Crew Resource Management (CRM) training includes teamwork, communication, decision making, and the routine usage of checklists and protocols. The principles of CRM were developed in high-risk, high-reliability industries where mistakes cause disastrous consequences. In recent years, CRM practices have been introduced to hospitals to improve patient safety. This paper examines the role of debriefing in the operating room, in helping to make the surgical suite safer for patients. As one of CRM’s most powerful tools, debriefing improves communication across disciplines, provides a means for practice improvement, and assures that equipment, personnel, and technology issues are identified and addressed. Communication among professionals in the operating room and the practice of debriefing will be discussed through an examination of the experience of the anesthesia and surgical teams at Memorial Regional Hospital and Joe DiMaggio Children’s Hospital in Hollywood, Florida. It was found that the debriefing tool supports continuous process improvement by encouraging each team member to creatively identify solutions to issues encountered during the perioperative period.
Introduction
Despite continuous improvements in surgical and anesthesia techniques, including the use of less invasive surgical approaches,1 preventable medical errors account for more deaths annually than breast cancer, automobile accidents, or drowning.2 Poor communication among health care workers is widely recognized as the most common cause of these errors,3 with estimates ranging from 43% to 91% of adverse events and near misses in the operating room (OR) attributable to miscommunication.4-6 In response to preventable surgical errors, the Joint Commission Board of Commissioners has mandated strategies for improving communication, including the Universal Protocol for Preventing Wrong Site, Wrong Procedure and Wrong Person Surgery™ (2003) which emphasizes pre-procedure verification, site marking, and a time out.7,8
Hospitals have a vested interest in improving the communications among OR staff, but admonitions and behavioral sanctions are seldom sufficiently effective to reduce OR-related errors and the facility’s concomitant malpractice risk. All too often, the spirit of teamwork and collaboration is not present in a typical operating room setting due to an uneven power dichotomy: the surgeon is the one in charge; other staff members are present to support the surgeon’s role. But this one-sided approach discounts the insights and wisdom of others in the room, sometimes to the detriment of the patient.
The surgical arena is not the only environment that requires thorough communications, teamwork, and decision-making to ensure safety, but other industries have integrated Crew Resource Management (CRM) into their daily practices as a way to promote teamwork, communication, decision making, and the usage of checklists, specific protocols, and algorithms.
CRM-based team training has an excellent track record in overcoming communication and collaboration causes of adverse events in such high-risk, high-reliability industries as aviation, nuclear power, and military operations.9-11 In these industries, CRM has contributed to an 86% decrease in the risk of dying on a U.S. major jet air carrier since the 1990s,12 a 52% reduction of military transport squadrons accidents, and an 81% decrease in U.S. Navy Intruder squadrons accidents, among others.13
With miscommunication significantly contributing to the volume of preventable medical errors, some hospitals have begun to tap into CRM training in recent years and document its positive effects on reducing both surgical mortality and OR delays.14-16 While full CRM implementation is multi-faceted, this paper addresses how surgical team debriefing following the completion of a surgical procedure is key to creating a culture that continuously improves patient safety.
Materials and Methods
Setting
Memorial Healthcare System (“Memorial”), the fifth-largest public health care system in the nation, has a reputation for providing advanced medicine and technology, and high quality health care services to South Florida residents through its 6 hospital facilities. Memorial and its facilities have earned many awards and accolades including the American Hospital Association’s “Living with the Vision” and Foster G. McGaw awards, for which Memorial was selected from more than 5,000 hospitals as the national model for improving the health of the community. Memorial Regional Hospital, the flagship facility of the health care system and one of the largest hospitals in Florida, offers extensive health care services including Memorial Cardiac and Vascular Institute, Memorial Cancer Institute, and Memorial Neuroscience Center. The value of debriefing and communication was explored among OR professionals from Memorial Regional Hospital and Joe DiMaggio Children’s Hospital.
CRM Tools
CRM training was introduced within Memorial in late 2007 with the goals of creating a culture for patient safety through improved communication, teamwork, and decision making among professionals in its operating suites. The assistance of a hospital consulting group with considerable experience in CRM Patient Safety programs was enlisted to help improve patient safety throughout the hospital system. Hospital executives and physician department chairs, in concert with Memorial’s consultants, began introducing teamwork and communication training to each department. Since buy-in from hospital leaders and key physicians was priority, Memorial’s team members worked together to develop specific tools and expected behaviors that would help each of them position patient safety at the forefront of everyone’s job.
A key element in the communication rigor established through CRM is the time out, which empowers each team member to be responsible for patient safety. Conducted just prior to surgical incision, the time-out statement concludes with the safety reminder: “If you see anything you think is unsafe, I expect you to speak up, look for red flags, and use the word ‘delta!’ anytime a full stop is needed.” When any member of the team calls ‘delta,’ that statement requires all action to cease because a team member has identified a serious patient safety issue that requires assessment by the team before proceeding. The willingness of staff to speak out in this way is predicated on strong commitment by top personnel to build an institutional culture for patient safety.
Other CRM tools, such as debriefing, are aimed at increasing communication across disciplines. In a study by Zuckerman, et al., debriefing is described as a process that allows individuals to discuss team performance in a constructive, supportive environment—a process which has been linked to improvements in specific procedures, teamwork and communication, and error identification.17 The Bandari et al. study demonstrated that briefings and debriefings were a practical and successful means of identifying both clinical and operational errors in surgical care.
The OR team debriefing is a very fast post-operative meeting with all members present from a surgery. The lead surgeon calls for input and, with an intentional twist on convention, the least senior member of the team is invited to speak first. The questions to be addressed during the debriefing are:
- What went well?
- What needs improvement (in terms of systems, supplies, staffing, and communications issues)?
- How can these improvements happen?
As demonstrated in these questions, the practice of debriefing provides an opportunity for all involved to identify both what went right with the case and what aspects could have been improved, as also noted in a study by Ahmed et al. that identifies best practices in surgical debriefing across 3 continents. In this manner, the intent is to hardwire teamwork behaviors and open communication into the daily standard of care.
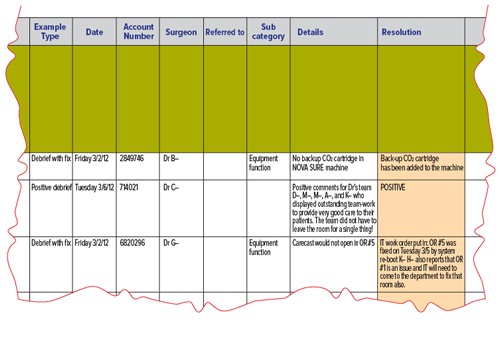
Implicit in the practice of debriefing is the act of follow-up by the institution. Follow through provides an opportunity for continuous improvement not only from the perspective of the team members’ performance but also for the identification of environmental aspects (equipment, supplies, physical layout, etc.) that require attention before the next surgery. Items generated from the previous day’s debriefing are reviewed in the morning OR report by the surgical director, giving staff the assurance that the work they are doing in the debriefing is being put to good use. It is the responsibility of the circulator to communicate specific problems identified in the debriefing session to specific individual(s) who would be responsible for taking corrective action, generally within 12-48 hours. For example, if missing equipment or instruments were noted, those items would be reported to the equipment sterile processing department. If one of the team members could not properly operate a piece of equipment, that person would be referred to the person in charge of OR personnel for follow-up education. Likewise, Bandari et al. describe how the list of defects identified during briefing and debriefing should be sent to administrative personnel on a weekly basis and to the hospital administration on a monthly basis.18 (An example form used during the debriefing process is shown in Figure 1, and an example of how the circulator will communicate follow-up issues to the various hospital departments is shown in Figures 2 and 3 on the following pages.) As in Berenholtz’s study, Memorial’s staff members use this information for continuous process improvement and feedback to hospital personnel.
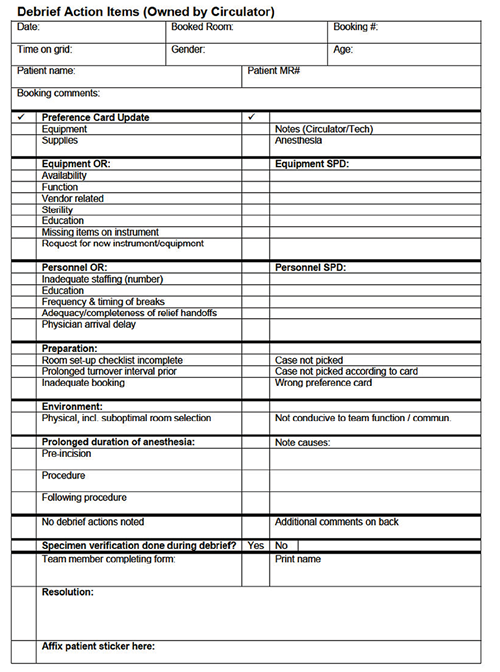
Figure 1. Example of debriefing form.
Results
Through CRM training that emphasizes communication and standardized processes, Memorial has experienced outcomes that include improved quality, improved safety, reduced untoward outcomes and sentinel events, improved patient experience, and improved patient satisfaction. Although it is a natural and inevitable human condition to revert back to poor habits, CRM eliminates such process and protocol variability, substantially reducing this creep towards previous habits by requiring conscious effort and concentration at the point of care.
Memorial saw significant increases in safety, communication, and satisfaction in every hospital as a result of implementing CRM and as evidenced through Memorial’s safety culture survey scores. A year following the implementation of CRM training, physician satisfaction increased substantially in every category, including perception of overall quality, place to practice, patient safety, teamwork collaboration with nursing, and communication with nursing.
In addition to physician satisfaction, Memorial’s staff members developed an extraordinary sense of teamwork combined with a high degree of personal responsibility to assure patient safety, as demonstrated by the 2010 safety survey. Here, teamwork within units and employee satisfaction experienced significant increases across every hospital. In this way, the standardization of communication procedures that CRM facilitated has created an environment where all employees are able to proactively contribute to patient safety.
CRM also contributed to significant improvement in terms of handoffs and transitions as well as improvements across other departments that utilized CRM training, including the radiation oncology department. Since implementing CRM in the radiation oncology department, none of its treatments have deviated from the treatment plan, and the department has been able to identify situations where ambiguity or conflicting documentation could have resulted in inappropriate treatment or significant patient harm.
However, not all departments saw significant increases. While moderate or mild increases were also common, pockets of low performance did exist, too. These pockets of low performance may be due to lack of management commitment or support, fewer experienced employees, or other external events. Although some departments demonstrated weaker results than others, CRM has greatly affected each of Memorial’s 6 hospitals by instituting a wide-ranging organizational culture change.
Examples
To further demonstrate how debriefing works to facilitate teamwork and promote a better culture for patient safety, we present several examples—some fairly straightforward and some that address the very core of teamwork and communication issues within the operating suite. It is our intent to demonstrate how the actions generated from debriefing can range from quick fixes to much more detailed solutions.
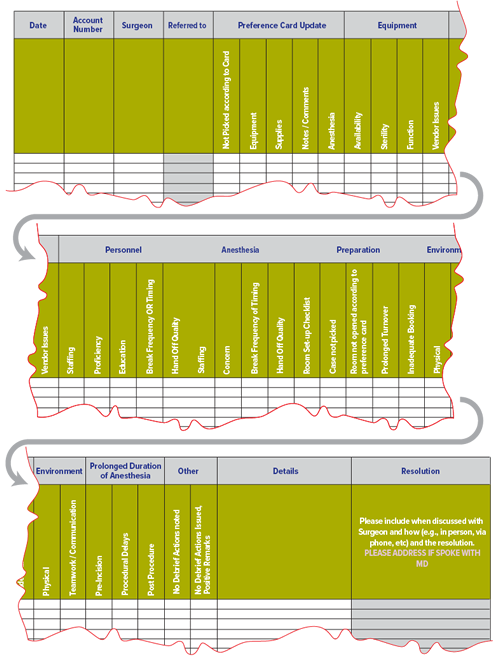
Figure 2. Example of form used to facilitate follow-up communication.
Environmental Factors
During open-heart surgery, a monitor measures brain function and blood flow to the brain during cardiopulmonary bypass procedures. In one such procedure, the view of this monitor was obstructed by other equipment. Since the monitor’s information was not visible to all the staff, appropriate adjustments during the surgery were not made as quickly as they otherwise would have been. In the debrief, the OR staff noted this and made a recommendation for future equipment placement that is visible to all staff throughout the procedure.
Protocol Development
After separating a pediatric patient from cardiopulmonary bypass and experiencing difficulty ventilating the patient, the anesthesia team recognized that they should perform more frequent blood gas analysis to ensure that the patient is appropriately ventilating and oxygenating post bypass. In the debriefing that followed, the anesthesia team developed a protocol that is now used routinely to ensure optimal ventilator management for the patient after separation from cardiopulmonary bypass.
Briefing Information
In one cardiac debriefing session, the team identified that by routinely addressing the type of anticoagulant the patient is taking during the presurgical briefing sessions, each team member would be more alert as to how it might affect the patient’s response to surgery. By incorporating information about the type of anticoagulant the patient has been taking and whether that anticoagulant is still in the patient’s system at the time of the surgery, greater focus can be brought to this issue prior to the procedure.
Tunnel Vision
A female patient was to receive a tracheostomy as a palliative measure. As is typical the surgical team expected a 30-minute procedure. However, the surgeon encountered difficult anatomy and consequently performed a major neck dissection and at one point considered aborting the procedure. After 90 minutes of surgery, convinced that he had identified the trachea, the surgeon placed a tracheostomy tube and asked that ventilation be initiated via the newly placed tracheostomy tube. It was immediately obvious that the tube was misplaced as there was no clinical evidence of ventilation and at this point the 3 anesthesiologists in the OR asked the surgeon to remove the tracheal tube so that the patient could be intubated transorally and ventilated. The surgeon insisted that he was in the airway.
Despite the anesthesiologists’ multiple invocations of delta (the signal to stop everything), he did not stop surgery and would not remove his hands from the field. The nursing staff present additionally invoked delta, but the surgeon did not respond to the other team members and continued with this course of action. The patient suffered a cardiac arrest secondary to progressive hypoxia. In desperation, one of the anesthesiologists reached with an unsterile hand into the surgical field and physically removed the surgeon’s hands so that the patient could be intubated transorally. The patient could not be resuscitated.
Here, the debriefing documented that the surgeon did not honor the delta. As a result, the Director of Medical Affairs counseled with the surgeon to make clear the expectations for communications in the operating room and response to delta. Moving forward, other operating room personnel have become empowered to move up the chain of command quickly whenever there is a concern about the effects of tunnel vision and a provider ignores delta.
Staff Empowerment
Upon arriving to the OR at 6:30 a.m., the anesthesia attending was greeted by 3 agitated nurses who had assisted with a combined neurosurgery, plastics, and ENT case that had begun the previous morning, approximately 22 hours ago. While obtaining a report from the departing night nurses, they were concerned about surgeon fatigue, the need to assess the patient’s status, the need for patient repositioning, and the appropriateness of keeping the patient under anesthesia for such a long period of time. With the knowledge that the Chief of Anesthesia was out of town, the attending realized that it was their responsibility to address this situation.
The anesthesiologist recounts that they marshaled courage to question the surgeon and call for a delta. The anesthesiologist indicated that they were documenting their request for a time out to ask some specific questions: Do you need extra help? Do you need another surgeon? Do you need any extra equipment? The anesthesiologist also requested that the patient’s coagulation and hematologic status be assessed, the patient be repositioned, and the advisability of proceeding to operate be discussed. The surgeon responded appropriately to the delta, the patient was assessed and repositioned, and the surgery was concluded quickly thereafter.
In this case, the debriefing session identified such issues as the risks of keeping the patient under prolonged anesthesia, the need for periodic repositioning, and the importance of periodic reassessment when the procedure is prolonged. Additional cross departmental meetings led to the development of a protocol that requires an automatic delta after 8 hours for reassessment and joint planning. This new protocol will guide staff the next time a similar situation occurs.
The anesthesiologist noted that the CRM training and strong support of superiors created a collaborative culture that empowered them to act on behalf of the patient and staff.
Interventional Radiology Suite
In addition to Memorial’s OR suite, quality and safety in Memorial’s Interventional Radiology Suites were improved due to the increases uniformity that the CRM process encourages. The reduction of untoward outcomes and sentinel events, improved experience and improved patient satisfaction were the result of the patient being included as a team member who could participate in the pause and call out any red flags of concern. Empowering the patient to ask questions has been found to increase the patient’s confidence in the physicians, team members, and overall experience.
Discussion
At the outset of the implementation of the CRM Patient Safety System at Memorial, a point of resistance by surgeons and anesthesiologists was the concern that debriefing would add time in the OR after the conclusion of the case. While the value of the routine use of debriefing is huge, the time required to do it is modest. In a study involving more than 37,000 cases in a large medical center, Berenholtz et al. found that debriefing took an average of 2.5 minutes to complete. Contrary to expectations, what Memorial’s OR teams have found is that debriefing actually makes their surgeries more efficient and take less time because less time is spent leaving the sterile field to acquire additional needed instruments or assemble equipment. In this way, the pivotal nature of the debriefing tool has been a major driver of change both in the daily practice of Memorial’s surgical suites, in terms of making things work more efficiently and effectively and in bringing about specific changes to protocols to assure patient safety.
Parallels with Military Debriefing
Debriefing has been an important performance tool in the military since World War II when it was used to question soldiers at the conclusion of a mission,19 and it continues to be routinely used today by military flight personnel at the conclusion of every flight and mission. Drawing the parallel between military pilots and surgical teams, Zuckerman et al. notes that mistakes have drastic consequences, so the goal of debriefing is to minimize mistakes and to repeat them with lessening frequency.17
The act of reflection has been shown to be a critical element in adult learning,20 so it is not surprising that debriefing after military operations emphasizes the significance of learning from the experience.21 Furthermore, the more that people associate debriefing with ordinary events, the better debriefing can be integrated into a company’s everyday activities.22
Airborne Warning and Control System (AWACS) navigators, for instance, manage to keep debriefing top of mind throughout their missions, noting any problems encountered, especially if the problems will impact later parts of the mission.23 As noted by Armistead, the debriefing process may occur at multiple intersections during a mission: if the weapons unit is not controlling fighters, they will debrief their missions internally and prepare debriefs to send to the fighter pilots; during the flight home, the technicians will note any problems to debrief with maintenance. Then, after the crew secures the aircraft, they debrief among themselves to evaluate how well they accomplished their training objectives. In this way, AWACS navigators utilize 2 forms of debriefing: the individual crews have the mission debrief on the plane, and then each crew comes together to have a debriefing session as a whole.
The length of such AWACS missions may be analogous to a long transplant case where the surgeon will remain in surgery but the teams change, including anesthesia providers and other surgical team members, thereby having different crews start and finish the procedure. In cases like this, with extended timeframes and multiple “crews,” a joint mission debriefing at the end may be beneficial to ensure critical findings are not missed.
Short cases raise similar yet opposing questions about the need for debriefing. When asking whether or not debriefing is necessary after every short case when the same team is present, one can refer to the process of stealth fighters who often land and take off again without turning the engine off yet still complete a minute debrief over the radio. In the same manner, if a procedure takes a matter of minutes in the OR, the team should still quickly note if improvements or problems were found, and at the end of a series of 4 or 5 cases, the OR team can then take a more thorough look at the cases.
Egalitarianism and Tunnel Vision
The emphasis on egalitarianism within the operating suite has not been without its challenges. Anesthesia professionals routinely provide debriefing to their trainees, making it ingrained in the culture of their specialty, but the same was not found to be true among surgeons, as Ahmed et al. noted.24 Although top down change is a challenging tranisition for surgeons who are accustomed to being in charge, Memorial’s commitment to the speedy resolution of problems identified in the debriefing process has real appeal for them.
Unfortunately, in example #4, Tunnel Vision, the surgeon had lacked situational awareness and had developed tunnel vision. This singular focus on one aspect, to the exclusion of everything else, is also noted by the National Transportation Safety Board (NTSB) as the reason for the crash of Eastern Airlines Flight 401 near the Miami airport in 1972. Members of that crew were so preoccupied with a malfunctioning indicator that they failed to monitor other instrumentation that would have informed them of their unexpected descent soon enough to prevent a crash into the ground. The plane was destroyed; of the 163 people aboard, 101 died from their injuries. The NTSB report observed that distraction, confusion, and lack of effective coordination among the crew led to the event.25 In our surgical example, the invocation of delta was an attempt to interrupt the surgeon’s tunnel vision, but that same distracted preoccupation led to fatal results.
Continual Process Improvement
As outlined by the methods and results in this paper, Memorial emphasized that each team member, regardless of his or her discipline or status, had an important voice and role in ensuring a safe outcome for the patient. The same dedication to safety holds true in other high risk settings, including military operations where military ranks are temporarily ignored to allow each member to become an equal witness for the duration of the debriefing, as noted by Armistead.
In both industries, recording action items from the debriefing session has proven to be a rewarding process in itself because it leads to continual process improvement. In Memorial’s OR environment, for instance, the right instruments for the specific surgeon and procedure are now prepared correctly the next time and the equipment found to be deficient the previous week is now corrected in advance. When deficiencies are corrected promptly and consistently, trust between staff and the hospital builds, and the surgeons are more likely to participate in other aspects of the CRM process as well.
Still, unwavering, impassioned commitment from all senior health care system executives has been the key to implementing the CRM Patient Safety System. From Memorial’s Chief Executive Officer to the Chief Medical Officer, Chief of the Department of Anesthesia, and Chiefs of all surgical departments, their commitment to cultural change in the interest of patient safety has set the tone for conduct within the operating suites. Reinforcement from the top produces changes that support the collaborative culture necessary for improved patient safety. In this way, patients are receiving safer care, and all of Memorial’s staff members are challenged to bring their very best efforts each day on behalf of their patients.
Conclusion
With dysfunctional communication patterns responsible for a considerable portion of adverse events in the hospital setting, effective CRM training in other high risk industries is gaining appeal. But change routinely meets with resistance. Strong leadership from the top levels of the organization has proven to be the key to effective implementation within Memorial. By concentrating on the successes garnered through a well implemented debrief and follow-up process, surgeons, anesthesia professionals, and staff are more likely to be open to the other aspects of the CRM Patient Safety System. By encouraging all members of the team to be fully involved in assuring the patient’s safety, hospitals can draw on the full capabilities of their team members to continually improve their practice. Memorial highly recommends this approach to creating a culture of patient safety.
References
- Pronovost PJ, Freischlag JA. Improving teamwork to reduce surgical mortality. JAMA 2010;304:1721-2.
- Hoyert DL, Kung HC, Smith BL. Deaths: preliminary data for 2003. Natl Vital Stat Rep 2005;53:1-48.
- Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academy Press, 2000.
- Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care 2004;13:330-4.
- Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis of errors reported by surgeons at three teaching hospitals. Surgery 2003;133:614-21.
- Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med 2004;79:186-94.
- The Joint Commission. Universal protocol. Available at: http://www.jointcommission.org/standards_information/up.aspx. Accessed March 28, 2013.
- Berenholtz SM, Schumacher K, Hayanga AJ, et al. Implementing standardized operating room briefings and debriefings at a large regional medical center. Jt Comm J Qual Patient Saf 2009;35:391-7.
- Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res 2006;41:1576-98.
- Salas E, Cannon-Bowers J. Design training systematically. In: Locke EA, ed. The Blackwell handbook of principles of organizational behavior. Malden, MA: Blackwell Publishing, Ltd, 2004:43-59.
- Salas E, Cannon-Bowers JA. The science of training: a decade of progress. Annu Rev Psychol 2001;52:471-99.
- Levin A. “Airlines Go Two Years with No Fatalities.” USA Today January 12, 2009. Available at: http://usatoday30.usatoday.com/travel/flights/2009-01-11-airlinesafety_N.htm. Accessed March 28, 2013.
- Solosky KJ. Crew Resource management. March 20, 2007. Officer.com. Available at: http://www.officer.com/article/10250060/crew-resource-management. Accessed March 28, 2013.
- Nundy S, Mukherjee A, Sexton JB, et al. Impact of preoperative briefings on operating room delays: a preliminary report. Arch Surg 2008;143:1068-72.
- Henrickson SE, Wadhera RK, Elbardissi AW, Wiegmann DA, Sundt TM III. Development and pilot evaluation of a preoperative briefing protocol for cardiovascular surgery. J Am Coll Surg 2009;208:1115-23.
- Neily J, Mills PD, Young-Xu Y, et al. Association between implementation of a medical team training program and surgical mortality. JAMA 2010;304:1693-700.
- Zuckerman SL, France DJ, Green C, Leming-Lee S, Anders S, Mocco J. Surgical debriefing: a reliable roadmap to completing the patient safety cycle. Neurosurg Focus 2012;33:E4.
- Bandari J, Schumacher K, Simon M, et al. Surfacing safety hazards using standardized operating room briefings and debriefings at a large regional medical center. Jt Comm J Qual Patient Saf 2012;38:154-60.
- Schenarts PJ. Debriefing is an effective method for providing feedback and ensuring adherence to best clinical practice by residents in the intensive care unit. Crit Care Med 2007;35:957-8.
- McGreevy JM, Otten TD. Briefing and debriefing in the operating room using fighter pilot crew resource management. J Am Coll Surg 2007;205:169-76.
- SLA Marshall’s contribution to CISD. International Combat Stress Conference: Debriefing History. Available at: http://tservcsc.bizhosting.com/cisdhist.html. Accessed March 28, 2013.
- Guterman J. The lost (or never learned) art of debriefing. Harvard Management Update. 2002;7:3.
- Armistead, E. AWACS and hawkeyes: The complete history of airborne early warning aircraft. St. Paul, MN: MBI Publishing Company, 2002: 82-84.
- Ahmed M, Sevdalis N, Paige J, Paragi-Gururaja R, Nestel D, Arora S. Identifying best practice guidelines for debriefing in surgery: a tri-continental study. Am J Surg 2012;203:523-9.
- Williams S. Eastern Airlines Flight 401 accident – aviation human factors case study. Aviation Glossary.com. Available at: http://aviationglossary.com/eastern-airlines-flight-401/. Accessed March 28, 2013.
Statement of Conflict of Interest
None of the authors have conflicts of interest relating to the publication of this paper. The first 5 authors are on staff of the hospital system; the final author is on staff with the consulting entity. No funds exchanged hands to make joint submission of this article possible.
We acknowledge the numerous staff members who were willing to provide information through on-site interviews as well as the senior administrators of the health care system who have strongly supported this cultural-change effort and the writing of this article. Specifically, we acknowledge Jean Miles, MD, Vice Chief of Anesthesiology and Mark Korenge, MD, Anesthesiologist, both of Memorial Regional Hospital in Hollywood, Florida, and Adam L. Blomberg, MD, National Education Director, Anesthesiology Division, Sheridan.
Stanley W. Marks, MD, FACS, Senior Vice President and Chief Medical Officer, Memorial Healthcare System, Hollywood, FL
Joseph Loskove, MD, Chief of Anesthesia, Memorial Healthcare System; Chief of Anesthesia, Memorial Regional Hospital; and Regional Medical Director, Sheridan, Sunrise, FL
Andrew Greenfield, MD, Senior Vice President of Anesthesia Division, Sheridan, Sunrise, FL; Formerly, Chief of Anesthesiology, Memorial Regional Hospital
Richard E. Berlin, MD, Vice-Chief of Pediatric Anesthesia, Joe DiMaggio Children’s Hospital, Memorial Regional Hospital, Hollywood, FL
Jennifer Kadis, MSN, RN, CPAN Director of Clinical Effectiveness, Memorial Healthcare System, Hollywood, FL
Richard Doss, BSB, Senior Advisor: Performance Breakthroughs and Strategy, LifeWings Partners, LLC, Minneapolis, MN


 Issue PDF
Issue PDF