
![]() Dear Q&A,
Dear Q&A,
Our hospital leases several GE-Datex Aespire anesthesia machines from GE and we rely on the GE service warranty with regular visits by the GE service technician for proper care of our machines. The CO2 absorber that came with the machines is GE’s Medisorb which we continue to order from our GE supplier. Until now, we have not had a reason to consider changing to another CO2 absorbing agent. Our only volatile anesthetic is sevoflurane. In order to reduce our sevoflurane usage we are currently laying the groundwork for establishing a very-low-fresh-gas-flow (0.3 to 1.99 L/min) protocol in our anesthesia practice. We know we would like to use a CO2 absorber that is not Medisorb (75% calcium hydroxide and 3% sodium hydroxide) or similar products. We want to use an absorber with low-to-no production of Compound A and carbon monoxide under any circumstances, ideally something like Litholyme and Amsorb Plus with no reported Compound A and carbon monoxide by-products under any conditions. Much less ideally, we will reluctantly consider using other CO2 absorbers such as Medisorb EF (75% calcium hydroxide and less than 1% sodium hydroxide) and SodaSorb LF if their levels of Compound A and carbon monoxide by-products are very low and are considered“safe” or “acceptable.” Since we do not own or service our anesthesia machines, I thought it would be reasonable to pose questions about the best CO2 absorber for very-low-fresh-gas-flow anesthesia with our GE Aespire anesthesia machines directly to the GE reps and technical experts. I posed to our GE representative these general questions:
- Which CO2 absorbers can be used with GE Aespire machines?
- Which of these low-flow compatible CO2 absorbers could be obtained from our current GE parts and
supplies vendor?
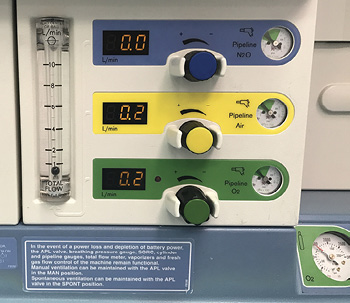
Photo of an anesthesia machine flowmeter set to deliver very-low-fresh gas flow during general anesthesia.
The information I received from GE included some sales material about GE’s Medisorb EF CO2 absorber which contains 75% calcium hydroxide and less than 1% sodium hydroxide. The sales material stated that GE Medisorb EF (when desiccated) produced less Compound A and carbon monoxide than the regular Medisorb (75% calcium hydroxide, 3% NaOH). However, no data were presented quantifying the levels of Compound A and carbon monoxide by-products with Medisorb EF and plain Medisorb vs. other CO2 absorber products. I was also provided with a July 2013 memo from a GE Director of Commercial Marketing indicating that GE anesthesia machines could only use GE-validated and GE-compatible parts and accessories, like Medisorb and Medisorb EF CO2 absorbers. The memo indicated the GE service warranty is only valid if GE-validated and GE-compatible products (like Medisorb) were used with the GE anesthesia machines. The memo did not specifically state that other CO2 absorber products (Litholyme, Amsorb, Amsorb Plus, etc.) were not GE-validated, -compatible, or -approved. It did not state that only GE Medisorb products could be used with a GE anesthesia machine. I was also informed that the Director of Commercial Marketing who penned the memo is no longer with GE.
In an effort to get a more definitive answer, I am posing these questions:
- Which CO2 absorber products are “safe” and “adequate” for very-low-fresh-gas-flow (0.3 to 1.99 L/min) general anesthesia?
- Which CO2 absorber products are “ideal”or “best suited” for very-low-fresh-gas-flow (0.3 to 1.99 L/min) general anesthesia?
- Which CO2 absorber products on the market are compatible with GE Aespire anesthesia machines?
- Do you know of any instances where a GE anesthesia machine service warranty was voided because a non-GE or non-Medisorb CO2 absorber was used?Robert Branche, MD
Phoenix, AZ
Table 1. A variety of CO2 absorbents and the corresponding lifespan (hours)
<tr “>Brand nameDistributorNaOH content (vol%)Amount of absorbent in canister (gram)Canister life (hours)*Absorbent life (hours/100 g)
| Amsorb Plus | Armstrong M | 0 | 821 | 10.6 | 1.29 |
| LoFloSorb | Intersurgical | 0 | 915 | 12.8 | 1.39 |
| Medisorb EF | CareFusion | < 2.5 | 721 | 9.9 | 1.37 |
| Medisorb | CareFusion | 2.5 | 796 | 15.0 | 1.88 |
| SpheraSorb | Intersurgical | 2.5 | 1057 | 15.6 | 1.47 |
| LithoLyme | Allied HC | 0 ** | 1010 | 16.0 | 1.58 |
| SpiraLith | Micropore | 0 *** | 569 | 18.8 | 3.31 |
* Exhaustion defined as FICO2 = 0.5%, and tested with Aisys machine, fresh gas flow 350 mL/min, CO2 load 160 mL/min
** LiCl as catalyst
*** Uses LiOH instead of Ca(OH)2
![]() Dear Dr. Branche,
Dear Dr. Branche,
You raise interesting and timely questions as the economic and environmental impacts of inhaled anesthetics are well known, but the optimal approach to minimizing those impacts is not obvious. We will do our best to answer your questions recognizing that some of the information is incomplete.
1. Which CO2 absorber products are “safe” and “adequate” for very-low-fresh-gas-flow (0.3 to 1.99 L/min) general anesthesia?
The safety concern with low-flow anesthesia is the impact of anesthetic degradation by CO2 absorbents leading to Compound A production in the case of sevoflurane, CO in the presence of desiccated absorbents and reduced anesthetic concentrations. It is clear from the literature that absorbents containing strong bases like potassium hydroxide (KOH) and sodium hydroxide (NaOH) are the most likely to result in anesthetic degradation, especially when dehydrated.1 It is interesting to note that even Baralyme and Classic Soda Lime which contain 2.6% and 4.6% KOH, respectively, do not produce CO if they are not desiccated. In one of the original studies on this topic, published before new absorbent formulations were available, Fang et al. recommended using fresh gas inflow rates less than 2–3 L/min with soda lime or Baralyme to ensure that
the absorbent did not desiccate and produce CO.2 The trend in absorbent formulations has focused on eliminating the KOH which has been found to be the worst offender in terms of CO and Compound A
production.3,4
Given this background, it is easy to recommend avoiding absorbents that contain KOH which has been eliminated from most formulations on the market. One is then left with selecting from absorbents that are either calcium hydroxide (Ca(OH)2) with or without small concentrations of NaOH added, or lithium hydroxide (LiOH). Keijzer et. al. studied seven different absorbents, both hydrated and desiccated, for the potential to produce Compound A and CO in the presence of sevoflurane.5 Six of the absorbents studied were primarily calcium hydroxide although three of them also contained an extremely small amount of KOH (0.003%) and varying amounts of NaOH (1.5–3%). The seventh consisted only of LiOH. They found that CO was only produced by dessicated absorbents containing NaOH. Compound A was produced by the absorbents containing NaOH in both hydrated and desiccated forms. One of the pure Ca(OH)2 absorbents produced Compound A when desiccated as did the LiOH absorbent.
Low-flow techniques have the advantage of preserving moisture in the absorbent and reducing the chance of desiccation which would reduce the concern for CO production. That said, it is possible that desiccation can occur if for example, a machine is left after emergence with a high fresh gas flow, and a more comfortable recommendation would recognize that possibility. It is easy to advocate for absorbents that do not have any KOH or NaOH, i.e., absorbents with Ca(OH)2 and LiOH only, as CO production would not be a concern, desiccated or not. These absorbents would definitely be safe. Since your question focused on the use of sevoflurane, Compound A production is another concern. The data from Keijzer indicates that even absorbents without a strong base have the potential to produce Compound A when dessicated. The clinical relevance of Compound A production remains to be demonstrated and should not be a primary consideration when selecting an absorbent. Indeed, NaOH containing Ca(OH)2 absorbents are routinely used outside the US during closed-circuit anesthesia without concern for, nor reports of, patient harm. Ca(OH)2 and LiOH absorbents with lower concentrations of NaOH and minimal to no KOH should be both safe and adequate for use with the fresh gas flows you propose especially since desiccation is less likely at low flows since moisture is preserved.
2. Which CO2 absorber products are “ideal” or “best suited” for very-low-fresh-gas-flow (0.3 to 1.99 L/min) general anesthesia?
This question adds another dimension to selecting the CO2 absorbent. As fresh gas flows are reduced, more exhaled gas is rebreathed, more CO2 must be absorbed, and CO2 absorbent cost will increase. The ideal or best suited absorbent would be the lowest cost material that does not put the patient at risk from degradation of anesthetics. Evaluating the cost difference between absorbents can be complex. Factors to consider include the cost of a pre-filled canister or loose fill of a CO2 absorbent canister, the intrinsic efficiency of the absorbent to absorb CO2, the total fresh gas flow, which will determine the degree of rebreathing and the CO2 production of the patient(s).
The intrinsic efficiency of the absorbent to absorb CO2 can be determined by measuring the quantity of CO2 that can be absorbed per 100 g of absorbent material. To be meaningful, this measurement should be done by simulating clinical conditions, which will include the potential to leave some of the absorbent material unused when the canister is changed due to channeling and lack of exposure to CO2.
There are some data that shed light on the relative efficiency of different absorbent materials to absorb CO2.6 In a recent in-vitro study using an AISYS anesthesia machine, Hendrickx et. al. evaluated the relative ability to absorb CO2 for seven different absorbent materials in pre-filled canisters. Absorbents tested included six Ca(OH)2 based materials with either no NaOH or varying amounts of NaOH added, and one that is pure LiOH. (Table 1). The anesthesia ventilator was set to ventilate a simulated lung at 5 L/min with 160 mls/min of CO2 supplied to the “lung” to simulate CO2 production. Total fresh gas flow was set to 350 mls/min of an O2 and Air mixture which would be consistent with significant rebreathing of exhaled gas in adult patients. Continuous capnography was used, and the time required to reach an FiCO2 of 0.5% (3-4 mmHg) was measured.
Given the standardized testing conditions, the best information for identifying the relative efficiency of the different absorbent canisters tested is the absorbent life in hours per 100 g of material. LiOH was found to be the most efficient absorbent on a weight basis with almost double the duration of effect per 100 g of material than the next closest absorbent. Of the remaining absorbents tested, the presence of NaOH or LiCl clearly improved efficiency, with the pure Ca(OH)2 absorbents showing the shortest duration per 100 g of material. The most efficient absorbent material is not, however, always the least costly. Local pricing determines the cost per absorbent canister and although LiOH was found to be the most efficient, soaring lithium prices will likely make it cost-prohibitive. Ultimately, the cost impact of utilizing more CO2 absorbent at low flows will be determined by a combination of the efficiency of the material and the local pricing. Less efficient absorbent materials will need to be available at a lower cost to be as effective as the more efficient materials.
Another strategy to reduce the cost of absorbent materials at low flows is to change the material based upon the presence of inspired carbon dioxide rather than an indicator change. As the absorbent material becomes completely saturated, inspired CO2 will begin to rise. The cause can easily be diagnosed by increasing fresh gas flow to exceed minute ventilation which should eliminate rebreathing and any measured inspired CO2. Picking a threshold for changing the canister based upon measured inspired CO2 will ensure absorbent material is used as completely as possible before changing.
3. Which CO2 absorber products on the market are compatible with GE Aespire anesthesia machines?
(NOTE: The APSF Committee on Technology is fortunate to have Kevin Tissot, Chief Engineer for the Anesthesia and Respiratory Care business at GE Healthcare, as a member of the committee to respond to this question.)
GE offers a reusable absorber canister that can be bulk filled with whatever absorbent material the customer may choose. GE also offers disposable (pre-filled) canisters of absorbent material.
Using canisters that are not sold by GE does not void your warranty. However, some dimensions of the canisters are important to prevent leaks and ensure proper operation of the CO2 bypass mechanism. Clearly, we test anything that we sell to make sure the dimensions are correct. We also work with other companies if we become aware of problems with their products, to encourage them to make
corrections.
4. Do you know of any instances where a GE anesthesia machine service warranty was voided because a non-GE or non-Medisorb CO2 absorber was used?
See the response above.
Jeffrey Feldman, MD, MSE
Interim Chair, APSF Committee on Technology
Professor of Clinical Anesthesiology
Children’s Hospital of Philadelphia
Perelman School of Medicine
Philadelphia, PA
Jan Hendrickx, MD, PhD
Dept. of Anesthesiology/CCM
OLV
Hospital
Aalst, Belgium
Dr. Feldman serves as a member of the Clinical Advisory Board, ClearLine MD, Boston, MA. Dr. Feldman has received consulting compensation from Draeger Medical, GE Medical, and Medtronic.
Dr. Hendrickx has received lecture support, consulting fees, equipment loans, or travel reimbursements from the following companies: AbbVie, Acertys, Aguettant, Air Liquide, Allied Healthcare, Armstrong Medical, Baxter, Draeger, evoked, GE, Hospithera, Heinen und Lowenstein, Intersurgical, Maquet, MDMS, MEDEC, Micropore, Molecular, MSD, NWS, Orion Pharma, Pall, Piramal, Philips, Quantium Medical, Sedana.
References:
- Karasch ED, Powers KM, Artru AA, et al. Comparison of Amsorb®, Sodalime, and
Baralyme® degradation of volatile anesthetics and formation of carbon monoxide and compound A in swine in vivo. Anesthesiology 2002;96:173–82. - Fang ZX, Eger EL, Laster MJ, et al. Carbon monoxide production from degradation of desflurane, enflurane, isoflurane, halothane and sevoflurane by soda lime and Baralyme®. Anesth Analg 1995;80:1187–93.
- Neumann MA, Laster MJ, Weiskopf RB, et al. The elimination of sodium and potassium hydroxides from desiccated soda lime diminishes degradation of desflurane to carbon monoxide and sevoflurane to compound A but does not compromise carbon dioxide absorption. Anesth Analg 1999;89:768–73.
- Yamakage M, Yamada S, Chen X, et al. Carbon dioxide absorbents containing potassium hydroxide produce much larger concentrations of compound A from sevoflurane in clinical practice. Anesth Analg 2000;91:220–4.
- Keijzer C, Perez RS, de Lange JJ, et al. Compound A and carbon monoxide production from sevoflurane and seven different types of carbon dioxide absorbent in a patient model. Acta Anaesthesiol Scand 2007;51:31–7.
- Hendrickx JF, De Ridder SP, Dehouwer A, et al. In vitro performance of prefilled CO2
absorbers with the Aisys.® J Clin Monit Comput 2016;30:193–202.
This article does not reflect the opinion of the editors or the APSF. The information provided is for safety-related educational purposes only, and does not constitute medical or legal advice. Content is provided for purposes of education or discussion, and comprises neither statements of advice nor the opinions of the APSF. It is not the intention of the APSF to provide specific medical or legal advice or to endorse any specific views or recommendations. In no event shall the APSF be responsible or liable, directly or indirectly, for any damage or loss caused or alleged to be caused by or in connection with the reliance on any such information.


 Issue PDF
Issue PDF