| Disclaimer: Viewers of this material should review the information contained within it with appropriate medical and legal counsel and make their own determinations as to relevance to their particular practice setting and compliance with state and federal laws and regulations. The APSF has used its best efforts to provide accurate information. However, this material is provided only for informational purposes and does not constitute medical or legal advice. These articles also should not be construed as representing APSF endorsement or policy (unless otherwise stated), making clinical recommendations, or substituting for the judgment of a physician and consultation with independent legal counsel. |
Introduction
 The COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) continues to have a profound impact on life across the globe and has placed an enormous strain on health care systems and economies, including with likely untold psychological and social implications. The outbreak of SARS-CoV-2, which originated in Wuhan, China, rapidly progressed to become a pandemic and has now spread to over 150 countries, infecting over 3.1 million people, as of April 29, 2020, with over 1 million cases in the United States alone.1,2
The COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) continues to have a profound impact on life across the globe and has placed an enormous strain on health care systems and economies, including with likely untold psychological and social implications. The outbreak of SARS-CoV-2, which originated in Wuhan, China, rapidly progressed to become a pandemic and has now spread to over 150 countries, infecting over 3.1 million people, as of April 29, 2020, with over 1 million cases in the United States alone.1,2
Current estimates suggest a fatality rate ranging from 2 to 20% for hospitalized patients, and up to 88% for those requiring mechanical ventilation.3–5 SARS-CoV-2 has an estimated basic reproductive number (R0) of 2.2–2.7,6 which means a single infected person has the potential to spread infection to more than 2 susceptible individuals. This can lead to rapid, exponential spread, which we have now seen within communities across the US.7
Given the capacity for human-to-human transmission,8–10 SARS-CoV-2 continues to pose a high risk to all health care professionals in the perioperative setting. We implore perioperative and hospital leaders to develop strategic steps for interventions on patients who have suspected or confirmed COVID-19 infection. The purpose of this communication is to present prudent safety measures in the perioperative setting, recognizing that these measures are based on learning from the current outbreak as well as from previous viral outbreaks.11 Specifically, we address those measures which resulted in the success or failure of curtailing transmission of viral pathogens (SARS-CoV-2, SARS-CoV, and Middle Eastern Respiratory Syndrome Coronavirus [MERS-CoV]) in health care settings. While nonpharmacological interventions remain the mainstay in curtailing the spread of disease, global experiences highlight the prominent role of prompt public health measures in combating a pandemic of this magnitude.
SARS-CoV-2 Pathogen Transmission
Pathogen transmission can occur between humans via inhalation of infected respiratory droplets, in particular if the exposure of droplets is within close proximity (6 feet) or if you are in a relatively closed-off environment with continuous exposure to high aerosol counts.12,13 Transmission can also occur through close contact, either directly or indirectly, with mucous membranes (i.e., eyes, nose, mouth) and through the digestive tract.12,14 There is now evidence to suggest that transmission may occur from direct or indirect contact with contaminated surfaces (fomites) and this may predispose to subsequent self-inoculation and/or transmission. Similar to other coronaviruses, SARS-CoV-2 is able to survive outside the body for approximately 12 hours (fabrics, cardboard surfaces) and up to 72 hours (plastic or metal surfaces).11,15,16
Preventing transmission of the SARS-CoV-2 remains the most effective public health effort to lessen its impact. This effort involves rapid identification of cases, tracing of contacts, isolation/quarantine of infected/exposed individuals, and supportive care. We recognize the perioperative setting as a site for possible unrecognized exposure to SARS-CoV-2; therefore, hospital-wide guidelines should be available for health care professionals to manage exposure and implement measures to mitigate transmission.
Lessons Learned from Previous Coronavirus Outbreaks (SARS-CoV, MERS)
We learned from the Toronto SARS-CoV outbreak in 2002 and the MERS-CoV outbreak in 2012 that the majority of cases were associated with nosocomial transmission, in particular amongst health care workers (HCWs) exposed to aerosol-generating procedures.17 Despite existing safety protocols, confirmed SARS-CoV infection of HCWs was associated with the intubation of a confirmed SARS-CoV infected patient in the ICU, if more than one attempt at intubation was required or when more than three people were in the room.18 Additional risk factors included patient contact during aerosolizing procedures including via nebulizers, CPAP, BiPAP, or high flow nasal oxygen therapy.11 However, improved measures and adherence to PPE reduced nosocomial transmission during the second wave of the SARS-CoV outbreak in Toronto. More recent data suggest high flow nasal oxygen may not augment aerosol spread during spontaneous coughing in healthy volunteers.19
Lessons Learned from the Current Outbreak (SARS-CoV-2):
Experience from China, Italy, the United Kingdom, and the United States makes it abundantly clear that community transmission is responsible for the majority of infected patients.1 Disease prevalence remains high in various parts of the country, with a lack of widely available and reliable testing posing a risk of nosocomial transmission in the perioperative setting. The period immediately prior to symptom onset is associated with SARS-CoV-2 viral shedding and represents a considerable transmission potential, further implicating all (asymptomatic) patients as an additional risk.20,21 To protect and ensure the safety of HCWs, and by extension, patients, preventing nosocomial transmission of SARS-CoV-2 requires a coordinated effort and complete organizational support.22
Due to the rapid spread of COVID-19, the ability of health care organizations to prepare for increasing admissions and implement risk mitigation strategies has been time-pressured. Anxiety and fear placed additional pressure on providers, in particular due to concerns of inadequate supplies of personal protective equipment (PPE) and a lack of clarity of information or unified thinking amongst leaders. We’ve learned that discordant messages cause confusion, create tension, and slow protocol implementation. Furthermore, keeping up with rapidly changing guidelines and communicating them clearly to an entire organization is challenging. We recommend a unified approach to supporting and communicating with members of staff within your organization.
Pathogen Transmission in the OR and Around the Anesthesia Work Environment
Within the operating room (OR), the anesthesia work environment allows for numerous surfaces that can harbor droplets, thus serving as reservoirs for the virus if proper droplet precautions or proper decontamination processes are not followed. As noted previously, processes that favor aerosolization of sputum an infected individual in the perioperative setting represents a potential source of exposure to HCWs. For the anesthesia professional and intensivist, attention should be given to the time periods during intubation and extubation, as these represent the highest risk of exposure and involve direct contact with respiratory droplets during airway management.23,24
Areas immediately outside the OR and around the operating department complex represent low-risk areas with regards to aerosol generation, but may still be potential sources for transmission. Irrespective of location, inadequate PPE, improper use of PPE, and poor hand hygiene are potential factors that can lead to transmission to the bedside HCW.25,26
Recommendations for the Perioperative Practice of Anesthesia in Patients with COVID-19
Due to the potential for transmission of SARs-CoV-2 in asymptomatic patients and HCWs, we recommend an escalation of standard practice during the perioperative management of all patients to reduce exposure to secretions.
Hand Hygiene:
Frequent hand washing is one of the most important hygiene measures to protect against cross infection and must be actively enforced. Alcohol-based hand wash gels should be located on or near every anesthesia workstation. Hand hygiene (HH) should be meticulously performed according to standard guidelines, specifically after removing gloves; after contact with soiled or contaminated areas; before touching the anesthesia machine, the anesthesia cart or its contents; and after every contact with the patient (e.g., placement of thermometer, nasogastric tube).
Personal Protective Equipment:22,27,28
Personal protective equipment should be available for all providers and should include an N95 respirator (or equivalent) or a powered air-purifying respirator (PAPR), eye protection such as goggles or a face shield, a disposable head cover, an impermeable fluid-resistant gown, shoe covers, and two sets of gloves. Disposable OR caps reduce the risk of contaminating hands by touching hair which may have been exposed to droplets. Hand washing is essential before donning and after doffing of PPE.
N95 masks fulfill the filtering efficiency criteria of the National Institute for Occupational Safety and Health (NIOSH) and are approved for protection against droplet and airborne transmission of 95% of particles greater than 0.3 microns in size. N95 masks, which must be fit tested, offer protection against the contact and droplet spread of the coronavirus. Alternatively, a PAPR may be used instead of an N95 respirator. This provides equivalent protection to an N95, but may offer greater versatility for use across various face sizes, in the presence of facial hair, or in multiple-use scenarios. Bear in mind that a PAPR may be more cumbersome to don and doff without self-contamination, and therefore, careful observation by a colleague may mitigate this risk. At a minimum, N95 respirators or their equivalent should be used for all known or suspected cases of COVID-19.
Providers and their organizations should review protocols for correct donning and doffing of PPE. Consider conducting mock intubation/extubation drills using PPE in a real environment (in situ). This is an opportunity to promote correct use of PPE among providers and to identify barriers to adherence. Consideration at the organization level should be taken to avoid ‘’rescue like’’ crash intubations where PPE cannot be fully adhered to.
Airway Manipulation (Intubation and Extubation):
 Prior to exposure to an aerosolizing procedure or airway management, HCWs should protect themselves by donning the appropriate PPE, described above. During intubation and extubation, limit the number of staff members present inside the room to reduce the risk of unnecessary exposure, unless staff members are donned in the appropriate PPE. Ensure that a plan for an unanticipated difficult airway has been discussed and the desired rescue equipment is immediately available, including a supraglottic airway and a surgical airway kit.
Prior to exposure to an aerosolizing procedure or airway management, HCWs should protect themselves by donning the appropriate PPE, described above. During intubation and extubation, limit the number of staff members present inside the room to reduce the risk of unnecessary exposure, unless staff members are donned in the appropriate PPE. Ensure that a plan for an unanticipated difficult airway has been discussed and the desired rescue equipment is immediately available, including a supraglottic airway and a surgical airway kit.
Prepare intubating equipment in close proximity to the patient, and plan for its disposal in a manner that limits the distance of travel of contaminated equipment. Consider using the double gloving technique during intubation, sheathing the laryngoscope blade with your outer gloves immediately following intubation. Alternatively, place the used laryngoscope directly into a sealed bag and then remove your outer layer of gloves.25
Extubation often results in greater aerosol generation compared to intubation and should be performed with strict adherence to PPE, as described above. Ensure that other HCWs in the room (e.g., respiratory therapist and nurse) also wear PPE. Consider the use of gauze or a protective cloth barrier to cover the mouth and nose during extubation. Carefully dispose of contaminated equipment. Strongly consider prophylactic antiemetics to reduce the risk of vomiting and possible viral spread.
Perioperative Workflow Planning and Simulation Training:
Review the need for specific perioperative workflows for the management of COVID-19 patients within your organization.29 This may require workflow redesign, checklist implementation, and testing in real time to reveal hazards or gaps in care. Designate specific ORs for COVID-19 patients and minimize contamination by removing unneeded contents and applying plastic coverings to nonmobile equipment. We recommend team training through in-situ simulation drills to promote awareness of perioperative changes for COVID-19 patients and encourage the development of a shared mental model amongst health care teams.30 Simulation training in donning and doffing PPE, intubating, extubating, and managing an adverse event in a COVID-19 patient is also recommended. Some of the authors’ institutional online resources are available at: https://www.anesthesiaeducation.net/qsi_covid19/.
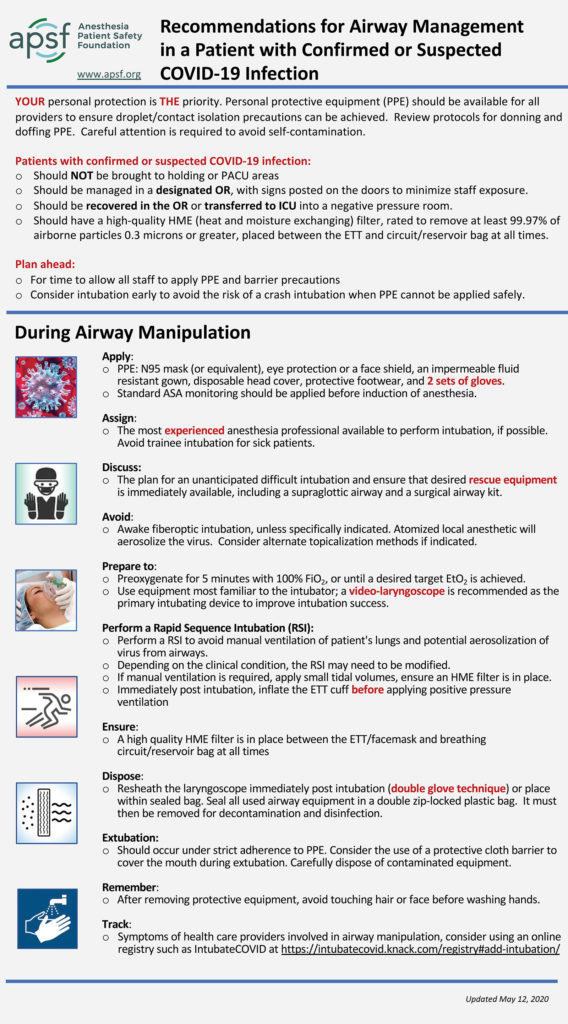
Recommendations for Airway Management in a Patient with Suspected or Confirmed Coronavirus (SARS CoV-2) Infection
General Precautions:
- Your personal protection is the priority. Personal protective equipment (PPE) should be available to all providers to ensure airborne/droplet/contact isolation precautions can be achieved. Review protocols for donning and doffing PPE. Plan ahead in order to allow sufficient time for staff to apply PPE and barrier precautions. Careful attention is required to avoid self-contamination.
- Confirmed or suspected SARS CoV-2 infected cases should NOT be brought to holding or PACU areas. A designated OR should be allocated for such cases and signs posted on the doors to minimize staff exposure. Infected cases should be recovered in the operating room or transferred to ICU into a negative pressure room. Have a clamp ready for circuit disconnections.
- Ensure that sufficient equipment for airway manipulation and contingencies are available. In addition, make sure that a high quality HME (Heat and Moisture Exchanging) filter, rated to remove at least 99.97% of airborne particles 0.3 microns or greater, and an endotracheal tube-clamp are available before proceeding with intubation.
During Airway Manipulation:
- Apply a fit-tested disposable N95 respirator, PAPR, or an equivalent mask, eye protection, gown, 2 sets of gloves, and protective footwear. Apply standard monitoring to the patient, as you would for any induction of anesthesia.
- Designate the most experienced anesthesia professional available to perform intubation, if possible. Avoid trainee intubations of suspected or confirmed SARS CoV-2 infected cases during this time.
- Discuss the plan for an unanticipated difficult airway and ensure that desired rescue equipment is immediately available, including a supraglottic airway and a surgical airway kit.
- Avoid awake fiberoptic intubations unless specifically indicated. Atomized local anesthetic will aerosolize the virus, so alternate topicalization techniques should be used if this procedure is indicated. Use equipment most familiar to the intubator; a video-laryngoscope is recommended as the primary intubating device to improve intubation success.31
- Preoxygenate for a minimum of 5 minutes with 100% oxygen, or until a desired target end tidal O2 is achieved.
- Perform a rapid sequence induction (RSI) in order to avoid manual ventilation of patient’s lungs. Ensure a skilled assistant is available to perform cricoid pressure. If manual ventilation is required during a modified RSI, apply small tidal volumes, ensuring an HME filter is in place.
- Immediately following intubation, inflate the ETT cuff, before applying positive pressure ventilation.
- Ensure the placement of a high quality HME filter between the facemask/endotracheal tube and breathing circuit or reservoir bag at all times.
- Resheath the laryngoscope immediately post intubation or place within a sealed specimen bag. Seal all used airway equipment in a double zip-locked plastic bag. The used airway equipment must then be removed for decontamination and disinfection.
- Extubation should occur under strict adherence to PPE. Consider the use of a protective cloth barrier to cover the mouth and nose during extubation. Carefully dispose of contaminated equipment.
- After removing protective equipment, remember to avoid touching your hair or face before washing hands.
- Consider tracking symptoms in health care workers involved in airway manipulation of a COVID-19 patient, at a local level or using an online platform such as the https://intubatecovid.org registry.
Recommendations for Resuming Nonurgent or Elective Perioperative Services
As health systems begin planning to resume nonurgent operative cases, and subsequently, elective cases with ongoing flattening of the SARS-Cov2 infection curve, it remains critical to continue to adhere to the highest evidence-based standards, from local, national, and international guidelines, in order to protect patients and HCWs. Resurgence of COVID-19 remains a strong possibility and concern for a multitude of reasons, including variations in testing availability, lack of clarity on immunity conferred by prior exposure, prevalence of disease, etc.32 Therefore, the need for ongoing surveillance, with emphasis on continuous public efforts, should be encouraged.
In anticipation of reopening nonurgent/elective perioperative services, we recommend careful institutional planning with a slow, phased resumption of nonurgent cases, as suggested in the Joint Statement from the American College of Surgeons (ACS), American Society of Anesthesiologists (ASA), American Hospital Association (AHA), and Association of Perioperative Registered Nurses (AORN) (Roadmap for Resuming Elective Surgery after COVID-19 Pandemic).33 Institutional policies and workflows for resuming nonurgent/elective cases should take into consideration testing availability, local disease prevalence, surgical procedure and indication, hospital and ICU capacity, and staffing requirements. Physical workspaces should be mapped out to optimize patient and provider distancing. Provisions should continue to be made for ongoing staff training and support for the overall hospital response to COVID-19.34 In accordance with the joint statement above, we advocate for a phased approach to resuming medically indicated, time-sensitive surgeries.34–36 We favor policies and protocols that prioritize patients’ clinical needs and organizational capacity as a way to mitigate the competition for limited operating capacity.
The cornerstone of risk management during pandemic recovery will remain symptom-based preoperative screening. Most hospitals have a dedicated service to ensure that symptom-positive patients have a clear pathway for delaying surgery and follow-up in 14 days where possible.
Recommendations for Preoperative Testing
Preoperative testing is being implemented across the world with three main goals. They are
- Delay elective surgery in patients who are either symptomatic or test positive.
- Trigger perioperative protocols for the appropriate care of suspected or confirmed COVID-19.
- Guide appropriate use of PPE and perioperative care protocols.
We support the recommendations issued in a joint statement by the ASA and APSF (ASA and APSF Joint Statement on Perioperative Testing for the COVID-19 Virus).37 A population risk assessment identifying the prevalence of SARS-CoV-2 should be reviewed.
When There is Local or Regional Presence of SARS-CoV-2:38
- All patients should be screened for symptoms prior to presenting to the hospital. Patients reporting symptoms should be referred for additional evaluation. All other patients should undergo nucleic acid amplification testing (including PCR tests) prior to undergoing non-emergent surgery. Health care systems may consider encouraging patients to self-isolate pending testing results.
- Because false negatives may occur with testing, droplet precautions (surgical mask and eye covering) should be used by OR staff for operative cases. Before performing an aerosol-generating procedure, health care providers within the room should wear an N95 mask, eye protection, gloves, and a gown.
- If a patient tests positive for SARS-CoV-2, elective surgical procedures should be delayed until the patient is no longer infectious and has demonstrated recovery from COVID-19. A patient may be infectious until either:
- CDC-recommended test-based strategy
- Resolution of fever without the use of fever-reducing medications
- Improvement in respiratory symptoms
- Negative results from two SARS-CoV-2 tests ≥ 24 hours apart
- CDC non-test-based strategy
- At least 72 hours since resolution of fever, without the use of fever-reducing medications, and improvement in respiratory symptoms
- At least 7 days since symptoms first appeared.
- CDC-recommended test-based strategy
- Recommendations regarding the definition of sufficient recovery from the physiologic changes from SARS-CoV-2 cannot be made at this time; however, evaluation should include an assessment of the patient’s exercise capacity (metabolic equivalents or METS).
When There is Little or No Regional Presence of SARS-CoV-2:
- All patients should be screened for symptoms before presenting to the hospital.
- Patients reporting symptoms should be referred for further evaluation.
Comment
Without any current vaccinations or proven pharmacological interventions, we recommend continuous emphasis on public health efforts and nonpharmacological interventions endorsed by the Center for Disease Control (CDC), World Health Organization (WHO), and local state governments. We also advocate for the continuous leveraging of technology (telemedicine) in the perioperative setting to facilitate adequate social distancing and mitigate nosocomial transmissions.39
Dr. Liana Zucco is a perioperative quality & safety fellow in Anesthesiology at the Beth Israel Deaconess Medical Centre and a Master’s in Healthcare Quality & Safety candidate at Harvard Medical School, Boston, MA.
Dr. Nadav Levy is a perioperative quality & safety fellow in Anesthesiology at the Beth Israel Deaconess Medical Centre and a Master’s in Healthcare Quality & Safety candidate at Harvard Medical School, Boston, MA.
Dr. Desire Ketchandji is a critical care medicine fellow in Anesthesiology at Oregon Health and Science University, Portland, OR.
Dr. Michael Aziz is the interim vice chair of Clinical Affairs and professor in the Department of Anesthesiology and Perioperative Medicine at Oregon Health and Science University, Portland, OR.
Dr. Satya Krishna Ramachandran is the vice chair of Quality, Safety and Innovation, associate professor of Anesthesia, Department of Anesthesia, Critical Care and Pain Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA.
Drs. Zucco, Levy, Ketchandji and Aziz have no conflicts of interest. Dr. Ramachandran receives personal fees from Fresenius Kabi USA (scientific advisor).
References
- World Health Organization (WHO). Coronavirus disease situation reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed April 29, 2020.
- John Hopkins University. COVID-19 Dashboard by the Centre for Systems Science and Engineering. Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html. Published 2020. Accessed April 29, 2020.
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;10022:1–8.
- Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;4720:2019–2021.
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069.
- Sanche S, Lin Y, Xu C, et al. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020. https://doi.org/10.1101/2020.02.07.20021154
- Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936.
- Fuk-Woo Chan J, Yuan S, Kok K-H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;6736:1–10.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan , China. Lancet. 2020;6736:1–10.
- Phan LT, Nguyen TV, Luong QC, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;(Panel D). doi:10.1056/NEJMc2001272
- Kamming D, Gardam M, Chung F. Editorial I. Anaesthesia and SARS. Br J Anaesth. 2003;90:715–718.
- Li H, Liu S-M, Yu X-H, et al. Coronavirus disease 2019 (COVID-19): current status and future perspective. Int J Antimicrob Agents. 2020;2019(xxxx):105951. doi:10.1016/j.ijantimicag.2020.105951
- Centers for Disease Control and Prevention. Cleaning and disinfection for households. Coronavirus Disease 2019 (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cleaning-disinfection.html. Accessed May 8, 2020.
- Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109(February):102433. doi:10.1016/j.jaut.2020.102433
- van Doremalen N, Bushmaker T, Morris D, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2010;382:1564-1567:
- Chen YC, Huang LM, Chan CC, et al. SARS in hospital emergency room. Emerg Infect Dis. 2004;10:782–788.
- Booth CM, Matukas LM, Tomlinson GA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. J Am Med Assoc. 2003;289:2801–2809.
- Caputo KM, Byrick R, Chapman MG, et al. Intubation of SARS patients: infection and perspectives of healthcare workers. Can J Anesth. 2006;53:122–129.
- Iwashyna TJ, Boehman A, Capelcelatro J, et al. Variation in aerosol production across oxygen delivery devices in spontaneously breathing human subjects. medRxiv. 2020:2020.04.15.20066688. doi:10.1101/2020.04.15.20066688
- He X, Lau EH, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. medRxiv. 2020:2020.03.15.20036707. doi:10.1101/2020.03.15.20036707
- Spicer K, Bardossy AC, Oakley LP, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. NEJM: April 24, 2020:1–10. DOI: 10.1056/NEJMoa2008457
- Ferioli M, Cisternino C, Leo V, et al. Protecting healthcare workers from SARS-CoV-2 infection: practical indications. Eur Respir Rev. 2020;29:200068.
- Rowlands J, Yeager MP, Beach M, et al. Video observation to map hand contact and bacterial transmission in operating rooms. Am J Infect Control. 2014;42:698–701.
- Loftus RW, Koff MD, Birnbach DJ. The dynamics and implications of bacterial transmission events arising from the anesthesia work area. Anesth Analg. 2015;120:853–860.
- Munoz-Price LS, Bowdle A, Johnston BL, et al. Infection prevention in the operating room anesthesia work area. Infect Control Hosp Epidemiol. 2019;40:1–17.
- Birnbach DJ, Rosen LF, Fitzpatrick M, et al. A new approach to pathogen containment in the operating room: sheathing the laryngoscope after intubation. Anesth Analg. 2015;121:1209–1214.
- Seto WH, Tsang D, Yung RWH, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet. 2003;361:1519–1520.
- ASA, APSF, AAAA, AANA. The use of personal protective equipment by anesthesia professionals during the COVID-19 pandemic. Anesthesia Patient Safety Foundation. https://www.apsf.org/news-updates/the-use-of-personal-protective-equipment-by-anesthesia-professionals-during-the-covid-19-pandemic/. Accessed on April, 20, 2020.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth. 2020. doi:10.1007/s12630-020-01591-x
- Dieckmann P, Torgeirsen K, Qvindesland SA, et al. The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: practical tips and resources from Norway, Denmark, and the UK. Adv Simul (London, England). 2020;5:3.
- Cook TM, El-Boghdadly K, McGuire B, et al. Consensus guidelines for managing the airway in patients with COVID-19. Anaesthesia. 2020:1–15.
- Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science (80- ). April 2020:eabb5793. doi:10.1126/science.abb5793
- ACS, ASA, AORN, AHA. Joint statement: roadmap for resuming elective surgery after COVID-19 pandemic. https://www.asahq.org/about-asa/newsroom/news-releases/2020/04/joint-statement-on-elective-surgery-after-covid-19-pandemic. Published 2020. Accessed April 25, 2020.
- COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;(March). doi:10.1002/bjs.11646
- Prachand VN, Milner R, Angelos P, et al. Medically necessary, time-sensitive procedures: scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. J Am Coll Surg. 2020. doi:10.1016/j.jamcollsurg.2020.04.011
- Dexter F, Parra MC, Brown JR, et al. Perioperative COVID-19 defense. Anesth Analg. 2020;XXX(Xxx):1. doi:10.1213/ane.0000000000004829
- ASA, APSF. Joint statement on non-urgent care during the COVID-19 outbreak. https://www.asahq.org/about-asa/newsroom/news-releases/2020/03/asa-apsf-joint-statement-on-non-urgent-care-during-the-covid-19-outbreak. Published 2020. Accessed April 29, 2020.
- Centers for Disease Control and Prevention. Overview of influenza surveillance in the United States. CDC webpage. 2010:1-5. http://www.cdc.gov/flu/weekly/pdf/overview.pdf.
- Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Heal Surveill. 2020;6:e18810. doi:10.2196/18810


 Issue PDF
Issue PDF