To the Editor
Lambert1 made a recent call for further examination of the transient radicular irritation syndrome (TRIS) that may occur after spinal anesthesia. This certainly deserves investigation. Although Schneider2 pointed out the incidence and possible seriousness of this apparent complication in 1993, one may think that its appearance may have been precipitated by a change in the local anesthetic composition or the technique of injection. However, Vandam and Dripps3 described this precise syndrome in one of their classic series of 3 publications on neurological complications noted in 10,098 patients receiving spinal anesthesia. Moreover, Pizzolato4 in 1959 and Gentili et al.5 in 1980, using different laboratory techniques, showed that all local anesthetics at high concentrations produce neurotoxicity.
It is not surprising that diagnostic electrophysiological studies do not reveal abnormalities in these cases, as they usually are only contributory after 15 or more days after nerve root injury.6 However, experienced radiologists can recognize the early stages of radicular inflammation when MRI images of nerve roots are enhanced with intravenous gadolinium, as shown in Figure 1.7-10 These findings can be seen in CAT scans, only when preceded by myelography, which is hardly justifiable under such circumstances, since it can exacerbate radicular injury.11
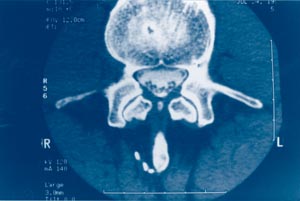
Figure 1: Axial view of MR image showing “enhanced” nerve roots whichare edematous and have a star-like appearance.
I echo Lambert’s suggestion for further investigation on TRIS and other neurological complications that may follow neuroaxial anesthesia; this is a challenge for all of us, and specifically the APSF.
The evidence against lidocaine in concentrations equal to or greater than 2% continues to mount.12,13 A lower incidence has been reported with prilocaine,13 mepivacaine and bupivacaine,14 and tetracaine,15 thus confirming the axiom proposed by Pizzolato: “All local anesthetics are potentially neurotoxic.”4 Since even a plain spinal tap results in inflammatory changes in the CSF, the $60,000 question raised by Gaiser,16 “Should intrathecal lidocaine be used in the 21st century?” can be expanded to the next logical question, one that we do not want to hear, “Should spinal anesthesia be used at all?”
J. Antonio Aldrete, MD, MS
Birmingham, AL
References
- Lambert DH. Transient radicular irritation remains a danger. APSF Newsletter 2003;18:38.
- Schneider M, Ettlin T, Kaufmann M, Schumacher P, Urwyler A, Hampl K, von Hochstetter A. Transient neurologic toxicity after hyperbaric subarachnoid anesthesia with 5% lidocaine. Anesth Analg 1993;76:1154-7.
- Vandam LD, Dripps RD. Long-term follow-up of patients who received 10,098 spinal anesthetics: incidence and analysis of minor sensory neurological defects. Surgery 1955;38:463-9.
- Pizzolato P, Renegar OJ. Histopathological effects of long exposure to local anesthetics on the spinal cord and on peripheral nerves. Anesth Analg 1959;38:138-41.
- Gentili F, Hudson AR, Hunter D, Kline DG. Nerve injection injury with local anesthetic agents: a light and electron microscopic, fluorescent microscopic, and horseradish peroxidase study. Neurosurgery 1980;6:263-72.
- Katims JJ. Electrodiagnostic functional sensory evaluation with pain: a review of the neuroselective current perception threshold. Pain Digest 1998;8:2129-30.
- Johnson CE, Sze G. Benign lumbar arachnoiditis: MR imaging with gadopentetate dimeglumine. AJR Am J Roentgenol 1990;155:873-80.
- Aldrete JA, Brown TL. Laboratory and clinical diagnosis. In: Aldrete JA, ed. Arachnoiditis: the silent epidemic. Denver: Futuremed 2000: 221-48.
- Avidan A, Gomori M, Davidson E. Nerve root inflammation demonstrated by magnetic resonance imaging in a patient with transient neurologic symptoms after intrathecal injection of lidocaine. Anesthesiology 2002;97:257-8.
- Aldrete JA. Nerve root “irritation” or inflammation diagnosed by magnetic resonance imaging. Anesthesiology 2003;98:1294
- Hoffman GS, Ellsworth CA, Wells EE, Franck WA, Mackie RW. Spinal arachnoiditis. What is the clinical spectrum? II. Arachnoiditis induced by Pantopaque/autologous blood in dogs, a possible model for human disease. Spine 1983;8:541-51.
- Kirihara Y, Saito Y, Sakura S, Hashimoto K, Kishimoto T, Yasui Y. Comparative neurotoxicity of intrathecal and epidural lidocaine in rats. Anesthesiology 2003;99:961-8.
- de Weert K, Traksel M, Gielen M, Slappendel R, Weber E, Dirksen R. The incidence of transient neurological symptoms after spinal anaesthesia with lidocaine compared to prilocaine. Anaesthesia 2000;55:1020-4.
- Salmela L, Aromaa U. Transient radicular irritation after spinal anesthesia induced with hyperbaric solutions of cerebrospinal fluid-diluted lidocaine 50 mg/ml or mepivacaine 40 mg/ml or bupivacaine 5 mg/ml. Acta Anaesthesiol Scand 1998;42:765-9.
- Sumi M, Sakura S, Kosaka Y. Intrathecal hyperbaric 0.5% tetracaine as a possible cause of transient neurologic toxicity. Anesth Analg 1996;82:1076-7
- Gaiser RR. Should intrathecal lidocaine be used in the 21st century? J Clin Anesth 2000;12:476-81.


 Issue PDF
Issue PDF