Dan Cole, MD, has recently been elected as APSF President and has been a major contributor on the APSF Board of Directors for years. He has a long history of strong dedication to perioperative patient safety and is a pioneer in the field of brain health. Dan is a neuroanesthesiologist and professor of Clinical Anesthesiology in the Department of Anesthesiology and Perioperative Medicine at the David Geffen School of Medicine, University of California, Los Angeles. His leadership skills are incomparable, and he has held past positions as President of the American Society of Anesthesiologists and American Board of Anesthesiology. Please welcome him as we continue our quest that “no one shall be harmed by anesthesia care.”
It is an honor to follow in the footsteps of legendary past APSF presidents such as Ellison Pierce, Robert Stoelting, and Mark Warner. It is a past that we can all be proud of; not only because of the scores of extraordinarily talented individuals who have been deeply committed to a vision “that no one shall be harmed by anesthesia care,” but also because APSF is an exceptional organization that has ensured that ideas became action, action that changed the world. Our organization has truly connected with our purpose and is one of the most amazing groups of people that I have been involved with.
Considering the complexity of health care systems, it should not be surprising that safety problems are endemic in health care. What is surprising is the sustained magnitude of the problem since the Institute of Medicine reported in 1999 (To Err Is Human: Building a Safer Health System) a headline that almost 100,000 deaths occur each year in hospitals due to medical error.1
To quote the World Health Organization, “The occurrence of adverse events due to unsafe care is likely one of the ten leading causes of death and disability in the world.”2 Patient safety is a “global health priority” and our work is far from done.
Safety is the foundation upon which the pillars by which we achieve quality care and the essential trust of our patients are built. These pillars include system competency, clinical competency of the provider(s), teamwork and communication, primacy of the patient’s interest, and the well-being of the workforce caring for patients.
In the above cited report, the Institute of Medicine stated that “anesthesia mortality rates are about one death per 200,000–300,000 anesthetics administered, compared with two deaths per 10,000 anesthetics in the early 1980s.”1 Although the exact figure of anesthesia-related mortality is controversial, there is no doubt that our specialty has made remarkable gains in safety over the past decades. Accordingly, as a specialty, we have not left the space that we worked so hard in during the 80s and 90s, but have expanded our vision of safety from reducing mortality with a focus on drug errors and hypoxia due to a difficult airway, to improving perioperative processes that enhance the long-term functional, cognitive, and psychological health of our patients.
We have a proud past, but an even more exciting future. Founding APSF President Ellison “Jeep” Pierce focused on the premise that safety is not a one and you’re done process. It is a long game that must be sustained by research, education, and by embedding science and best practices into the systems of care within which we work. It is analogous to running a marathon without a finish line. It is a one-step-at-a-time commitment to a shared struggle. It is about the end of a beginning stage of work and the beginning of a new stage of improvement. And finally, it is about the rewards from working at the frontier of quality and safety, knowing that you made the world a better place.
It seems as though more change has occurred in health care over the last few years than in the previous 30 years, and, like it or not, the next decade promises a tsunami of change. For example, multidisciplinary care pathways that incorporate precision medicine and are designed to improve patient outcomes by integrating preoperative risk assessment, prehabilitation, standardized intra- and postoperative management, and home rehabilitation will continue to grow and become commonplace. Home rehabilitation is likely to incorporate microsensors, remote monitoring, and the “hospital at home” model of care. Other technological advances include automated systems of anesthesia delivery, machine learning, artificial intelligence, and telehealth. We will have to learn about and carefully analyze these disruptive innovations to ensure that safety is not compromised and that safety standards are proactively embedded into new processes of patient care.
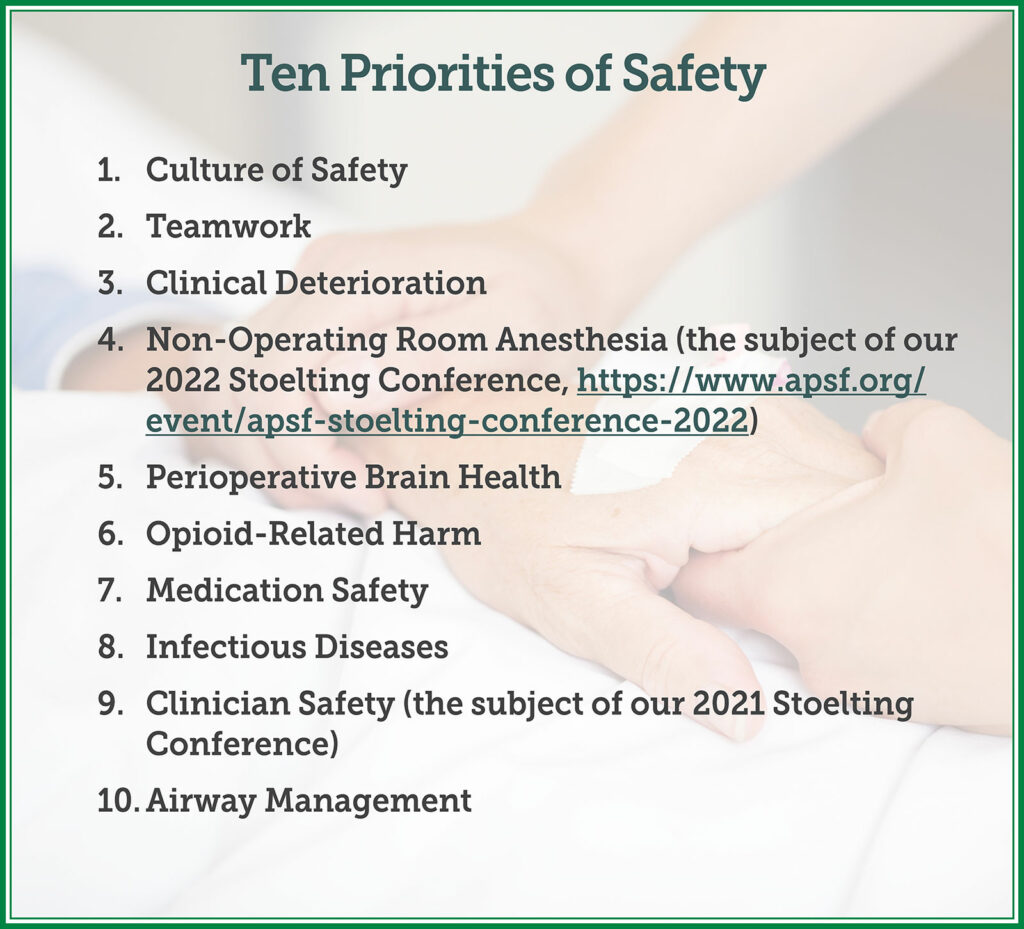
The APSF has at least six levers by which we turn ideas into action and action into results. They include research, education, the Newsletter, other communication vehicles (e.g., social media), collaboration with other stakeholders in patient safety, and advocacy. We will continue to pull these levers to make progress in the fight against preventable harm. Our focus this year will be directed at our ten priorities.
We have a deeply committed group of volunteers, who, I am confident, will rise to the safety challenges that will result from disruptive innovation that will occur in the perioperative space over the next decade. We rely on your financial support to achieve our goals, and we will use our resources wisely to ensure that anesthesiology continues to be a leader in patient safety. Sometimes it is best to resist change, sometimes to align with change, but we at the APSF will be proactive to continue our work to fulfill the vision “that no one shall be harmed by anesthesia care.” It is indeed a sacred trust that we have with our patients and our goal is to further the foundation of trust on which our specialty has been built.
Dan Cole, MD, is professor of clinical anesthesiology in the Department of Anesthesiology and Perioperative Medicine David Geffen School of Medicine, University of California at Los Angeles. He is also the current president of the Anesthesia Patient Safety Foundation.
The author has no conflicts of interest.
References:
- Kohn LT, Corrigan JM, Donaldson MS, Editors; Committee on Quality of Health Care in America, Institute of Medicine. 2000. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press. https://doi.org/10.17226/9728. Accessed December 6, 2021.
- World Health Organization. Patient Safety. https://www.who.int/news-room/fact-sheets/detail/patient-safety. Published 2019. Updated September 13, 2019. Accessed December 6, 2021.


 Issue PDF
Issue PDF PDF
PDF