To the Editor:
Post-dural puncture headache (PDPH) was first described in 1898, a few hours after the first successful spinal anesthetic by August Bier. Over 100 years later, it is still a problem and little consensus exists on managing it.1 The risk of puncturing the dura inadvertently is between 0.2 and 4%.2-3
Data obtained from the American Society of Anesthesiologists closed claims analysis project show that this is the third most common reason for litigation in obstetric anesthesia in the USA.4
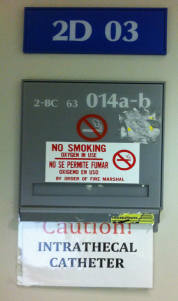
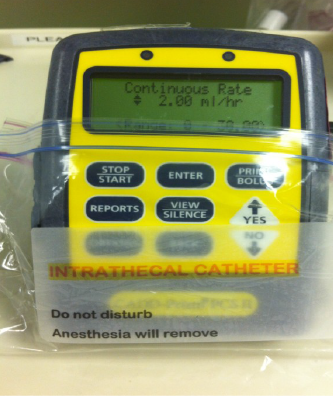
Intrathecal placement of an epidural catheter after unintended dural puncture has become increasingly common. Reasons cited for intrathecal catheter insertion are to prevent another unintended dural puncture, ensure excellent analgesia for normal labor, instrumental, or operative delivery, and to reduce the incidence and severity of postdural puncture headache.
There are safety concerns with the use of intrathecal catheters including the potential for high block, meningitis, and inappropriate drug administration.
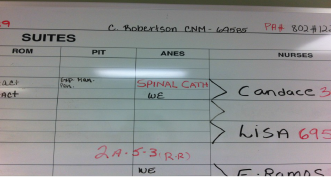
In our institution we have a mix of residents, CRNAs, and SRNAs. Our policy is to thread the epidural catheter intrathecally following an unintended dural puncture during the placement of an obstetric epidural. Unfortunately, in the midnight hours a parturient with an intrathecal catheter was taken to the OR for an emergent Caeserean section and due to a breach in communication was administered a large volume of local anesthetic. The high block was detected immediately and an emergent Caesarean section was performed with no adverse outcome to mother or baby. Following this incident we implemented the guidelines in Figure 1, so as to avoid future errors.
Madhumani Rupasinghe, MBBS, FRCA Tina Houseworth, CRNA Peter D. Doyle, MD The University of Texas Medical School at Houston Houston, TX
References
- Halpern SH, Douglas MJ. Evidence-based obstetric anesthesia. Malden, MA: Blackwell Publishing, 2005.
- Sharpe P. Accidental dural puncture in obstetrics. BJA CEPD Reviews 2001;1:81-4.
- Tourtellotte WW, Haerer AF, Heller GL, Somers JE. Post lumbar puncture headache. Springfield, IL: Charles C Thomas, 1964.
- Chadwick HS. An analysis of obstetric anesthesia cases from the American Society of Anesthesiologists closed claims project database. Int J Obstet Anesth 1996;5:258-63.


 Issue PDF
Issue PDF