The transition of responsibility and accountability for patient care from one clinical team to another is a routine part of modern health care delivery. Whether between physical locations (e.g., from the emergency department to an inpatient floor), or between teams in a static location (e.g., from a day team of trainees to a night float team), effective handoffs are crucial to safe, high-quality care.1 With over 300 million surgical procedures performed worldwide, a number that is poised only to increase as the population ages and low and middle income countries gain access to surgical care,2,3 perioperative handoffs between anesthesia clinicians, postanesthesia care unit (PACU) nurses, and intensive care unit (ICU) teams will only increase in frequency.
Yet, despite the fact that handoffs occur so frequently, they continue to be a critical point in patient care that can result in patient harm. The Joint Commission reports that its sentinel event database contains reports of wrong-site surgery, delays in treatment, falls, and medication errors as a result of inadequate communication at handoff,4 and has maintained handoffs as an area of patient safety concern since they were first included in their National Patient Safety Goals in 2006.5 Perioperative handoffs are especially risky, often occurring in noisy, complex care environments. While the published literature is evolving, there have been numerous studies supporting the association of intraoperative handoffs with increased morbidity and mortality.6-10
Aware of the challenges related to perioperative handoffs, and each leading improvement efforts in their own institutions, a small group of academic anesthesiologists from around the United States assembled at the annual meeting of the American Society of Anesthesiologists (ASA) in 2015 to brainstorm how we could learn from one another. As we shared ideas about how to expand interest in the topic of handoffs as a perioperative patient safety issue, our group collaborated with the APSF to plan and conduct the first Stoelting Consensus Conference on Perioperative Handoffs in 2017. The interprofessional conference of patient safety experts led to over 50 consensus recommendations across a number of domains, including process elements, behaviors, metrics and measurement, education and training, implementation, and research.11
The Stoelting Conference recommendations created the foundation for what is now the Perioperative Multi-center Handoff Collaborative (MHC) under the leadership of Philip Greilich, MD, MSc, as its founding chair. With a steering committee and initial working groups on communication, education, implementation, and research, the group began to expand its work. In 2019 the MHC’s collaborative relationship with APSF was formalized as it became a sponsored special interest group focused on perioperative transitions of care, enabling the group to access resources that have helped energize and sustain the work of the MHC.
Since its formation, the members and working groups of the MHC have worked tirelessly to improve handoffs through multiple channels. Members of the MHC have participated as lecturers and panelists on the topic of handoffs at national meetings of the ASA, International Anesthesia Research Society, Society of Cardiovascular Anesthesiologists, and International Symposium of Human Factors Ergonomics in Healthcare and the World Federation of Societies of Anesthesiology. The communications workgroup successfully created and launched a website (www.Handoffs.org), with literature, resources and tools related to perioperative handoff improvement. The education and training group has created and curated a collection of handoff education and training tools, including a comprehensive list of mnemonics and checklists for all types of perioperative handoffs. The implementation/electronic medical record (EMR) workgroup successfully partnered with Epic Systems (Madison, WI.) to create a standardized intraoperative handoff tool that is now included in the standard Epic build for hospitals and health systems across the United States.12 Members of the research workgroup have worked independently and together to expand the evidence base for optimal handoffs, publishing multiple manuscripts in journals related to anesthesiology, quality and safety, human factors, and implementation science.10-26
Alongside and in addition to these accomplishments, the MHC has continued its push to further the conversation about perioperative handoffs. In 2019, the MHC held a workshop during the ASA Annual Meeting where we confirmed interest in setting a formal research agenda and began characterizing the questions that would benefit from a research conference to generate solutions. A proposal entitled “Handoff Effectiveness Research in periOperative environments (HERO) Collaborative Research Conference” was initially submitted in January 2020, funded by the Agency for Healthcare Research and Quality (AHRQ) in March 2021, and ultimately conducted in February 2022 after a number of COVID-related delays. The objective of this research development conference was to operationalize the existing literature base, create a research agenda, foster full stakeholder engagement, and build the research infrastructure necessary to address critical evidence gaps. The conference was designed to leverage MHC’s accomplishments and growth, harness the synergy of stronger relationships with diverse stakeholders required to advance and accelerate handoff research, and promote widespread adoption of this patient safety priority.
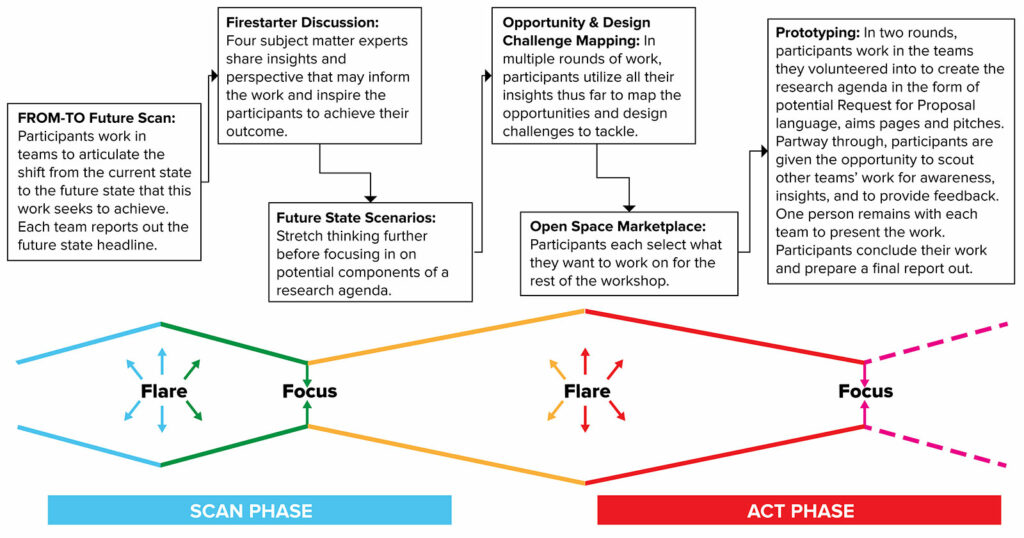
The HERO collaborative research conference was a two-day virtual design studio workshop cochaired by Philip Greilich, MD, MSc, and Dan France, PhD, and designed by members of the MHC.17 The design workshop was facilitated by the Vanderbilt University Medical Center’s Strategy and Innovation office, taking advantage of their expertise in the design studio methodology and the mentorship of its senior advisor, Matt Weinger, MD, MSc. Design Studio is a Lean User Experience (UX) method that combines divergent and convergent thinking.27 It allows a group of people to address a well-defined problem, generate many ideas, and then converge into shared solutions in a short amount of time (Figure 1).
The research conference was designed to 1) organize and engage key stakeholders through inclusion of interdisciplinary experts on the planning committee and outreach to interested researchers and stakeholders across the country; 2) facilitate maximal attendance by interprofessional teams from participating sites, representatives from relevant national organizations, and subject matter experts; 3) utilize a facilitated, creativity-enhancing, design studio process to energetically engage participants and complete clear and actionable deliverables at the conclusion of the conference, and 4) identify and prioritize the most promising scalable solutions.
We were intentional in inviting a diverse group of stakeholders and personas to achieve organizational alignment and identify user-friendly, technically feasible solutions that would create value. These solutions were intended to allow us to integrate research gaps and applicable interventions across different perioperative environments and health systems. Special attention was given to leveraging current health care technologies (e.g., cognitive aids, integrated data aggregation/analytics) to prompt and assess handoff interventions in real-time.
One hundred and ten individuals representing 43 organizations from academia, industry, professional societies, regulatory agencies, patient safety organizations, and funding agencies attended the two-day HERO design workshop. This design workshop brought together the key stakeholders in this domain, including clinicians, hospital leaders, researchers, quality improvement specialists, human factors and implementation scientists, and representatives from medical and nursing societies, industries, patient safety organizations, regulatory bodies, and funding entities, to build partnerships and to create an agenda to close the gap in perioperative handoff safety. Primary work products from the workshop included a paper on perioperative handoffs in the areas of intervention, design, measurement, and dissemination and implementation delivered to attendees prior to the studio event; the identification and prioritization of 18 product prototypes to advance perioperative handoff safety (Table 1); and publication of a Special Issue on Perioperative Handoff Quality and Safety in The Joint Commission Journal on Quality and Patient Safety.18
Table 1. Topics identified through the HERO conference for further exploration and development.*
| National Recognition & Integration |
| Universal guidelines for handoff communication and care coordination |
| National requirements by federal agencies for core handoff processes and assessment |
| Research network to identify key handoff issues and foster collaborative initiatives |
| Harmonization of measurement system for key effectiveness-implementation outcomes |
| Teamwork and Safety Culture |
| Handoff toolkits supported by institutional guidance teams |
| Teamwork competencies required for resilient interprofessional handoffs |
| Combined top-down and bottom-up user-centered change culture |
| Process Identification & Improvement |
| Workflow redesign to optimize handoff ergonomics |
| Engineering sociotechnical systems that reduce distractions and promote resilience |
| Platforms for accelerating organizational and/or institutional learning |
| Integration of patient/caregiver needs into the handoff continuum |
| Tools, Technology & Cognitive Aids |
| Augmented assistant to prompt and improve information transfer |
| Interactive/adaptive cognitive aids to anticipate risks and promote anticipatory guidance |
| Education & Training |
| Competency-based handoff education curriculum and assessment |
| Longitudinal, interprofessional teamwork education and training strategy |
| *Sparling JL, France D, Abraham J, et al. Handoff Effectiveness Research in periOperative environments (HERO) Design Studio: A Conference Report. Jt Comm J Qual Patient Saf. Published online February 2023.doi:10.1016/j.jcjq.2023.02.004. |
The growth and evolution of the MHC as a network hub for perioperative handoffs was positively impacted by the studio event by introducing 50 non-anesthesiologists to the MHC with half expressing an interest in becoming members. The transition of the HERO Planning Committee and the workshop solutions are driving transformational changes in the MHC to support the most promising individuals and ideas arise from this event. The workshop has already set into motion myriad activities to advance handoff research, develop academia-industry partnerships, and to train and develop future leaders in perioperative safety.
As we look forward to what is next for the MHC, we have begun strategic planning for “MHC 2.0” under the leadership of Aalok Agarwala, MD, MBA, as the new chair of the MHC. We have reorganized our workgroups to address the areas identified as most impactful in improving perioperative handoffs after taking into account the results of the HERO conference. Our communication workgroup will be focusing on increasing the visibility of the MHC and the work of its members through our website, social and traditional media, and collaborative relationships with partner organizations. Our education and training workgroup has begun work on creation of a comprehensive repository of the perioperative handoff literature and will be working to curate a repository for handoff education and training materials. Our EMR workgroup will continue its work with Epic (Madison, WI.) to expand OR-to-PACU handoff tools to mobile platforms and to create easy-to-use tools for OR-to-ICU handoff. And our newly formed implementation workgroup is in early stages of planning for a comprehensive implementation toolkit, designed to help individual champions improve perioperative handoffs in their own care environments. With dedicated individuals committed to continuous improvement, we are excited about the work that lies ahead.
If you or someone you know is interested in working to improve perioperative teamwork, communication, and patient safety, we invite you to join us in our efforts to make handoffs safer. We would love to have your help!
Philip E. Greilich, MD, MSc, is a professor of Anesthesiology & Pain Management, Health System Quality Officer and Director, Team FIRST at the University of Texas Southwestern Medical Center, Dallas, TX.
Aalok V. Agarwala, MD, MBA is chief medical officer at Massachusetts Eye and Ear and assistant professor of anesthesiology at Harvard Medical School, Boston, MA.
The authors have no conflicts of interest.
REFERENCES
- Gandhi TK. Fumbled handoffs: one dropped ball after another. Ann Intern Med. 2005;142:352–358. PMID: 15738454
- Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Int J Obstet Anesth. 2016;25:75–78. PMID: 26597405
- Mock CN, Donkor P, Gawande A, et al. Essential surgery: key messages from Disease Control Priorities, 3rd edition. Lancet. 2015;385:2209–2219. PMID: 25662414
- The Joint Commission. Inadequate hand-off communication. Sentinel Event Alert. 2017;58. PMID: 28914519
- Catalano K. JCAHO’S National Patient Safety Goals 2006. JPerianesth Nurs. Published online 2006. PMID: 16446238
- Boet S, Djokhdem H, Leir SA, et al. Association of intraoperative anaesthesia handovers with patient morbidity and mortality: a systematic review and meta-analysis. Br J Anaesth. 2020;125:605–613. PMID: 32682560
- Saager L, Hesler BD, You J, et al. Intraoperative transitions of anesthesia care and postoperative adverse outcomes. Anesthesiology. 2014;121:695–706. PMID: 25102312
- Hudson CCC, McDonald B, Hudson JKC, et al. Impact of anesthetic handover on mortality and morbidity in cardiac surgery: a cohort study. J Cardiothorac Vasc Anesth. 2015;29:11–16. PMID: 25440620
- Jones PM, Cherry RA, Allen BN, et al. Association between handover of anesthesia care and adverse postoperative outcomes among patients undergoing major surgery. JAMA. 2018;319:143. PMID: 29318277
- Abraham J, Pfeifer E, Doering M, et al. Systematic review of intraoperative anesthesia handoffs and handoff tools. Anesth Analg. 2021;132:1563–1575. PMID: 34032660
- Agarwala A V, Lane-Fall MB, Greilich PE, et al. Consensus recommendations for the conduct, training, implementation, and research of perioperative handoffs. Anesth Analg. 2019;128:e71–e78. PMID: 30995210
- Hong Mershon B, Vannucci A, Bryson T, et al. A collaborative partnership between the multicenter handoff collaborative and an electronic health record vendor. Appl Clin Inform. 2021;12:647–654. PMID: 34320682
- Lane-Fall MB, Christakos A, Russell GC, et al. Handoffs and transitions in critical care-understanding scalability: study protocol for a multicenter stepped wedge type 2 hybrid effectiveness-implementation trial. Implement Sci. 2021;16:63. PMID: 34130725
- Lazzara EH, Simonson RJ, Gisick LM, et al. Does standardisation improve post-operative anaesthesia handoffs? Meta-analyses on provider, patient, organisational, and handoff outcomes. Ergonomics. 2022;65:1138–1153. PMID: 35438045
- Michael MM, Ambardekar AP, Pukenas E, et al. Enablers and barriers to multicenter perioperative handoff collaboration: lessons learned from a successful model outside the operating room. Anesth Analg. 2021;133:1358–1363. PMID: 34673728
- Abraham J, Meng A, Tripathy S, et al. Systematic review and meta-analysis of interventions for operating room to intensive care unit handoffs. BMJ Qual Saf. 2021;30:513–524. PMID: 33563791
- Sparling JL, France D, Abraham J, et al. Handoff Effectiveness Research in periOperative environments (HERO) Design Studio: A Conference Report. Jt Comm J Qual Patient Saf. Published online February 2023. https://doi.org/10.1016/j.jcjq.2023.02.004
- Abraham J, Rosen M, Greilich PE. Call for papers: special issue on perioperative handoff safety and quality. Jt Comm J Qual Patient Saf. 2022;48:362–363. PMID: 35534421
- Massa S, Wu J, Wang C, et al. Interprofessional training and communication practices among clinicians in the postoperative icu handoff. Jt Comm J Qual Patient Saf. 2021;47:242–249. PMID: 33451897
- Daly Guris RJ, Lane-Fall MB. Checklists and cognitive aids: underutilized and under-researched tools to promote patient safety and optimize clinician performance. Curr Opin Anaesthesiol. 2022;35:723–727. PMID: 36302211
- Riesenberg LA, Davis R, Heng A, et al. Anesthesiology patient handoff education interventions: a systematic review. Jt Comm J Qual Patient Saf. Published online December 15, 2022. PMID: 36631352
- Lane-Fall MB, Christakos A, Russell GC, et al. Handoffs and transitions in critical care-understanding scalability: study protocol for a multicenter stepped wedge type 2 hybrid effectiveness-implementation trial. Implement Sci. 2021;16:63. PMID: 34130725
- Lazzara EH, Keebler JR, Simonson RJ, et al. Navigating the challenges of performing anesthesia handoffs and conducting anesthesia handoff research. Int Anesthesiol Clin. 2020;58:32–37. PMID: 31800413
- Lane-Fall MB, Pascual JL, Peifer HG, et al. A partially structured postoperative handoff protocol improves communication in 2 mixed surgical intensive care units: findings from the handoffs and transitions in critical care (HATRICC) prospective cohort study. Ann Surg. 2020;271:484–493. PMID: 30499797
- Abraham J, Duffy C, Kandasamy M, et al. An evidence synthesis on perioperative Handoffs: a call for balanced sociotechnical solutions. Int J Med Inform. 2023;174:105038. PMID: 36948060
- Webster KLW, Keebler JR, Chaparro A, et al. Handoffs and teamwork: a framework for care transition communication. Jt Comm J Qual Patient Saf. 2022;48:343–353. PMID: 35715018
- Tej R (Tejj). Design Studio: an intersection of ideas. https://uxdesign.cc/design-studio-an-intersection-of-ideas-23724b9ae141. Accessed February 21, 2023.


 Issue PDF
Issue PDF PDF
PDF