Failure mode and effects analysis (FMEA) is a valuable tool used for process analysis, most prominently in manufacturing or assembly processes, primarily in high risk industries. It is used to assess processes, break them down into individual steps and determine possible sites for failure. Assigning a risk priority number (RPN) for each step allows leaders to utilize resources including time, money and manpower in a more efficient manner to make the biggest impact. FMEA may be used in perioperative medicine to improve process efficiency and maintain patient safety.
Failure mode and effects analysis (FMEA) is an invaluable tool that has been used in industry to identify potential points of failure in a process, to evaluate their causes and effects, and to determine ways to decrease risks.1 Patient safety initiatives have incorporated strategies such as FMEA in addition to other techniques, e.g., root cause analysis (RCA) and the safety assessment code (SAC). The patient safety program at the Dept. of Veterans Affairs (VA)2 dates back nearly 30 years; approaching error reduction on a systemic basis in the VA was associated with a significant reduction in MRI hazards and cardiac pacemaker malfunction, supporting the role of proactive analysis.2 Systemic analysis for patient safety improvement has a long history, including such programs as the Safer Patients Initiative launched in the United Kingdom (2004–2008), which in its first year saw a decrease of adverse events from 7% to 1.5% per 1,000 patient days by improving reliability in general ward care, critical care, perioperative care, and medication management.3
Risk assessment using FMEA has been used effectively in hospitals to minimize medical errors; it has been deployed in many different settings.4,5,6 One study of administration of unfractionated heparin identified hundreds of potential failures with a hundred more causes, and deployed dozens of countermeasures to improve medication administration safety.7 After an extensive study at a 367-bed academic pediatric hospital, 233 potential points of failure were identified with the administration of unfractionated heparin including mathematical errors, unknown requirements for administration, incorrect timing, difficulties accessing information from hospital EMR, poor patient education, and the ability to administer incorrect dosages.7 The application of countermeasures for the process steps identified as having the highest Risk Priority Number yielded a statistically significant improvement in the scores with resultant improvement in safety for the administration of unfractionated heparin.7
FMEA has been successfully deployed to enhance the safety of radiotherapy,8-10 hospital or community pharmacy processes,11,12 clinical laboratory processes,13 blood transfusion,14 and clinical trials.15 Deployment of FMEA across a unit or service has also been demonstrated to improve such processes as transfers of care, lab/radiology requests or admission in Emergency Departments,16,17 and overall systemic functionality in intensive care units (ICUs).18 Finally, FMEA has been successful at attempts to not only improve systemic processes, but also to identify points of failure leading to hospital complications such as posture syndrome of thyroid surgery19 or venous thromboembolic disease in critically ill patients.20
Despite its demonstrated benefit, there is sparse literature examining the role of FMEA in anesthesiology. Past studies have been limited to examining maintenance and repair of anesthesia equipment,21 avoiding medication errors in pediatric anesthesia,6 and enhancing safety of propofol sedation in endoscopy.22 However, the practice of anesthesiology, which is a systems-based specialty with numerous processes that have similarities to manufacturing, lends itself to the use of FMEA to both identify potential adverse outcomes resulting from errors and to improve productivity. Table 1 illustrates categories and subcategories of anesthesia processes to which FMEA could be applied.
Table 1: Examples of Anesthesia and Perioperative Processes to which failure mode and effects analysis (FMEA) may be applied.
| Medication Safety | Equipment |
|
Allergy avoidance Ordering Administration Postadministration monitoring |
Routine check
Equipment failure Availability Emergency equipment |
| Clinical care | Hospital processes |
| Airway management
Avoid laryngospasm Prevention of PONV Perioperative pain management Surgical site infection prevention |
OR Scheduling
Patient transport Bed management OR turnover |
| Pre-operative workup | PACU processes |
| Case booking
PAT booking Consultations Labs/testing Anesthesia evaluation |
Patient monitoring
Patient evaluation PONV management Pain management |
| Regional Anesthesia | |
| Consent/Scheduling
Equipment preparation Catheter management |
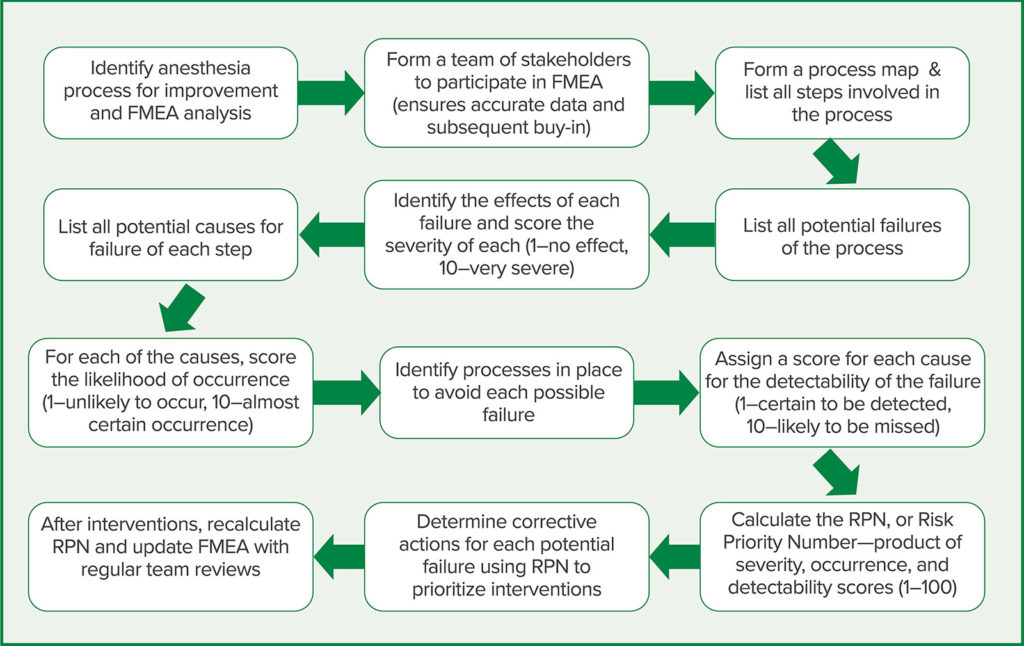
The steps involved in conducting an FMEA for an anesthesia process are demonstrated in Figure 1. The first two steps are critically important for success—namely the identification of the process for optimization and assembly of a team for involvement in the analysis and subsequent interventions. The necessary stakeholders in any complicated system must be involved to ensure adequate input during analysis so that buy-in is present when corrective actions are identified. For example, “Prevention of postoperative nausea and vomiting” is a process that likely will require corrective actions that involve the pharmacy, surgical services, and preoperative nursing, without whose participation remedies might not be successfully deployed.
The next step is also critical: Creating a list of all steps in the process. It’s usually helpful to create a process map. For each step, all potential modes of failure are listed and the possible effect of failure is recorded. Next, the severity of each failure is scored (1–least severe to 10–most severe), the potential causes for each failure are identified, and the likelihood of occurrence is scored (1–least likely to 10–near certain occurrence). Any “controls” to prevent the failure are identified and the levels of potential detection are scored (1–certain detection to 10–unlikely detection). The Risk Priority Number (RPN) is determined by multiplying the severity, occurrence, and detection scores; this number can be used by the working group to prioritize which steps to mark for corrective actions and re-evaluation. A higher RPN score indicates an area of more urgent need for intervention and process improvement, whereas a lower RPN denotes a task or step of less immediate importance.
ApPlying FMEA to Pre-Anesthesia Evaluations
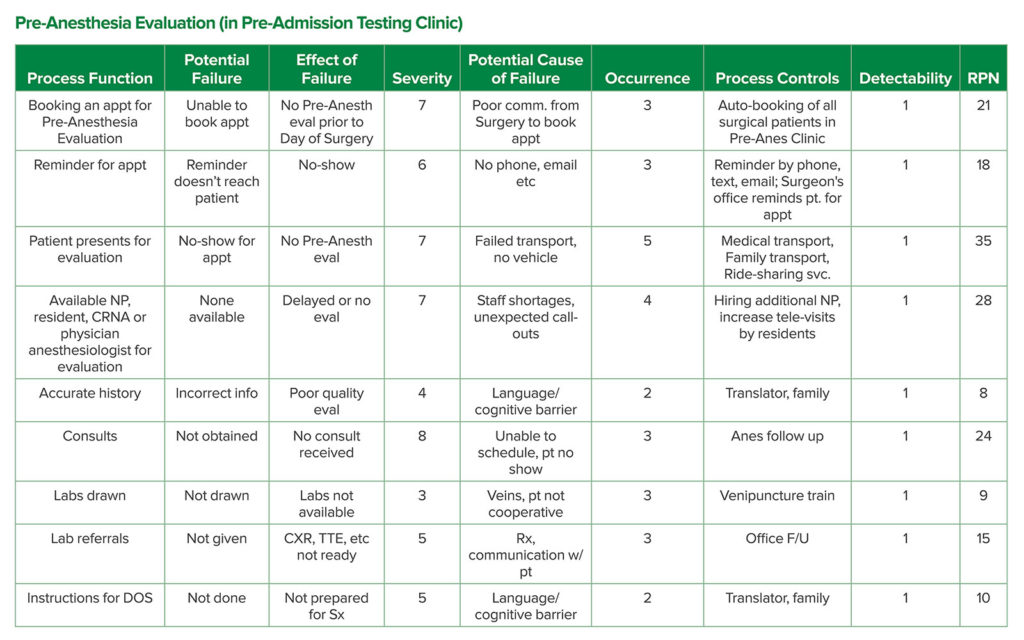
At University Hospital in Newark NJ, we performed an FMEA for the process of pre-anesthesia evaluations. Those are conducted for outpatients at the Pre-Admission Testing Clinic, who are referred for evaluation by surgeons’ offices after cases have been booked. Table 2 shows a simplified version of the FMEA analysis we conducted in the first two months of 2020 to evaluate the process. The process begins with booking an appointment in the clinic and ends with giving the patient instructions for the day of surgery. Each of the process functions are displayed in Column 1 with subsequent analysis using the steps above to calculate an RPN for each function. As shown in Table 2, the functions with the three highest RPN scores are: “Patient present for evaluation,” “Available staff,” and “Consults.” This information has allowed the senior leadership to focus efforts to make the most impact to improve the process of obtaining a thorough pre-anesthesia evaluation.
Table 2: An Example of FMEA Analysis Done at University Hospital in Newark, NJ Analyzing the Steps Involved in Obtaining a Pre-anesthesia Evaluation at the Pre-Admission Testing Clinic, Run by the Anesthesiology Department.
Severity scored 1–10 (1–least severe to 10–most severe), Occurrence scored 1–10 (1– least likely to 10–near certainty) and Detectability scored 1–10 (1–certain detection to 10–unlikely detection); RPN is the product of Severity, Occurrence, and Detectability scored 1–100 and is used to prioritize processes to avoid failure and deploy appropriate resources/manpower for improvement (highest scores given most urgent attention).
Steps that have been implemented, or are in the process of implementation, include improving patient transport to appointments and confirmation of transport with patients when booking with office staff. To address a lack of available staff to evaluate patients in clinic, an anesthesia resident is assigned for a pre-anesthesia evaluation clinic rotation to see patients in addition to the two nurse practitioners who routinely staff it. In addition, plans are being made to deploy telemedicine to replace many of the in-person evaluations, which will likely improve efficiency of visits, and relieve the strain of limited staff. Finally, we addressed possible failures in obtaining timely consults, such as cardiology to evaluate for congestive heart failure (CHF) or pulmonology to evaluate worsening or uncontrolled chronic obstructive pulmonary disease (COPD), by improving communication with the consultants’ offices and scheduling consult appointments through anesthesia, instead of relying on patients. In addition, anesthesia office staff follow up with consultants to ensure patient presence for appointments and enlist surgeons’ offices to also assist with this process.
FMEA is a powerful tool to improve health care facility processes and can be particularly effective in perioperative medicine. After deployment of each intervention and corrective action, the analysis can be repeated; rescoring of the RPN will elucidate success or failure of such actions. In addition, an updated score will allow leaders to redeploy resources including time and money to process functions that have the highest failure potential. For example, using the model in Table 2, the process function “booking in clinic” may emerge as the most significant potential failure once the three most problematic processes have been improved.
Despite its established potential for identifying risks and process failures in health care, FMEA does not appear to be as widely employed as might be expected generally and there are few applications in perioperative medicine and anesthesiology. There are several possible reasons for its lack of regular use, such as the tedious nature of the steps involved, requiring a multidisciplinary team and detailed information-gathering.23 Franklin et al. recommend a more targeted approach using FMEA, emphasizing the significance of the multidisciplinary mapping process and its potential for further analysis and intervention.23 The authors further raise a critical limitation of the RPN, in that all three variables from which the score is derived (severity, occurrence and detectability) are equally weighted, resulting in situations where RPNs may be the same for different process steps, but the underlying factors significantly consequential.23
 In 2013, Liu H-C et al. conducted an extensive review concerning FMEA use in health care and showed that the most common major shortcomings cited in the literature include not considering the relative importance of occurrence, severity, and detectability, difficulty assessing the three risk factors, inability to evaluate similar RPNs with different underlying scores, and a questionable equation used to calculate RPN amongst numerous other limitations.1 A possible alternative to FMEA may be Healthcare Failure Mode and Effects Analysis (HFMEA) developed by the National Center for Patient Safety and implemented by the VA National Center for Patient Safety.24 This approach differs from traditional FMEA by combining detectability and criticality steps of FMEA into a decision-making algorithm and replaces the RPN with a hazard score, yielding a process in which deliberation on interventions for potential failures is simpler and more responsive to user input/expertise.24
In 2013, Liu H-C et al. conducted an extensive review concerning FMEA use in health care and showed that the most common major shortcomings cited in the literature include not considering the relative importance of occurrence, severity, and detectability, difficulty assessing the three risk factors, inability to evaluate similar RPNs with different underlying scores, and a questionable equation used to calculate RPN amongst numerous other limitations.1 A possible alternative to FMEA may be Healthcare Failure Mode and Effects Analysis (HFMEA) developed by the National Center for Patient Safety and implemented by the VA National Center for Patient Safety.24 This approach differs from traditional FMEA by combining detectability and criticality steps of FMEA into a decision-making algorithm and replaces the RPN with a hazard score, yielding a process in which deliberation on interventions for potential failures is simpler and more responsive to user input/expertise.24
An important consideration when using FMEA is that hospital systems often have unique process functions that differ greatly between institutions, necessitating individualized analysis for each facility. For example, an examination of steps to prevent surgical site infections may find that surgical residents place orders for preoperative antibiotics, and that antibiotics are kept in a central drug-dispensing machine. In such a scenario, compliance with perioperative antibiotic administration requires the successful placement of the order, a nurse to check the order, the nurse to retrieve the medication and deliver it to the anesthesia team, and anesthesia to administer the medication, with numerous additional substeps and potential failures for each. This differs from many other institutions where anesthesia professionals may be responsible for determining antibiotic administration and those antibiotics are stored in anesthesia carts in the operating rooms. The mapping of an institution’s process may not translate to other facilities.
Conclusion
Although FMEA has its limitations, it is a valuable tool for proactive process analysis to improve both patient safety and optimize efficiency. Assembling a multidisciplinary team to conduct an FMEA enables leadership to focus on the most problematic and high-impact steps of a process that may fail and to assign resources to those functions to bring about corrective action. FMEA further enables a team to continually assess the usefulness of interventions and redeploy resources where they will continue to make the biggest impact. This author strongly recommends its use in anesthesiology and perioperative medical processes to assist in improving quality and safety via a systematic process to identify where attention and resources will be most effective.
George Tewfik, MD, is an assistant professor and director of Quality Assurance in the Department of Anesthesiology at Rutgers-New Jersey Medical School in Newark, NJ.
The author has no conflicts of interest.
References
- Liu H-C, Liu L, Liu N. Risk evaluation approaches in failure mode and effects analysis: a literature review. Expert Systems with Applications. 2013;40:828–838.
- Bagian JP, Gosbee J, Lee CZ, et al. The Veterans Affairs root cause analysis system in action. Jt Comm J Qual Improv. 2002;28:531–545.
- Improvement IfH. Safer patients initiative leads to reductions in mortality and adverse events in the United Kingdom. http://www.ihi.org/resources/Pages/ImprovementStories/SaferPatientsInitiativeLeadstoReductionsinMortalityandAEsintheUK.aspx. Published 2006. Accessed July 19, 2020.
- Asgari Dastjerdi H, Khorasani E, Yarmohammadian MH, et al. Evaluating the application of failure mode and effects analysis technique in hospital wards: a systematic review. J Inj Violence Res. 2017;9:51–60.
- Aranaz-Andrés JM, Bermejo-Vicedo T, Muñoz-Ojeda I, et al. Failure mode and effects analysis applied to the administration of liquid medication by oral syringes. Farm Hosp. 2017;41:674–677.
- Martin LD, Grigg EB, Verma S, et al. Outcomes of a failure mode and effects analysis for medication errors in pediatric anesthesia. Paediatr Anaesth. 2017;27:571–580.
- Pino FA, Weidemann DK, Schroeder LL, et al. Failure mode and effects analysis to reduce risk of heparin use. Am J Health Syst Pharm. 2019.
- Frewen H, Brown E, Jenkins M, O’Donovan A. Failure mode and effects analysis in a paperless radiotherapy department. J Med Imaging Radiat Oncol. 2018;62:707–715.
- Giardina M, Cantone MC, Tomarchio E, et al. A review of healthcare failure mode and effects analysis (HFMEA) in radiotherapy. Health Phys. 2016;111:317–326.
- Xu Z, Lee S, Albani D, et al. Evaluating radiotherapy treatment delay using failure mode and effects analysis (FMEA). Radiother Oncol. 2019;137:102–109.
- Castro Vida M, Martínez de la Plata JE, Morales-Molina JA, et al. Identification and prioritisation of risks in a hospital pharmacy using healthcare failure mode and effect analysis. Eur J Hosp Pharm. 2019;26:66–72.
- Stojković T, Marinković V, Jaehde U, et al. Using failure mode and effects analysis to reduce patient safety risks related to the dispensing process in the community pharmacy setting. Res Social Adm Pharm. 2017;13:1159–1166.
- Jiang Y, Jiang H, Ding S, Liu Q. Application of failure mode and effects analysis in a clinical chemistry laboratory. Clin Chim Acta. 2015;448:80–85.
- Lu Y, Teng F, Zhou J, Wen A, Bi Y. Failure mode and effect analysis in blood transfusion: a proactive tool to reduce risks. Transfusion. 2013;53:3080–3087.
- Mañes-Sevilla M, Marzal-Alfaro MB, Romero Jiménez R, et al. Failure mode and effects analysis to improve quality in clinical trials. J Healthc Qual Res. 2018;33:33–47.
- Sorrentino P. Use of failure mode and effects analysis to improve emergency department handoff processes. Clin Nurse Spec. 2016;30:28–37.
- Taleghani YM, Rezaei F, Sheikhbardsiri H. Risk assessment of the emergency processes: healthcare failure mode and effect analysis. World J Emerg Med. 2016;7:97–105.
- Yousefinezhadi T, Jannesar Nobari FA, Behzadi Goodari F, et al. A case study on improving intensive care unit (icu) services reliability: by using process failure mode and effects analysis (PFMEA). Glob J Health Sci. 2016;8:52635.
- Zhang L, Zeng L, Yan Y, et al. Application of the healthcare failure mode and effects analysis system to reduce the incidence of posture syndrome of thyroid surgery. Medicine (Baltimore). 2019;98:e18309.
- Viejo Moreno R, Sánchez-Izquierdo Riera J, Molano Álvarez E, et al. Improvement of the safety of a clinical process using failure mode and effects analysis: Prevention of venous thromboembolic disease in critical patients. Med Intensiva. 2016;40:483–490.
- Rosen MA, Lee BH, Sampson JB, et al. Failure mode and effects analysis applied to the maintenance and repair of anesthetic equipment in an austere medical environment. Int J Qual Health Care. 2014;26:404–410.
- Huergo Fernández A, Amor Martín P, Fernández Cadenas F. Propofol sedation quality and safety. failure mode and effects analysis. Rev Esp Enferm Dig. 2017;109:602–603.
- Dean Franklin B, Shebl NA, Barber N. Failure mode and effects analysis: too little for too much? BMJ Qual Saf. 2012;2:607–611.
- Safety VNCfP. The basics of healthcare failure mode and effect analysis. U.S. Dept. of Veterans Affairs. https://www.patientsafety.va.gov/docs/hfmea/HFMEAIntro.pdf. Published 2001. Accessed July 20, 2020.


 Issue PDF
Issue PDF