Dr. Robert K. Stoelting, president of the APSF, and Dr. Robert A. Caplan, staff anesthesiologist and medical director of Quality at Virginia Mason Medical Center and clinical professor of Anesthesiology at the University of Washington in Seattle, WA, co-moderated the APSF Board of Directors Workshop entitled “Current Anesthesia Patient Safety Initiatives—Help Set the Priorities for Immediate Short Term Resolution” at the Anesthesiology 2011 meeting in Chicago, IL, on Saturday October 15, 2011. Opening introductory remarks were made by Dr. Stoelting and Dr. Mark A. Warner, president of the American Society of Anesthesiologists and member of the APSF Board of Directors, respectively. Dr. Caplan’s presentation followed these remarks and was entitled “What Do the Closed Claims Data Tell Us?” He presented data from the ASA Closed Claims Database highlighting the anesthesia areas with the highest proportion of medicolegal claims from 1990 or later. He discussed the most common damaging events in anesthesia claims and the areas with the highest severity injuries. Dr. Caplan noted that the ASA Closed Claims approach has been to identify recurring patterns of injury and provide suggestions for prevention, thus benefiting patients, anesthesia professionals, and insurers. He suggested we broaden the scope of future patient safety initiatives to include issues pertaining to surgeons and nurses as well. These initiatives should be embedded in our training programs so that future health care providers can “grow up” in a culture of patient safety. Dr. Caplan suggested that we should view risk management as risk reduction and provide a way to fail safely with redundancies built into the provision of health care. He felt that the most effective and efficient approach to improving patient safety is by identifying specific patient safety targets and measuring the effect of initiatives with pre- and post-intervention measurements.
Dr. David Gaba, professor of Anesthesia, associate dean for Immersive and Simulation-based Learning, Stanford University School of Medicine and staff physician, VA Palo Alto Health Care System, followed by discussing “How to Evaluate Targets for Safety Intervention.” He noted that most patient safety issues can be categorized as specific problems (phenotype), such as fire safety in the operating room, or deeper-level issues (genotype), such as teamwork and communication, production pressure, and developing a culture of safety. Dr. Gaba felt that specific issues may be more amenable to quicker resolution, but that they would have a high likelihood of recurrence unless we also work on the deeper level patient safety issues. He believed that both types of patient safety issues should be addressed simultaneously, and that deep problems would require sustained efforts and collaboration over decades with fundamental changes in health care organization and structure.
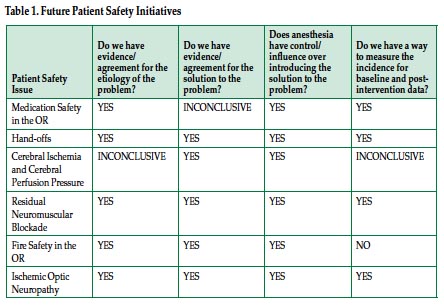
Following these 2 overviews, 6 speakers each presented a specific patient safety issue and addressed the following 4 questions: 1) “Do we have evidence/agreement for the etiology of the problem?” 2) “Do we have evidence/agreement for the solution to the problem?” 3) “Does anesthesia have control/influence over introducing the solution to the problem?” and 4) “Do we have a way to measure the incidence for baseline and post-intervention data?”

APSF Workshop speakers included (left to right): Dr. John C. Drummond, University of California, San Diego and VA Medical Center, San Diego, CA; Dr. Matthew B. Weinger, Vanderbilt University School of Medicine; Dr. Lorri A. Lee, University of Washington; Dr. David Gaba, Stanford University School of Medicine; Dr. Robert C. Caplan, Virginia Mason Medical Center and University of Washington; Dr. Mark A. Warner, ASA President and Mayo Clinic College of Medicine; Dr. Robert K. Stoelting, APSF President; Dr. Jeffrey M. Feldman, Children’s Hospital of Phiiladelphia and University of Pennsylvania School of Medicine; and Dr. Sorin J. Brull, Mayo Clinic College of Medicine.
A synopsis of the answers to these questions for each patient safety issue is presented in Table 1 below with more detailed answers at the following link: https://www.apsf.org/announcements.php?id=11.
Presentations and speakers included “Medication Safety in the Operating Room (Standardization, Technology, Pharmacy/Prefilled, Culture)” by Donald E. Martin, MD, Professor of Anesthesiology, associate dean for Administration, Penn State University College of Medicine, Hershey, Pennsylvania; “Physician Hand-Offs—A Role for a Checklist?” by Matthew B. Weinger, MD, Norman Ty Smith chair in Patient Safety and Medical Simulation professor of Anesthesiology, Biomedical Informatics, and Medical Education, Vanderbilt University School of Medicine; “Cerebral Ischemia and Cerebral Perfusion Pressure (What is a Safe Blood Pressure?” by John C. Drummond, MD, Professor of Anesthesiology, University of California, San Diego, staff anesthesiologist, VA Medical Center, San Diego, CA; “Residual Effects of Neuromuscular Blockers into the Postoperative Period” by Sorin J. Brull, MD, FCARCSI (Hon) and professor of Anesthesiology, Mayo Clinic College of Medicine; “Fire Safety in the Operating Room (Oxygen as a Drug in the Presence of an Unsecured Airway)” by Jeffrey M. Feldman, MD, MSE, Division Chief, General Anesthesia, Children’s Hospital of Philadelphia and clinical associate professor of Anesthesiology, University of Pennsylvania School of Medicine; and “Postoperative Visual Loss from Ischemic Optic Neuropathy After Spinal Fusion Surgery” by Lorri A. Lee, MD, associate professor, Department of Anesthesiology and Pain Medicine, University of Washington, Seattle, WA.
Following these presentations, the audience of approximately 700 Anesthesiology 2011 meeting attendees was polled using an audience response system (ARS) to help prioritize future patient safety initiatives. Of over 200 responses, 90% were anesthesiologists, and 89% had been in practice for more than 10 years. Of the audience members responding, personal (or a colleague’s) experience with these patient safety issues occurred in the following descending order: respiratory compromise from residual neuromuscular blockade (89%), adverse effects from medication errors (84%), adverse event related to a physician hand-off (68%), operating room fires related to supplemental oxygen use (49%), postoperative ischemic optic neuropathy (41%), and postoperative cognitive dysfunction following anesthesia in the beach-chair position (17%). The top 3 patient safety issues that audience members selected as having evidence/agreement to the etiology and solution to the problem, as well as control/influence over introducing the solution to the problem, included fire safety in the operating room, medication safety, and residual neuromuscular blockade. The top 3 patient safety issues that members felt would improve patient safety without an increased investment in technology included hand-offs, residual neuromuscular blockade, and fire safety. Sixty percent of respondents believed that improvements in medication safety would require an increased investment in technology.
The session closed with Dr. Stoelting thanking the audience and speakers for their participation in helping prioritize patient safety initiatives for the future. He subsequently noted recent efforts that have been taken to improve patient safety on these issues including recent APSF workshops on medication safety and cerebral perfusion pressure in the beach-chair position, a special APSF research grant for the study of cerebral perfusion in the beach chair position, a recently released DVD sponsored by the APSF in conjunction with the ECRI Institute on prevention of fires in the operating room (available for download free on the APSF website apsf.org), the ASA Postoperative Visual Loss Registry and its associated recent multicenter case control study, and an ASA task force on the topic of hand-offs.


 Issue PDF
Issue PDF