The next patient safety movement is sustainable health care. Anesthetic gasses make an unexpectedly large contribution to health care pollution and emissions. This gives anesthesiologists the opportunity to lead in the effort to reduce health care’s impact on population health. If we can markedly reduce our specialty’s emissions, we can demonstrate to the entire health care sector that sustainable health care is possible and important to the well-being of our patients.
The harm done by health-care-related pollution is equivalent to the medical errors that sparked the patient safety movement.1 Anesthetic gas are one of the largest and most modifiable sources of health care sector greenhouse gas (GHG) emissions.2 Anesthesia professionals have the opportunity to lead the health care sector’s response to pollution and climate change.
Last summer, an older woman living in the usually mild climate of British Columbia suffered dyspnea following an extraordinary heatwave—her physician diagnosed her with “climate change.”3 While she is the first known to receive the diagnosis of climate change, she is not the first patient whose health has suffered because of climate change.4 She will not be the last.
Climate change is already affecting the health of our patients. Yet, the health care sector is just beginning to understand the impact of environmental health on population health, and to evaluate its large contribution to global emissions and climate-related morbidity.4-6
Impact of Anesthesiology on Our Environment
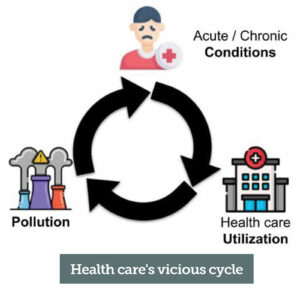
Figure 1: Health care’s vicious cycle. Pollution causes and exacerbates acute and chronic conditions, which require health care and health care contributes to pollution. Pollution is a patient safety issue.
The modern health care sector is responsible for an estimated 8.5% of United States GHG emissions; pollution that harms the very people the health care sector cares for (Figure 1).6,7 It is essential for the entire health care sector to evaluate and reduce its impact on the environment. Responding to climate change, and its downstream population health impact, is an opportunity for anesthesia professionals to lead on patient safety once again.
Pharmaceutical-related emissions account for approximately 20% of health care sector GHG emissions, more than food service, construction, or transportation.6 Volatile anesthetics and nitrous oxide can trap hundreds to thousands of times more energy than carbon dioxide.8 One study found anesthetic gasses could be the source of over 50% of the GHG footprint of the entire operating room (OR) suite.2
Desflurane9 and nitrous oxide10 have the highest impact on climate change due to their energy trapping ability and the concentration at which they are used clinically; sevoflurane is the least harmful, but still multiple times worse than the potent GHG methane. In a study comparing the GHG emissions per Minimum Alveolar Concentration (MAC)-hour of anesthesia, propofol is orders of magnitude less impactful on the climate than any volatile anesthetic.8
Adding to the harm of nitrous oxide, a recent study found intrahospital delivery of nitrous oxide to be dangerously inefficient with upwards of 70% of procured nitrous oxide being lost via leakage.11 The loss of nitrous oxide from hospital storage to OR utilization is a potential patient and occupational safety issue.
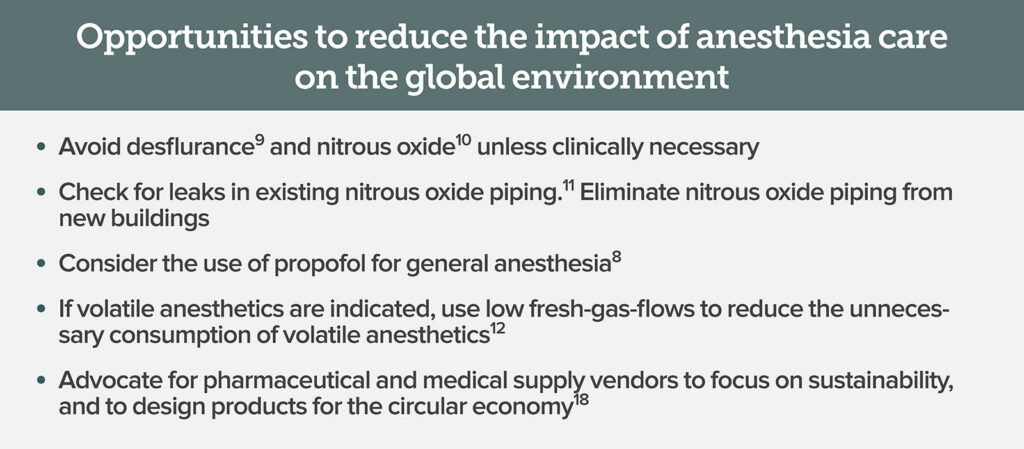
Making modifications to the delivery of anesthesia care (Figure 2) provides an opportunity to reduce our profession’s environmental impact and provide higher value patient care. For example, a multidisciplinary OR green team including anesthesia professionals at the University of Wisconsin Health educated the anesthesiology department on anesthetic gas waste, low-flow anesthesia,12 and differential GHG emissions of volatile anesthetics. Within three years they reduced their GHG emissions 64% per case while saving $25,000 per month.13 Furthermore, even if a health system institutes sustainable anesthesia practices like low fresh gas flows (<1L per minute), reusable instruments, and the elimination of desflurane and nitrous oxide, there is still an opportunity for the attentive, individual anesthesia professional to make a notable impact..14
How to get involved?
As global priorities shift and patients and organizations demand a more sustainable economy, health care will have to change. The current practice of medicine is unsustainable. In an unprecedented call to action, over 200 medical journals, including the New England Journal of Medicine, and The Lancet, published an editorial calling for emergency action to reduce greenhouse gas emissions and limit future harm.4,15
Climate change and environmental pollution are global, existential problems that require coordinated and collective action that can provoke anxiety and concern.16 There are many great organizations leading health care’s response to the climate crisis: Healthcare without Harm, Practice Green Health, and The Medical Society Consortium on Climate and Health. These three organizations lead the sustainable health movement in the United States. In addition, Medical Students for a Sustainable Future is a student-led organization for climate and health advocacy.
To be leaders in sustainable health care, anesthesia professionals must reduce the harm of their own practice and begin to advocate for more sustainable health systems. Health care institutions have both great responsibility and great ability. The health care sector is responsible for one-sixth of the entire US GDP; creating sustainable health care systems17 can catalyze change throughout the entire economy. Anesthesia professionals have the opportunity to reduce the environmental harm of our practice and again take a leading role in this next patient safety movement.
Jonathon P. McBride, MD, MS, is an incoming anesthesiology resident at the University of Michigan.
Matthew J. Meyer, MD, is an assistant professor of anesthesiology at the University of Virginia.
Matthew J. Meyer, MD, has consulted for Dialectica and received speaking fees from Takeda Pharmaceutical for a science forum on sustainability. Dr. Meyer has intellectual property related to perioperative efficiency and sustainability. Matthew J. Meyer, MD, is on the steering-committee of Virginia Clinicians for Climate Action. Jonathon P. McBride, MD, is a member of White Coats for Planetary Health and Medical Students for a Sustainable Future.
References
- Sherman JD, Lagasse R. How healthy is health care? JAMA Netw Open. 2018;1:e181000. 30646087. Accessed April 22, 2022.
- MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e381–e388. 29851650. Accessed April 22, 2022.
- Limb L. Frustrated doctor diagnoses woman with ‘climate change’ in world first. Euronews. Published November 10, 2021. https://www.euronews.com/green/2021/11/10/frustrated-doctor-diagnoses-woman-with-climate-change-in-world-first. Accessed February 2, 2022.
- Romanello M, McGushin A, Di Napoli C, et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. 2021;398:1619–1662. 34687662. Accessed April 22, 2022.
- Haines A, Ebi K. The imperative for climate action to protect health. N Engl J Med. 2019;380:263–273. 30650330. Accessed April 22, 2022.
- Eckelman MJ, Huang K, Lagasse R, et al. Health care pollution and public health damage in the United States: an update. Health Aff . 2020;39:2071–2079. 33284703. Accessed April 22, 2022.
- Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care system and effects on public health. PLoS One. 2016;11:e0157014. 27280706. Accessed April 22, 2022.
- Sherman J, Le C, Lamers V, Eckelman M. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg. 2012;114:1086–1090. 22492186. Accessed April 22, 2022.
- Meyer MJ. Desflurane should des-appear: global and financial rationale. Anesth Analg. 2020;131:1317–1322. 32925355. Accessed April 22, 2022.
- Muret J, Fernandes TD, Gerlach H, et al. Environmental impacts of nitrous oxide: no laughing matter! Comment on Br J Anaesth. 2019;122:587–604. Br J Anaesth. 2019;123:e481–e482. 31320116. Accessed April 22, 2022.
- Seglenieks R, Wong A, Pearson F, McGain F. Discrepancy between procurement and clinical use of nitrous oxide: waste not, want not. Br J Anaesth. 2022;128:e32–e34. 34802695. Accessed April 22, 2022.
- Anesthesia Patient Safety Foundation. Concern about the use of very low-flow sevoflurane anesthesia. Published February 1, 2018. https://www.apsf.org/article/concern-about-the-use-of-very-low-flow-sevoflurane-anesthesia/ Accessed February 23, 2022.
- Zuegge KL, Bunsen SK, Volz LM, et al. Provider education and vaporizer labeling lead to reduced anesthetic agent purchasing with cost savings and reduced greenhouse gas emissions. Anesth Analg. 2019;128:e97–e99. 31094796. Accessed April 22, 2022.
- McGain F, Sheridan N, Wickramarachchi K, et al. Carbon footprint of general, regional, and combined anesthesia for total knee replacements. Anesthesiology. 2021;135:976–991. 34529033. Accessed April 22, 2022.
- Atwoli L, Baqui AH, Benfield T, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. N Engl J Med. 2021;385:1134–1137. 34491006. Accessed April 22, 2022.
- Clayton S. Climate anxiety: Psychological responses to climate change. J Anxiety Disord. 2020;74:102263. 32623280. Accessed April 22, 2022.
- Health System Sustainability Centers: A remedy for climate catastrophe. https://www.healthaffairs.org/do/10.1377/forefront.20211029.282272/full/. Accessed February 1, 2022.
- MacNeill AJ, Hopf H, Khanuja A, et al. Transforming the medical device industry: road map to a circular economy. Health Aff (Millwood). 2020;39:2088–2097. https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.01118. Accessed April 22, 2022.


 Issue PDF
Issue PDF PDF
PDF