To the Editor:
We wish to thank the authors and editors of the APSF for publishing the study, “Improving Post Anesthesia Care Unit Handoff by Implementing a Succinct Checklist,”1 in the 2015 summer issue of the APSF Newsletter. This article informs the anesthesiology community about the importance of effective communication throughout a patient’s perioperative journey.
At MD Anderson Cancer Center, we have implemented and continue to modify our own postoperative handoff protocol, which has been presented at the 2015 ASA Practice Management Conference and the IARS (International Anesthesia Research Society, 2015). We would like to share some of our experiences in order to complement the work performed by Potestio and colleagues and perhaps further guide other groups who are about to embark on similar projects.
In this study, the authors customized their checklist by selecting from items identified in the handoff literature as being important for postoperative handoffs and they organized the items into Patient, Procedure, and Medications for their handoff report.1 While succinct and organized, there are 2 disadvantages with this method. First, even with a short list, not all items will be relevant to every handoff and other items may be missed. Potestio et al. acknowledge this drawback by stating that “any standardization tool is often going to be too comprehensive or too efficient.”1 Second, providers giving the handoff reports are forced to follow the order of the checklist. While this may be beneficial for less experienced providers who are just learning how to perform handoffs (such as junior residents who made up the majority of study subjects in this study), following a rigid checklist may elicit resistance among more experienced clinicians because it interferes with the “flow” of their practiced, yet not necessarily complete,2 handoff reports.3
In order to address these 2 issues, our protocol first allows anesthesia providers to give a verbal report in the manner of their choice. In contrast to pre-flight aviation checklists and surgical “time out” checklists, where a number of mostly unrelated items are sequentially addressed, unstructured anesthesia handoff reports are often told as a “story.”3 For example, a “non-standardized” report might state: “Mrs. X has a history of PONV so I administered ondansetron prophylactically” while in many “standardized” checklists, PONV and anti-emetics would be mentioned in separate sections (e.g., Patient and Medications). This liberal approach also allows providers to have the freedom to focus on the important details pertinent to the individual clinical scenario.
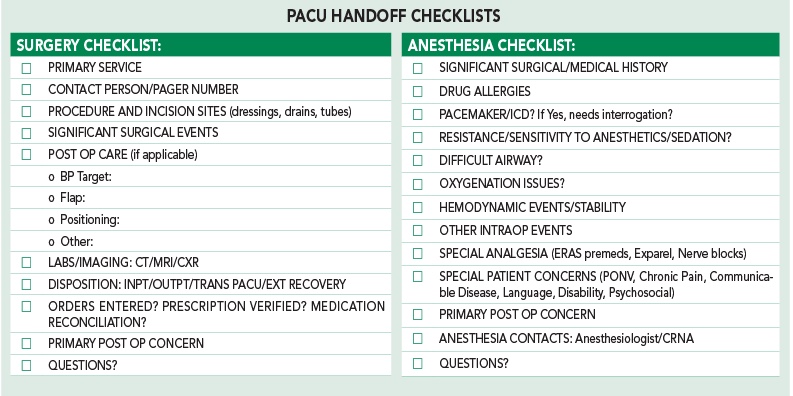
We do, however, still include a standardized checklist as part of our handoff protocol. After delivering their customized handoff report, anesthesia providers are asked to review a “Read and Verify” checklist (as opposed to the more common “Read and Follow” type checklists such as the one described in the authors’ study). This checklist contains 10 items that the handoff improvement team, which included anesthesiologists and PACU nurses, felt were critical to consider in every handoff exchange. It includes routine topics such as allergies and difficult airway, items required for CMS reimbursement such as hemodynamic stability,4 and less frequently encountered items such as communication barriers (language, hearing impairment) which can be overlooked as providers perform their “routine” handoff.
Click the image for a larger view.
To summarize, our handoff report can be adjusted to the simplicity/complexity of the patient/procedure because anesthesia providers are using their own judgment to decide how much detail is needed while key safety items are still reviewed as clinicians “skim” through the checklist. The resulting customized protocol was our attempt to strike a balance between individualization and standardization.
Two further points are worth noting. First, while checklists address the content of handoff protocols, it is also important to address process. For example, our protocol states that verbal handoff should occur only after the patient’s monitors have been attached, a baseline set of vital signs have been taken, and the patient is stable. This avoids multitasking5 and allows the PACU nurses to give providers their full attention when the time comes to take report. We also found that having the PACU RNs complete a worksheet based on the checklists helped them to focus on the transmitted information.
Second, we encourage the authors to follow up with their statement to implement handoff reports, including a checklist, from their surgery colleagues to guide in the patient’s immediate postoperative care. In our case, our initial assessment of existing handoffs and feedback from PACU RNs suggested that input regarding surgical issues such as incision sites, drains, patient disposition etc., were considered important to address as part of a complete postoperative handoff discussion. Therefore, a surgical checklist and verbal report by a surgical representative became part of our handoff protocol from inception. We found that surgical leadership support, presentation of local data regarding unsatisfactory handoffs, and examples of postoperative handoff research from their own surgical literature6 all helped to improve compliance. Perhaps these suggestions will be useful to Potestio and his colleagues as they move to build upon their current protocol.
Thank you again for sharing your work in this important area.
Drs. Jens Tan, Shreyas Bhavsar, Katherine Hagan, and Javier Lasala are Assistant Professors in the Department of Anesthesiology and Perioperative Medicine at the University of Texas MD Anderson Cancer Center in Houston, TX.
References
- Potestio C, Mottla J, Kelley E, et al. Improving post anesthesia care unit (PACU) handoff by implementing a succinct checklist. APSF Newsletter 2015; 30(1):13-15.
- Ilan R, LeBaron CD, Christianson MK, et al. Handover patterns: An observational study of critical care physicians. BMC Health Serv Res 2012;10:11
- Patterson ES. Structuring flexibility: The potential good, bad and ugly in standardization of handovers. Qual Saf Health Care 2008;17:4-5.
- Anesthesia Quality Institute. 2015 PQRS QCDR Measures by NQS Domain. Available at: http://www.aqihq.org/files/pqrs/2015_PQRS_QCDR_ MEASURES_BY_NQS_DOMAIN.pdf. Accessed August 11, 2015.
- van Rensen EL, Groen ES, Numan SC, et al. Multitasking during patient handover in the recovery room. Anesth Analg 2012;115:1183-7.
- <>Nagpal K, Abboudi M, Manchanda C, et al. Improving postoperative handover: a prospective observational study. Am J Surg 2013;4:494-501.


 Issue PDF
Issue PDF