Letter to the Editor:
To the Editor:
In response to Drs. Mythen and Grocott…
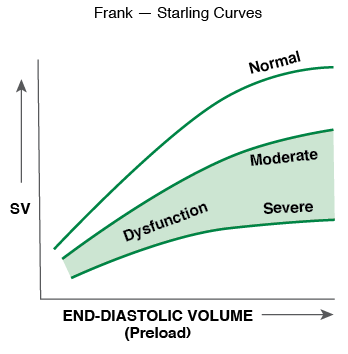
For over 30 years of practicing anesthesiology, I have considered the following physiologic principle when trying to optimize fluid management. Based on the Starling Curve, it is apparent that patients with normal systolic ventricular contractility should be more “fluid responsive” than patients with poor systolic contractility. I believe that much of the recent research and discussion about fluid management has ignored this concept. Patients with poor systolic function are likely to increase their stroke volume over a smaller range of fluid challenges and more likely to develop heart failure and pulmonary edema with larger fluid boluses.
I believe that one of the reasons it is difficult to “optimize” fluid therapy is that we need to consider underlying contractility. Normal ventricles are preload dependent and poor ventricles are less preload dependent and more afterload dependent.
Another reason we have had difficulty in proving that fluid management/“goal-directed therapy” can improve stroke volume and “perfusion” in sepsis is that several existing studies have set lofty and perhaps unreachable goals in their experimental design. Knowing that contractility may be impaired in sepsis, it may be difficult to push the stroke volume to “normal” with just fluid. Inotropes may need to be added for contractile support.
Using goal-directed therapy models to characterize fluid responsiveness and being more generous in those patients with normal systolic function seems prudent. Consideration for judicious fluid administration with the potential addition of inotropes in patients with poor systolic function should be considered. ONE SIZE DOES NOT FIT ALL.
Fred Rotenberg, MD
Assistant Professor of Surgery (Anesthesiology)
The Warren Alpert Medical School of Brown University
Department of Anesthesia, Rhode Island Hospital and The Miriam Hospital, Providence, RI
Dr. Rotenberg has no financial disclosures relevent to this letter.


 Issue PDF
Issue PDF