Introduction
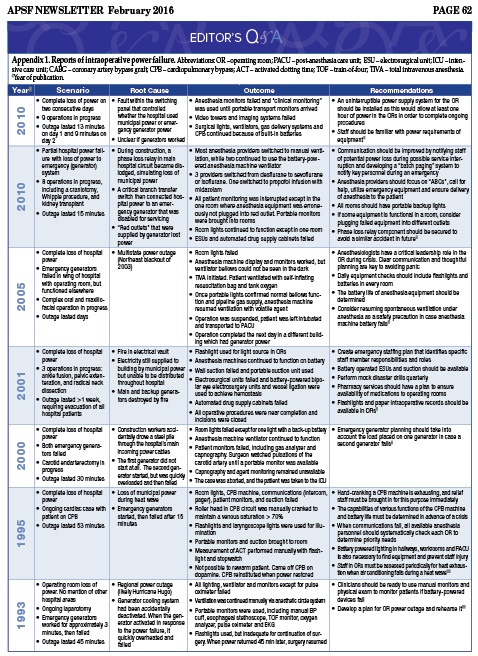
Loss of electrical power in a hospital is a patient safety hazard that has been neglected in medical training and research.1,2 The technology-rich environment of the operating room (OR) puts patients at risk should a sudden loss of power occur, as lights and critical equipment may fail without warning. Regional disasters and extreme weather events are the most common causes of power outages. Extreme weather events have become more common in the past two decades, and it is projected that regional power failures will occur more frequently and last longer in future years, despite efforts to improve power grid resiliency.3,4 Hospital power failure may also be the result of a local disruption of municipal power, or be limited to a single institution. Published case reports (Appendix 1) suggest that frequent root causes of intraoperative power loss are a failure of emergency generators to function during a widespread power outage, and hospital construction work that unmasks faults in internal electrical systems.5-11 These reports underscore the fact that hospital emergency generators and back-up systems are not completely reliable. Anesthesia providers need to know as much about responding to power failure as they do about managing any other intraoperative crisis. As there is no centralized reporting system for hospital power failure events, the true incidence of this emergency is unknown. Based on anecdotal experience, we believe it may be more common than is generally appreciated.
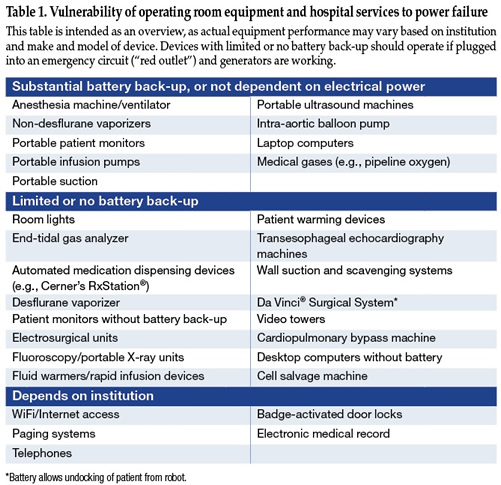
In addition to direct effects on critical anesthesia equipment, other repercussions of power outage in the OR can be extensive (Table 1). Power failure often translates to loss of lighting in the OR and adjacent hallways. Surgeons are faced with loss of electrosurgical units, video display monitors, and suction.6,8 Anesthesia machines and ventilators revert to battery power, which may last from 30 to 90 minutes depending on device and manufacturer specifications. Surprisingly, there are few reports on how well anesthesia machines function on battery power, and what can be expected when their batteries are finally depleted. Electronic patient monitors, desflurane vaporizers, and end-tidal gas analyzers often lack battery back-up. Hospital power failure may compromise communications (telephones, pagers, WiFi), electronic medical records, access to critical medications from automated dispensing cabinets, room temperature control, sterilization capabilities, elevators, and staff access to clinical areas through badge-secured doors.12,13 In some cases, operations may need to be aborted and patients evacuated. Prolonged hospital power failure eventually impacts sanitation, access to food and clean water, transportation and security.
Our anesthesia department at a tertiary-care medical center was recently faced with the challenge of preparing for electrical upgrades in a new hospital building that could temporarily compromise emergency generator power delivery to a suite of operating rooms and other critical areas. Published reports suggest that anesthesia departments should be knowledgeable about the battery life and capabilities of their equipment, should have sources of back-up lighting and monitoring immediately available, and should have a disaster plan that engages the entire OR staff. We thus embarked upon a project to review our current emergency plans, test the functionality of key anesthesia equipment during power failure, and develop a safety checklist and inexpensive emergency patient monitoring kit.
Anesthesia Equipment Testing
We tested two different anesthesia machines, one portable monitor and one infusion pump for duration of battery life and functionality on battery power (Table 2). Multiple examples of each device were tested, and all devices were charged overnight prior to testing. Anesthesia machine, ventilator, infusion pump, and portable monitor function were observed until display screens indicated “0% battery,” and then until devices failed and screens became dark.
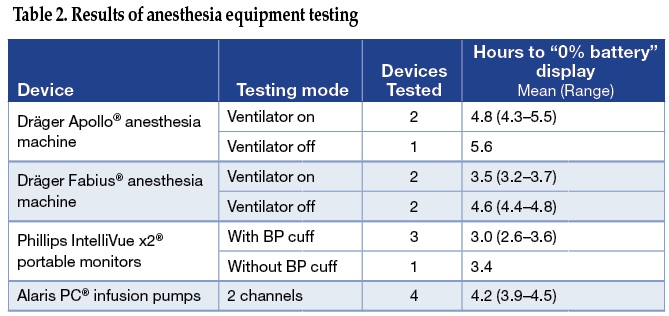
Anesthesia machines on battery power were tested both with ventilator on (set to tidal volume of 500 mL and respiratory rate 10 breaths per minute), or ventilator off (simulating a “manual ventilation” state). Fresh gas flow was set to 2 L/min, sevoflurane was dialed to 2%, and end-tidal sevoflurane was measured. Alaris pumps were set-up to run two channels, simulating a carrier infusion at 150 mL/hour and a phenylephrine infusion at 25 mcg/min. In addition to measuring infusion pump battery life, the function of infusion pumps was measured by comparing pump output in mL/hour for devices on battery power compared to alternating current (AC) power. Phillips monitors were tested for battery life both with a non-invasive blood pressure (NIBP) cuff cycling every 5 minutes, and with no NIBP cuff measurements.
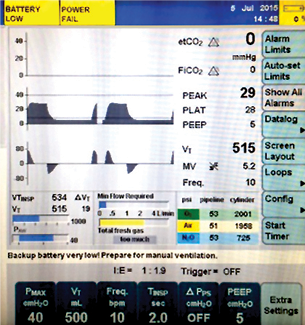
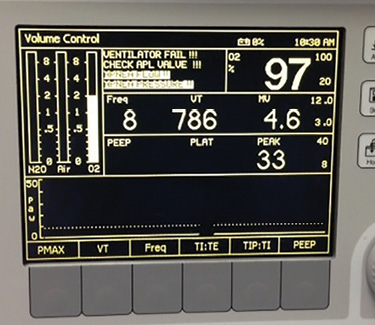 Figure 1. Screens displayed on Dräger Apollo and Fabius GS anesthesia machines at time of battery failure.
Figure 1. Screens displayed on Dräger Apollo and Fabius GS anesthesia machines at time of battery failure.
We found that all types of equipment had a battery life longer than expected, approximately 3 to 4 hours. Anesthesia machine battery life was extended by approximately 1 hour by turning the ventilator off and using manual ventilation. Ventilators on Fabius machines continued to operate for <10 minutes after “0% battery” was displayed, but Apollo ventilators continued functioning for several hours longer. Sevoflurane vaporizer output on both types of anesthesia machines was consistent with dialed settings as long as there was fresh gas flow, and did not depend whether the anesthesia machine was using alternating current (AC) power, battery power, or had a completely depleted battery. Fresh gas flow, rotometers, and the oxygen flush valve were unaffected by AC power loss or battery depletion. These observations are consistent with the manufacturer’s specifications, except that battery life was consistently longer than the 30–90 minutes advertised for these machines (Dräger anesthesia machine user manuals courtesy of Dräger Medical, Inc). Alaris pumps failed within minutes of “battery failure” warning screens. Their fluid volume output was no different whether on battery or AC power. Phillips monitors also failed within about 15 minutes of a “0% battery” indicator screen. In general, displays on all devices underestimated actual battery life. It is unsurprising that manufacturers err on the side of caution in displaying this value to the user, particularly for critical medical devices. All types of devices displayed increasingly loud, visible, and difficult-to-ignore warnings when close to battery failure (Figure 1). No device failed without warning during testing. It is important to note that complete battery depletion during tests such as these can adversely affect subsequent battery function, so repeated tests are not advised.
Emergency Monitoring Supplies
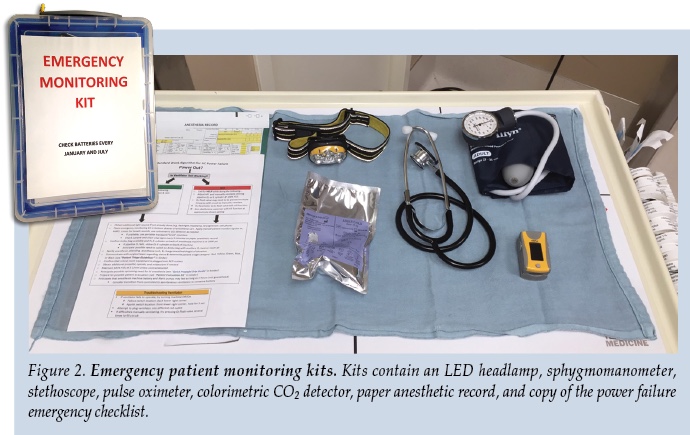
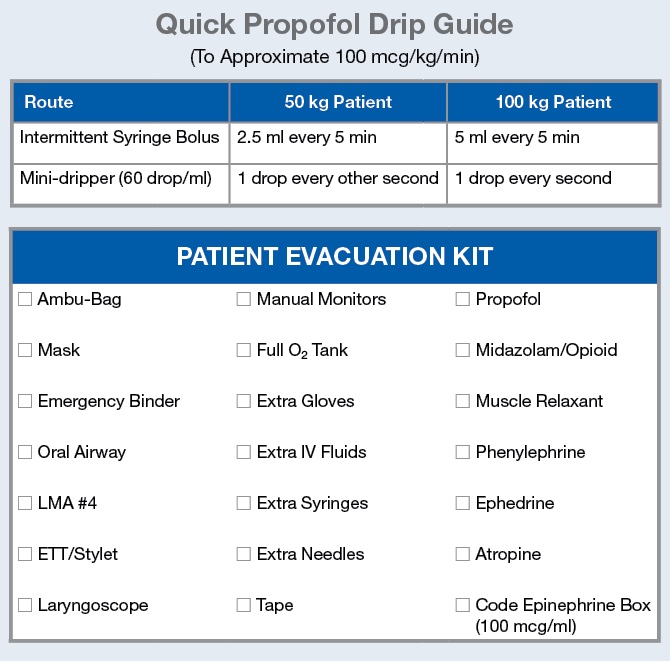
While it is helpful to know how anesthesia equipment will generally perform during a crisis, it is also wise to plan for contingencies. In order to be prepared for a worst-case scenario in which patient monitors fail and portable monitors are unavailable, we designed and distributed “Emergency Monitoring Kits” to carts in every anesthetizing location. Figure 2 shows the contents of the $60 kits, of which the most important are an inexpensive pulse oximeter and a light-emitting diode (LED) headlamp. The kits are sealed with break-away tags to discourage component theft, and batteries in headlamps, pulse oximeters, and LED flashlights kept in all anesthesia machines are replaced every 6 months. A paper anesthetic record is included not only for anesthesia charting, but as a critical part of patient identification and documentation during an evacuation.
OR Power Failure Checklist
Checklists are useful cognitive aids for clinicians that have been proven to increase patient safety in numerous areas of medicine.14,15 For anesthesiologists and nurse anesthetists, checklists are particularly helpful guides for patient management during rare, life-threatening intraoperative events such as malignant hyperthermia and local anesthetic systemic toxicity.16-18 In published reports, anesthesia providers have had variable responses to operating room power failure, including switching to manual ventilation and discontinuing volatile anesthetics.6,7 These actions may be appropriate in some power failure situations, and inappropriate in others.
As we were unable to find any published checklists on crisis management for OR power failure, we created our own (Figure 3). Based upon the results of equipment testing and multiple simulations, we decided that the crucial first step during power failure was to determine whether the anesthesia machine and ventilator were functional, and if so, to continue using them. This step allows the clinician’s hands to be free to perform other necessary tasks, allows continued delivery of a reliable anesthetic, and minimizes the chance of barotrauma and respiratory alkalosis from manual ventilation. Confidence that volatile anesthetic will continue to be delivered removes the immediate burden on the anesthesia provider to urgently convert to a total intravenous anesthetic (TIVA) in the dark. Furthermore, as electronically controlled medication dispensing stations are not operational without power, supply of intravenous sedatives and anesthetics may be rapidly depleted if multiple ORs are affected. Another crucial element of the checklist involves repeated steps to assure the delivery of oxygen to the patient. In the case of a disaster such as an earthquake, pipeline oxygen supply may be damaged or turned off as a fire control measure. We also include prompts for the anesthesia provider to confirm that critical equipment is plugged into a generator-powered circuit (“red outlets”), to communicate with the surgical team and nursing staff regarding prioritization of help for patient care, and to prepare for patient evacuation if necessary.
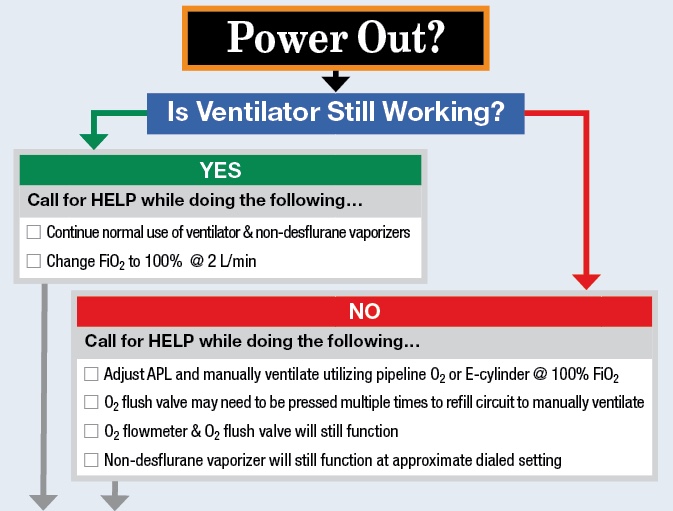
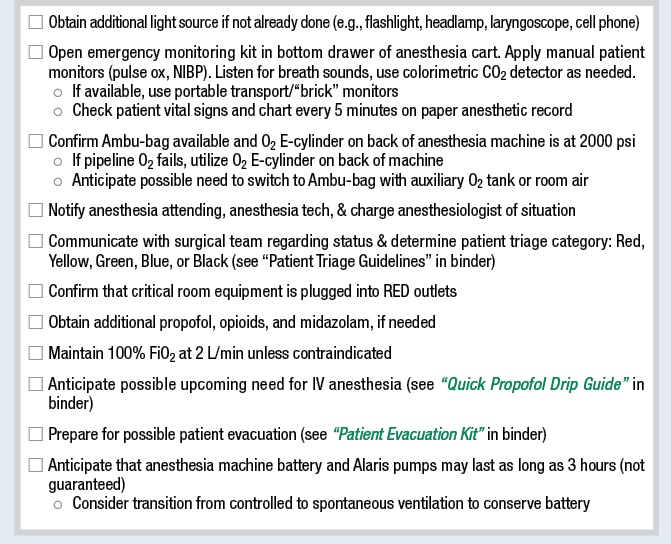
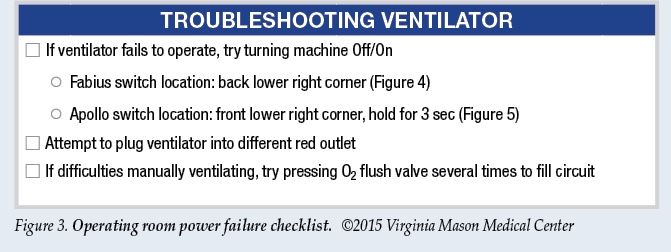
 Figure 4: Fabius On/Off Switch (back of machine). |
 Figure 5: Apollo On/Off Switch (hold for 3 sec). |
Discussion
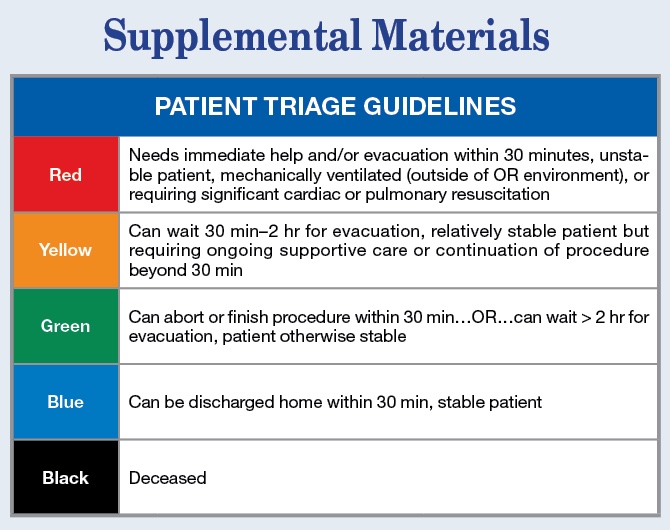
Operating room power failure is a critical event that merits advance preparation to prevent catastrophic patient harm. Hospitals are rightly subject to rigorous regulations regarding emergency generator power testing and reliability, and required to develop plans for power failure emergencies.19 In most cases, it is likely that in the event of intraoperative power loss, approximately 10 seconds (or longer) of darkness will be followed by restoration of power by generators. Return of electrical power does not mean the end of a crisis, however, as sophisticated medical equipment may be damaged by power surges or forced to undergo a prolonged restarting process. Recently at our institution, municipal power interruption of less than a second caused by an accident at a local electrical substation resulted in unanticipated problems: damage to delicate electronics in some fluoroscopy equipment, malfunction of a transesophageal echocardiography machine during a cardiac case, and loss of video imaging for several minutes during a da Vinci® robot-assisted laparoscopic case in which significant bleeding was occurring. A delay of care for several minutes as equipment reboots during a critical part of a procedure can be dangerous. Regardless of whether a crisis is brief or prolonged, or whether generators work or not, patients remain at significant risk whenever power is interrupted. Management of intraoperative power failure should be part of a coordinated medical facility response. While preparedness within the operating room is important, it is equally important to develop an institutional system for disaster response that allows for a clear chain of command with recognized roles and protocols, rapid assessment of patient needs, and deployment of resources. The Hospital Incident Command System (HICS)20 is the basis of our institution’s efforts to build a robust emergency preparedness program. Within the HICS system, protocols in perioperative areas are being developed that allow staff to rapidly assess operating room needs and triage care even in the presence of darkness and loss of normal avenues of communication. Individual operating room needs are triaged by color to direct assistance to the most critical, and gauge OR readiness to receive patients during an emergency.
This project has allowed us to explore our capabilities “in the dark” as an anesthesia service practicing in an earthquake hazard area, and has also allowed us to engage the entire medical center in preparations and simulations for disaster planning. Anesthesiologists, nurse anesthetists, and anesthesia technicians should learn about the battery capabilities of their equipment and the projected impact of a power outage on key services necessary for patient care. Anesthesia departments should have extra equipment for patient monitoring readily available, most importantly, LED headlamps and battery-powered pulse oximeters. A checklist may help clinicians remember to perform key steps when the lights go out: finding alternative light sources, preventing hypoxemia, and confirming that critical equipment is plugged into generator-powered outlets. We continue to refine and practice this checklist and our disaster response protocols, and hope that others may use our experience as a starting point for discussing preparedness for power failure and other emergencies at their own institutions.
Authors: Erica L. Holland, MD Carli D. Hoaglan, MD Martha A. Carlstead, CRNA Ryan P. Beecher, CRNA Grete H. Porteous, MD* Department of Anesthesia, B2-AN Virginia Mason Medical Center Seattle, WA *Corresponding authorDisclosures and conflicts of interest: None
Acknowledgments:
We are grateful for the assistance and support of Randy Johnson, Cert. A.T., without whom this project would not have been possible.
References
- Eichhorn JH, Hessel EA. Electrical power failure in the operating room: a neglected topic in anesthesia safety. Anesth Analg 2010;110:1519–21.
- Klinger C, Landeg O, Murray V. Power outages, extreme events and health: a systematic review of the literature from 2011–2012. PLoS Curr 2014 Jan 2; 6:ecurrents.dis.04eb1dc5e73dd1377e05a10e9edde673
- Larsen PH, LaCommare KH, Eto JH, Sweeney JL. Assessing changes in the reliability of the U.S. electric power system. Lawrence Berkeley National Laboratory 2015. Available at: https://publications.lbl.gov/islandora/object/ir%3A188741. Accessed October 20, 2015.
- DOE-PI (U.S. Department of Energy’s Office of Policy and International Affairs): U.S. Energy sector vulnerabilities to climate change and extreme weather. 2013. Available at: http://energy.gov/sites/prod/files/2013/07/f2/20130710-Energy-Sector-Vulnerabilities-Report.pdf. Accessed October 20, 2015.
- Riley RH. Power failure to a tertiary hospital’s operating suite. Anaesth Intensive Care 2010; 58:785.
- Carpenter T, Robinson ST. Response to a partial power failure in the operating room. Anesth Analg 2010; 110:1644–6.
- Yasny J, Soffer R. A case of a power failure in the operating room. Anesth Prog 2005; 52:65–69.
- Pagán A, Curty R, Rodriquez MI, Pryor F. Emergency—Total power outage in the OR. AORN J 2001; 74:514–516.
- Tye JC, Chamley D. Complete power failure. Anaesthesia 2000; 55:1133–1134.
- Troianos, CA. Complete electrical failure during cardiopulmonary bypass. Anesthesiology 1995; 82:298–302.
- Norcross DE, Elliott BM, Adams DB, Crawford FA. Impact of a major hurricane on surgical service in a university hospital. Am Surg 1993; 59:28–33.
- Nates JL. Combined external and internal hospital disaster: Impact and response in a Houston trauma center intensive care unit. Crit Care Med 2004; 32:686–690.
- O’Hara JF, Higgins TL. Total electrical power failure in a cardiothoracic intensive care unit. Crit Care Med 1992; 20:840–845.
- Treadwell JR, Lucas S, Tsou AY. Surgical checklists: a systematic review of impacts and implementation. BMJ Qual Saf 2014; 4:299–318.
- Byrnes MC, Schuerer DJE, Schallom ME, et al. Implementation of a mandatory checklist of protocols and objectives improves compliance with a wide range of evidence-based intensive care unit practices. Crit Care Med 2009; 10: 2775–81.
- Ziewacz JE, Arriage AF, Bader AM, et al. Crisis checklists for the operating room: development and pilot testing. J Am Coll Surg 2011; 213:212–19.
- Neal JM, Mulroy MF, Weinberg GL. American Society of Regional Anesthesia and Pain Medicine checklist for managing local anesthetic systemic toxicity: 2012 version. Reg Anesth Pain Med 2012; 37(1):16–8.
- Harrison TK, Manser T, Howard SK, Gaba DM. Use of cognitive aids in a simulated anesthetic crisis. Anesth Analg 2006; 103(3):551–6.
- JCAHO (Joint Commission on Accreditation of Healthcare Organizations): Preventing adverse events caused by emergency electrical power system failures. The Joint Commission Sentinel Event Alert 2006; 37: 1-3. Available at:
http://www.jointcommission.org/sentinel_event_alert_issue_37_preventing_adverse_ events_caused_by_emergency_electrical_power_system_failures/. Accessed October 20, 2015. - Arnold JL, Dembry LM, Tsai MC, et al. Recommended modifications and applications of the Hospital Emergency Incident Command System for hospital emergency management. Prehosp Disast Med 2005; 20(5):290–300.
The APSF sometimes receives questions that are not suitable for the Dear SIRS column. This Q and A column allows the APSF to forward these questions to knowledgeable committee members or designated consultants. The information provided is for safety-related educational purposes only, and does not constitute medical or legal advice. Individual or group responses are only commentary, provided for purposes of education or discussion, and are neither statements of advice nor the opinions of the APSF. It is not the intention of the APSF to provide specific medical or legal advice or to endorse any specific views or recommendations in response to the inquiries posted. In no event shall the APSF be responsible or liable, directly or indirectly, for any damage or loss caused or alleged to be caused by or in connection with the reliance on any such information.


 Issue PDF
Issue PDF