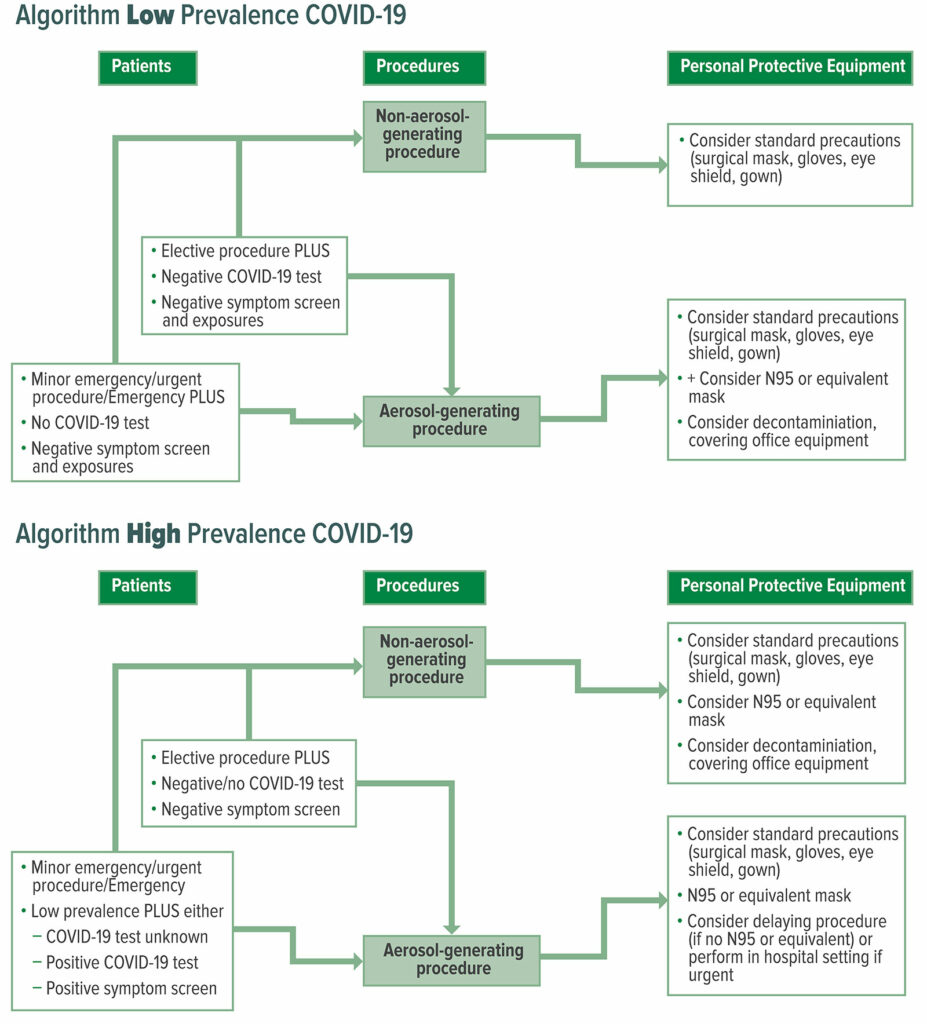
Reproduced and modified with permission From: Young et al. Patients, Procedures, and PPE: Safe Office-Based Anesthesia Recommendations in the COVID-19 Era. Best Prac Research Clin Anaesthesiol. 2020 Nov. (article in press) https://doi.org/10.1016/j.bpa.2020.11.006
There must be a conversation between the surgeon and anesthesia professional, when conversion from a monitored anesthesia care case to a general anesthetic is required and COVID-19 testing is limited or unavailable. We recommend rescheduling the case and ordering a COVID-19 PCR test within 72 hours of the surgical date, for any elective cases that require transition from sedation to general anesthesia.20 There are occasional circumstances, when a patient may become agitated or develop a panic attack during surgery and conversion from sedation to general anesthesia is necessary, and full PPE is required.19 As noted, these events are very rare in our practice.
The COVID-19 pandemic has changed many aspects of our lives, including many changes to our medical practices aimed to reduce or minimize the risk of community and hospital transmission of the SARS-CoV-2 virus. Part of identifying this risk is recognizing which procedures produce aerosolized particles and which, as seen by the algorithms below, result in modifications in PPE usage for the procedure being performed.
Several studies have examined if ophthalmological procedures in fact result in the aerosolization of particles. A study of 30 phaco-emulsification studies detected no intraoperative aerosolization in any of the cases regardless of technique.20 Noureddin et al. used a sophisticated aerosol monitor to detect aerosolization in phacoemulsification cataract surgeries in porcine subjects. They also concluded that it was not an aerosol-generating medical procedure.21
Results of these studies indicate that ophthalmologists may safely perform these surgeries by adhering to traditional droplet precautions during the COVID-19 pandemic.
In consideration of this data regarding these nonaerosol producing procedures, the algorithms will have to be adjusted accordingly, and the type of anesthesia will also need to be reconsidered. Although a procedure such as phacoemulsification may not generate aerosol particles, endotracheal intubation for general anesthesia can result in potential aerosolization. Until the Centers for Disease Control (CDC) updates their policies with new recommendations, the current algorithms should be maintained.
We are now learning that acute infection with COVID-19 is not the end of the road. Patient selection criteria must now include determination of COVID status, vaccination status, and prior infection with long-standing comorbidities. The well recognized COVID-19 “long-hauler” status can include lingering fatigue, dizziness, shortness of breath, chest pain, muscle and/or joint pain, loss of smell or taste, depression or anxiety, memory or concentration problems, blood clots and vessel problems, and even sustained organ damage to the heart, lungs, or brain.22
Our Future Vision
As new techniques continue to evolve, we recognize that the trend of performing elective ophthalmic procedures in the ambulatory setting will continue to grow. Commensurate with this, we appreciate a continued increase in an elderly and sicker patient population that will require elective eye interventions. For example, we recently encountered patients presenting to the OR with left ventricular assist devices (LVAD) for elective eye surgery. In order to continue to maintain a safe and appropriate environment, we recommend developing ongoing policies that support appropriate patient, procedure, and location selection. In the past five years, there have been reports claiming that complications related to eye blocks have occurred due to the use of incorrect techniques or settings. Therefore, we strongly believe that it is prudent to implement a formal educational program that includes clinical and technical skills, interpersonal and interprofessional communication, practice management, policies, simulation training, standards, guidelines, and regulations. At the MEEI, we have been successful in implementing this educational curriculum and created the official MEEI Manual for ophthalmic procedures to accompany the curriculum as a “pocket” resource. To share our program globally, along with the MEEI Manual release in 2022, we envision the availability of both live and virtual MEEI/HMS Continuing Medical Education (CME) opportunities.
Andres Macias, MD, FASA, is chief of Anesthesia, assistant professor, Harvard Medical School, Massachusetts Eye and Ear Infirmary, Boston, MA.
Fred E. Shapiro, DO, FASA, is associate professor of Anesthesia, Harvard Medical School, Massachusetts Eye and Ear Infirmary, Boston, MA.
The authors have no conflicts of interest.
References
- Altman AJ, Albert DM, Fournier GA. Cocaine’s use in ophthalmology:our 100-year heritage. Surv Ophthalmol. 1985;29:300-306. doi: 10.1016/0039-6257(85)90154-7.
- Polania Gutierrez JJ, Riveros Perez E. Retrobulbar block. [Updated 2021 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. Accessed July 7 2021. Available at: https://www.ncbi.nlm.nih.gov/books/NBK557448/
- Davis DB, Mandel MR. Posterior peribulbar anesthesia: an alternative to retrobulbar anesthesia. J Cataract Refract Surg. 1986;12:182–184.
- Macias, AA, Bayes J, McGoldrick, KE. Anesthesia for elective eye surgery. UpToDate. 2021. Accessed June 25 2021. Available at: https://www.uptodate.com/contents/anesthesia-for-elective-eye-surgery.
- Rüschen H, Aravinth K, Bunce C, Bokre D. Use of hyaluronidase as an adjunct to local anaesthetic eye blocks to reduce intraoperative pain in adults. Cochrane Database Syst Rev. 2018; 3:CD010368.
- DeBroff BM, Hamilton RC, Loken RG, et al. Retrobulbar anesthesia with 7.5 vs. 0.75 IU/mL of hyaluronidase. Can J Ophthalmol. 1995;30:262.
- Benzimra JD, Johnston RL, Jaycock P, et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: antiplatelet and anticoagulant medications. Eye. (Lond). 2009;23:10–16.
- Macias A, et al. Evaluating the outcomes and safety of peribulbar anesthesia for patients taking direct oral anticoagulants. EC Ophthalmology 10.2 (2019):120–124.
- Seaberg RR, Freeman WR, Goldbaum MH, Manecke GR Jr. Permanent postoperative vision loss associated with expansion of intraocular gas in the presence of a nitrous oxide-containing anesthetic. Anesthesiology. 2002;97:1309–1310.
- Macias AA, Bayes J, McGoldrick KE. Anesthesia for elective eye surgery. UpToDate. 2020 Mar. Accessed July 8, 2021. Available at: https://www.uptodate.com/contents/anesthesia-for-elective-eye-surgery#H115132139.
- Huebert I, Heinicke N, Kook D, et al. Dual platelet inhibition in cases of severe retrobulbar hemorrhage following retrobulbar and peribulbar anesthesia. J Cataract Refract Surg. 2015;41:2092–2101.
- Takaschima A, Marchioro P, Sakae TM, et al. Risk of hemorrhage during needle-based ophthalmic regional anesthesia in patients taking antithrombotics: a systematic review. PLoS One. 2016;11:e0147227.
- Edge R, Navon S. Scleral perforation during retrobulbar and peribulbar anesthesia: risk factors and outcome in 50,000 consecutive injections. J Cataract Refract Surg. 1999; 25:1237–1244.
- Kostadinov I, Hostnik A, Cvenkel B, Potočnik I. Brainstem anaesthesia after retrobulbar block. Open Med. 2019;14:287–291.
- Rajalakshmi AR, Kumar MA. Hyaluronidase hypersensitivity: A rare complication of peribulbar block. Indian J Ophthalmol. 2016;64:160–162.
- Moon YE. Venous air embolism during vitrectomy: rare but potentially fatal complication. Korean J Anesthesiol. 2014;67:297–298.
- Hussain N, McCartney CJL, Neal JM, Chippor J, Banfield L, Abdallah FW. Local anaesthetic-induced myotoxicity in regional anaesthesia: a systematic review and empirical analysis. Br J Anaesth. 2018;121:822–841.
- Macias AA, Bayes J, McGoldrick KE. Anesthesia for elective eye surgery. https://www.uptodate.com/contents/anesthesia-for-elective-eye-surgery. Accessed September 1, 2021.
- Young S, Osman BM, Urman RD, Shapiro FE. Patients, procedures, and PPE: safe office-based anesthesia recommendations in the COVID-19 era. Best Prac Research Clin Anaesthesiol. 2020 Nov. https://doi.org/10.1016/j.bpa.2020.11.006
- Wong JKW, Kwok JSWJ, Chan JCH, et al. Aerosolization and fluid spillage during phacoemulsification in human subjects. Clin Ophthalmol. 2021;15:307–313.
- Noureddin GS, Iovieno A, Eslami M, et al. Quantification of aerosol generation during cataract surgery. J Cataract Refract Surg. 2020 Nov 30. doi: 10.1097/j.jcrs.0000000000000530. Epub ahead of print.
- COVID-19 (coronavirus): Long-term effects. Mayo Clinic. Mayo Foundation for Medical Education and Research (MFMER). 2021. Accessed July 6 2021. Available at: https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-long-term-effects/art-20490351.


 Issue PDF
Issue PDF