Related Article:
National Partnership for Maternal Safety— Maternal Safety Bundles
The United States is one of only eight countries worldwide and the only developed nation where maternal mortality has increased since 1990.1 Parturients in this country are three times more likely to die from pregnancy-related complications than women in Britain, Germany, or Japan.1 These findings are shocking, especially considering that prior to 1982 maternal mortality in the United States had improved dramatically over the last century.2 Improvement in survival can be attributed to advances in medical care, more hospital deliveries by those trained in obstetrical care, and better aseptic technique.3
Traditionally, the most common causes of maternal death have been hemorrhage, hypertensive disorders, thromboembolic events, and infections.4,5 The proportion of deaths due to conventional causes is now declining and instead a significant proportion of maternal deaths are attributable to cardiovascular conditions and other co-existing medical diseases (Figure 1).5,6 Interestingly, anesthesia complications leading to mortality are becoming rarer. This change underscores the need for anesthesia professionals to not only provide safe labor analgesia and anesthesia for cesarean delivery, but to broaden the scope of their attention to assist women through a safe pregnancy and birth.
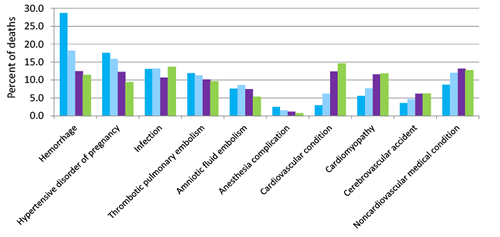
Figure 1. Cause-Specific Proportionate Pregnancy-Related Mortality: United States, 1987–2010.
Not only has maternal mortality increased, but severe maternal morbidity has more than doubled in the 21st century, affecting 50,000 women every year.7 The reason for this change is unclear, but several possible explanations exist. First, we are observing an increased incidence of parturients in the United States with advanced maternal age,8 but this trend is also seen in other parts of the world where mortality rates are not increasing. Second, we are performing a disproportionately high rate of cesarean deliveries as compared to other developed countries,9 which leads to a variety of complications including an increased incidence of placental implantation abnormalities such as placenta acrreta.10 Or, the most compelling explanation is the surge of chronic health conditions such as obesity, hypertension, diabetes, and chronic heart disease in the parturient.6,7,11,12
In response to the increase in maternal mortality and morbidity in this country, a national imperative exists to identify and evaluate the causes of these deaths as well as identify preventable factors. Remarkable progress has been made in the state of California where more than 10% of American births take place. Data published on maternal deaths in California between 2002 and 2004 documented 207 deaths, with nearly 40% of those deaths potentially preventable.13 Three conditions were found to have the greatest level of preventability: obstetric hemorrhage, deep vein thrombosis, and preeclampsia/eclampsia. In response to these findings, the California Maternal Quality Care Collaborative created free online “toolkits” available to anyone. Toolkits include a collection of articles, guidelines, implementation guides, and educational documents with the goal of preventing death in the parturient. The first toolkit released was on obstetric hemorrhage. Many hospitals in California used the toolkit to implement efforts at their institutions to actively decrease maternal hemorrhage and morbidity and mortality stemming from it. Over the next five years, maternal mortality in California decreased dramatically as compared to the national maternal mortality rate that continued to increase from 2008 to 2013 (Figure 2).
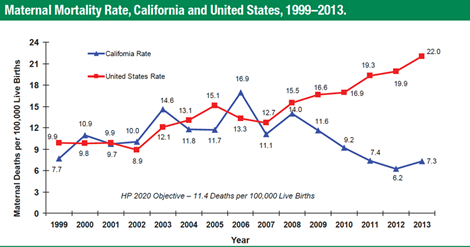
Figure 2. Source: State of California, Department of Public Health, California Birth and Death Statistical Master Files, 1999–2013. Maternal mortality for California (deaths ≤ 43 days postpartum) was calculated using ICD-10 cause of death classification (codes A34, O00–O95–O99). United States data and HP2020 Objective use the same codes. U.S. maternal mortality data are published by the National Center for Health Statistics (NCHS) through 2007 only. U.S. maternal mortality rates from 2008 through 2013 were calculated using the CDC Wonder Online Database, accessed at http://wonder.cdc.gov on March 11, 2015. Produced by California Department of Public Health, Center for Family Health, Maternal, Child and Adolescent Health Division, May, 2015. (https://www.cdph.ca.gov/data/statistics/Documents/2013MaternalMortalityRates-SlideSet%20for%20MCAH%20Website.pdf – Last accessed 08/09/2016)
The effectiveness of instituting protocols with the intention of reducing maternal hemorrhage has been evaluated. Looking at over 32,000 deliveries during the periods before and after institution of a hemorrhage protocol, one group of investigators observed a significant reduction in blood products transfused and a nonsignificant reduction in the number of puerperal hysterectomies performed.14 These findings provide the best evidence to date that increasing education and resources and providing toolkits may have a real impact on patient outcomes.
New York took its own initiative to decrease maternal mortality. In 2013, a group of clinicians met together with leaders from The American Congress of Obstetricians and Gynecologists (ACOG) District II, an area covering the state of New York, to create the Safe Motherhood Initiative (SMI). They were encouraged by success stories of systematic educational interventions that led to decreased mortality elsewhere. For example, the United Kingdom created a national effort to reduce the incidence of pulmonary embolism in pregnancy, and mortality from embolic disease subsequently decreased.15 Consequently, SMI included standardized risk-assessment tables, protocols, checklists, and algorithms to minimize variability in practice. Finally, three bundles were created: one on hemorrhage, one on hypertension, and one on venous thromboembolism (VTE). They then created bundle boxes under the safe motherhood website and even offered Continuing Medical Education to encourage clinicians to visit their website. Bundle boxes include a binder with implementation guidance, including posters, brochures, checklists, algorithms, and tables. They also offer a variety of PowerPoint and audio recordings archived on the website to assist in learning. Those who developed and implemented the bundles provide practical advice on implementation.
Four years after he led the efforts in California, Dr. Eliot Main issued a call to action to bring similar resources and infrastructure to a national stage. Representatives from a variety of organizations met in Atlanta in 2012 to create a collaborative approach to optimize maternal health and improve maternal care. The group set priorities for implementation and deployment of efforts focusing on obstetric safety. These meetings resulted in formation of the National Partnership for Maternal Safety (NPMS), housed within the Council on Patient Safety in Women’s Healthcare. Its mission is to “continually improve patient safety in women’s health care through multidisciplinary collaboration that drives cultural change.” An important element of the NPMS is the wide range of professional organizations included in this coalition (Table 1).
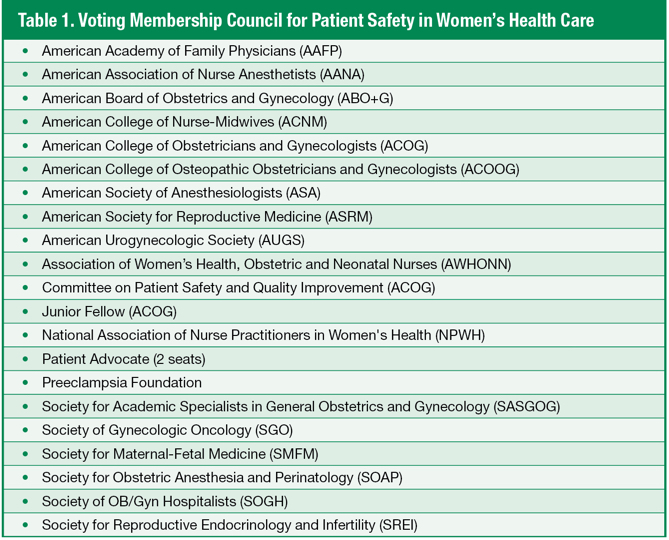
The NPMS goal is to reduce maternal morbidity and mortality in the United States by 50%. One means of accomplishing that was to create bundles—evidence-based interventions that are designed to be implemented together resulting in improved outcomes16—similar to those created in California. NPMS began by creating materials on three topics: hemorrhage, hypertension in pregnancy, and VTE, and published their findings on the website:
http://www.safehealthcareforeverywoman.org/. All the information on the website is free and available to the public, but a login and password is needed to access the site to help the NPMS keep track of who utilizes the information.
The process of making the bundles available to the public is a stepwise process. First, a one-page document is published online which includes links to critical information and implementation guidance. Then, a formal detailed article is published in a variety of high-impact journals. The core of the NPMS is its commitment to being a multidisciplinary group. The publication of the bundles in a variety of sources including anesthesia, obstetrics, nursing, and midwifery journals is a testament to this commitment.
Although ACOG has published practice bulletins and committee opinions for years, they have not been multidisciplinary in nature. Bundles are a way of providing a variety of existing evidence-based recommendations, such as ACOG practice bulletins, into an organized and accessible format. Additionally, there is a real emphasis on allowing the individual facility to modify and tailor the bundle to meet local needs. The bundles give examples of different ways of managing and responding to maternal complications that are known to cause significant maternal morbidity and mortality. Each bundle is formatted into four sections: Readiness, Recognition and Prevention, Response, and Reporting/System Learning.
The first bundle, the Obstetric Hemorrhage Patient Safety Bundle, was initially published on the website. Then a more detailed document was published in 2015 in four high-impact journals simultaneously: Anesthesia & Analgesia,17 Obstetrics and Gynecology,18 Journal of Obstetric, Gynecologic, & Neonatal Nursing,19 and Journal of Midwifery and Women’s Health.20 Obstetric hemorrhage is the most common complication of childbirth, but much of hemorrhage-related morbidity and mortality is considered preventable.21,22 Areas for improvement include better recognition and quantitative appreciation of blood loss, increased attention to clinical signs of hemorrhage, quicker restoration of blood volume, and greater emphasis on intervening decisively.23 Goals of the hemorrhage bundle include limiting the proportion of hemorrhage episodes that become severe, decreasing the need for blood product transfusion, and decreasing the frequency of coagulopathy.
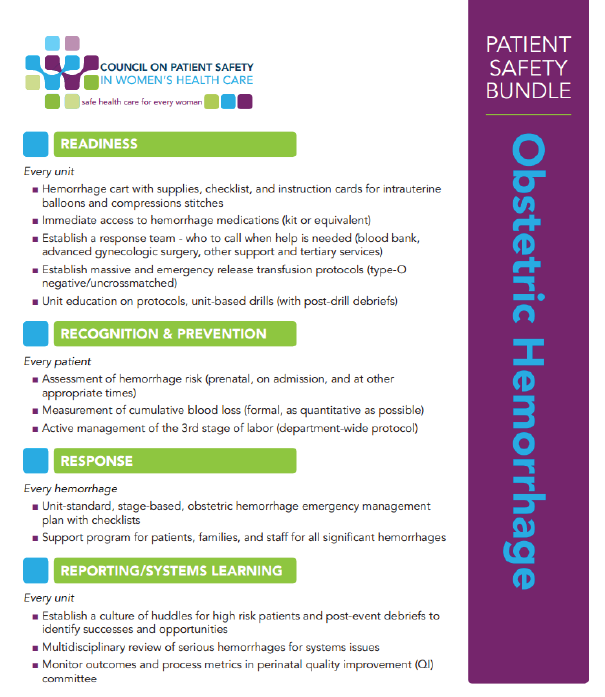
Figure 3. Maternal Safety Bundle on Proactive Establishment of Resources for Management of Obstetric Hemorrhage.
The Readiness section of the hemorrhage bundle includes a list of supplies and systems needed to prepare for hemorrhage, such as a hemorrhage cart and hemorrhage medications. The Recognition and Prevention section includes those assessments that should be performed for every patient, such as accurate measurement of cumulative blood loss. Response includes stage-based obstetric hemorrhage emergency management plans. And finally, the Reporting/System Learning includes recommendations on how to conduct multidisciplinary reviews after severe hemorrhage episodes, including tips for debriefing and perinatal quality improvement committees (Figure 3).
The second bundle, Severe Hypertension in Pregnancy, was recently made available on the above mentioned website. Failure to adequately control blood pressure or recognize the clinical manifestation of preeclampsia such as hemolysis, thrombocytopenia, elevated liver enzymes, and pulmonary edema are leading sources of error leading to grave complications.23 Furthermore, the systolic blood pressure in preeclamptic patients is an important indicator of stroke.24 Therefore, administration of anti-hypertensives in a timely fashion is essential and potentially lifesaving. ACOG has published dosing regimens for labetalol and hydralazine for the initial management of acute severe hypertension in pregnancy, and this guidance has been incorporated into the hypertension in pregnancy bundle.
Like the hemorrhage bundle, the document is divided into four subgroups: Readiness, Recognition and Prevention, Response, and Report/Systems Learning. The Readiness section includes diagnostic criteria and guidance on antihypertensive medications including dosages and administration. The Recognition and Prevention section includes protocols for measurement and evaluations of blood pressure. Response includes management plans for patients with severe hypertension and eclampsia. And, again, Reporting/System Learning includes recommendations on multidisciplinary reviews including debriefing (Figure 4).
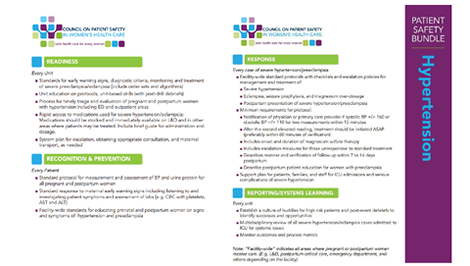
Figure 4. Maternal Safety Bundle for Establishing Protocol and Resources for Management of Hypertension/Preeclampsia.
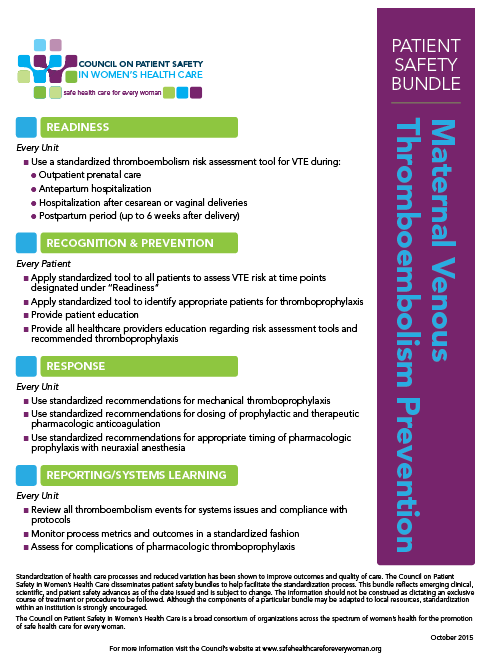
Figure 5. Maternal Safety Bundle for Prevent ion of Maternal Venous Thromboembolism.
As for the VTE draft, it is available on the website now, and the more detailed version is currently being created and due for publication soon. VTE is one of the leading causes of maternal mortality and severe morbidity, but it is largely considered preventable.4 Diligence in administering adequate anticoagulation is crucial. Encouraging data from the United Kingdom demonstrated a reduction in maternal death after implementation of more widespread VTE prophylaxis.15 The Joint Commission requires compression devices on parturients at risk for pulmonary embolism during their cesarean procedure. They also require that high-risk antepartum and postpartum patients be anti-coagulated. The NPMS VTE bundle will include recommendations on who is considered high risk and who should receive VTE prophylaxis. It also will encourage early ambulation and the use of compression devices (Figure 5).
Recognizing that a large percentage of maternal mortality and morbidity is preventable is the key to improving outcomes in the United States. Managing patients with life-threatening emergencies requires clinicians with expertise in resuscitation and critical care. Anesthesia professionals are therefore a vital part of the peripartum team and should take an active stance to limit maternal morbidity and mortality. Now, more than ever, anesthesiologists should act as peripartum physicians and participate with other caregivers to optimize maternal safety and reduce morbidity and mortality.
The authors wish to acknowledge Jill Mhyre, MD, for her assistance in the preparation of this article.
Dr. Jennifer Banayan, MD, is an Assistant Professor in the Department of Anesthesia and Critical Care at the University of Chicago Medical Center. Dr. Banayan has no disclosures.
Dr. Barbara Scavone, MD, is Professor in the Department of Anesthesia and Critical Care and Section Chief of Obstetric Anesthesia at the University of Chicago Medical Center. Dr. Scavone has no disclosures.
References
- Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, Shackelford KA, Steiner C, Heuton KR, et al. Global, regional, and national levels and causes of maternal mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:980–1004.
- From the Centers for Disease Control and Prevention. Healthier mothers and babies—1900-1999. JAMA 1999;282:1807–1810.
- Goldenberg RL, McClure EM. Maternal mortality. Am J Obstet Gynecol 2011;205:293–295.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol 2015;125:5–12.
- Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998 to 2005. Obstet Gynecol 2010;116:1302–1309.
- Kuklina E, Callaghan W. Chronic heart disease and severe obstetric morbidity among hospitalisations for pregnancy in the USA: 1995-2006. BJOG 2011;118:345–352.
- Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol 2012;120:1029–1036.
- Mathews TJ, Hamilton BE. Mean age of mothers is on the rise: United States, 2000-2014. NCHS Data Brief 2016:1–8.
- Betran AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, et al. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol 2007;21:98–113.
- Blanchette H. The rising cesarean delivery rate in America: what are the consequences? Obstet Gynecol 2011;118:687–690.
- Albrecht SS, Kuklina EV, Bansil P, Jamieson DJ, Whiteman MK, Kourtis AP, et al. Diabetes trends among delivery hospitalizations in the U.S., 1994-2004. Diabetes Care 2010;33:768–773.
- Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol 2009;113:1299–1306.
- Main EK, McCain CL, Morton CH, Holtby S, Lawton ES. Pregnancy-related mortality in California: causes, characteristics, and improvement opportunities. Obstet Gynecol 2015;125:938–947.
- Shields LE, Wiesner S, Fulton J, Pelletreau B. Comprehensive maternal hemorrhage protocols reduce the use of blood products and improve patient safety. Am J Obstet Gynecol 2015;212:272–280.
- Lewis G. Saving mothers’ lives: the continuing benefits for maternal health from the United Kingdom (UK) Confidential Enquires into Maternal Deaths. Semin Perinatol 2012;36:19–26.
- Arora KS, Shields LE, Grobman WA, D’Alton ME, Lappen JR, Mercer BM. Triggers, bundles, protocols, and checklists—what every maternal care provider needs to know. Am J Obstet Gynecol 2016;214:444–451.
- Main EK, Goffman D, Scavone BM, Low LK, Bingham D, Fontaine PL, et al. National Partnership for Maternal Safety: Consensus Bundle on Obstetric Hemorrhage. Anesth Analg 2015;121:142–148.
- Main EK, Goffman D, Scavone BM, Low LK, Bingham D, Fontaine PL, et al. National Partnership for Maternal Safety: consensus bundle on obstetric hemorrhage. Obstet Gynecol 2015;126:155–162.
- Main EK, Goffman D, Scavone BM, Low LK, Bingham D, Fontaine PL, et al. National Partnership for Maternal Safety: consensus bundle on obstetric hemorrhage. J Obstet Gynecol Neonatal Nurs 2015;44:462–470.
- Main EK, Goffman D, Scavone BM, Low LK, Bingham D, Fontaine PL, et al. National Partnership for Maternal Safety consensus bundle on obstetric hemorrhage. J Midwifery Womens Health 2015;60:458–464.
- Berg CJ, Harper MA, Atkinson SM, Bell EA, Brown HL, Hage ML, et al. Preventability of pregnancy-related deaths: results of a state-wide review. Obstet Gynecol 2005;106:1228–1234.
- Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW, et al. Frequency of and factors associated with severe maternal morbidity. Obstet Gynecol 2014;123:804–810.
- D’Alton ME, Main EK, Menard MK, Levy BS. The National Partnership for Maternal Safety. Obstet Gynecol 2014;123:973–977.
- Committee Opinion No. 623: Emergent therapy for acute-onset, severe hypertension during pregnancy and the postpartum period. Obstet Gynecol 2015;125:521–525.


 Issue PDF
Issue PDF