Both the Scientific and the Technical Exhibits at the October American Society of Anesthesiologists (ASA) Annual Meeting in Chicago featured anesthesia patient safety as a significant component theme. The scheduling of the exhibits at the meeting reflected the new ASA meeting compressed format in that the Exhibits opened Saturday, October 15, at 11 am and closed Monday, October 17, at 3 pm. New and recurrent patient safety concerns were presented throughout the Exhibits along with proposed technical and educational safety improvement strategies.
Widespread Scientific Safety Subjects
In the Scientific Exhibits, safety-related topics varied widely, from some with the greatest impact to others that might appear somewhat mundane, but that still represent everyday hazards persisting as threats to patients. Also, high-fidelity simulation was featured as an integral part of more exhibits than ever before.
Several exhibits displayed educational programs aimed at anesthesia professionals and intended to improve patient outcomes, such as in caring for morbidly obese patients or children with congenital vascular or lymphatic malformations of the head and neck causing difficult airway situations. Likewise, there was emphasis on practitioners learning to use ultrasound guidance for initiating regional anesthesia, either for placing neuraxial blocks in one exhibit or thoracic paravertebral blocks in another.
One educational exhibit from the University of Florida featured 2 newly developed simulators—one for skin prepping and the other for central venous catheter (CVC) placement. The CVC simulator was stimulated by a “learning need” demonstrated by an above-average incidence of pneumothorax as a complication of CVC placement. The device has a 3-D component on the monitor screen showing strikingly realistic neck/chest anatomy that incorporates the same type of technology that puts the yellow first-down stripe on the TV image of a football field. The practice needle the student inserts into the mannequin has a sensor on the tip with 6 degrees of freedom so it is mapped in 3-D space by what is essentially radar inside the mannequin, and the needle is shown on the monitor screen passing through the realistic depiction of the internal anatomy. The screen can be moved so only the instructor can see where the needle is going, or turned so the student can also see and correlate tactile with visual senses. Further, the software allows modifications of the anatomy, such as depicting a very obese patient. Another exhibit, from Japan, featured a “knowledge simulator” with dramatic 3-D video images (requiring battery-powered glasses) of relevant anatomy, such as for a brachial plexus block.
Airway management issues, as always, were featured prominently. A technique for nasal intubation using a bougie through the nose and a video laryngoscope in the mouth was demonstrated. A new technique for topicalization of an airway in preparation for awake intubation utilizing a fiberoptic bronchoscope involved a “mucosal atomizing device” that was offered for trial on willing exhibit visitors. A review and update of Rush University’s formal resident training program in advanced airway management was offered at a well-attended exhibit booth. A recurrent Cleveland Clinic exhibit on airway innovation featured a new version of their oral airway design with continuous suction capability, intended to reduce aspiration danger. Also, repeated from last year was the sealed sterile plastic sheath (with both a lens and a suction port orifice at the distal end) that fits over a fiberoptic bronchoscope with the intention of keeping it sterile inside the sheath during use – thus reducing the time involved in turning over the scope between uses, which is intended to increase dramatically the availability of this critical tool.
An exhibit from the University of Pittsburgh addressed the risk of bleeding complications from placing peripheral nerve blocks in patients receiving thromboprophylaxis. Over a period of 9 years, more than 15,000 blocks were placed without observation of any significant bleeding complications.
An excellent example of high-fidelity simulation was exhibited in a presentation from Johns Hopkins that recreated a remarkably dramatic explosive airway fire that can occur when a surgeon uses an electrocautery to incise a trachea containing 100% oxygen.
Safe medication practices in the OR were emphasized in an exhibit from Emory University regarding breaches in correct techniques of safe medication utilization involving, for example, sterility of IV medications and also the reuse of “single-use” vials allegedly to reduce cost, waste, and environmental burden. Results of an anonymous survey about exactly what anesthesia professionals really do in the operating room in day-to-day practice were cited as the stimulus demonstrating the need for the teachings in this exhibit.
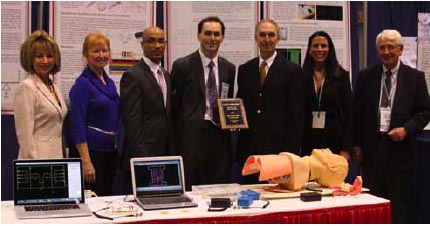
Members of the APSF award the Ellison C. (‘Jeep’) Pierce Best Scientific Exhibit in Patient Safety at the ASA meeting on Sunday, October 16th, 2011 in Chicago, IL. Photo displays award recipients Christopher Connor, MD, PhD and Eddy Feliz, MD from Boston Medical Center, Boston, MA. Also pictured are: Robert Stoelting, MD, APSF President, and APSF Education Committee members Maria Magro, CRNA; Richard Prielipp, M.D, FCCM; Tricia Meyer, PharmD; Deb Lawson, Certified Anesthesiologist Assistant. The authors developed a simple electronic prototype device to assist in accurate performance during application of cricoid pressure for clinical practice and learning during simulation of Rapid Sequence Intubation (RSI).
An intriguing dual-purpose exhibit from Boston Medical Center was awarded the APSF’s E.C. Pierce, Jr., MD, Award for the best safety-themed Scientific Exhibit. The presenters created a simple sensor with a force transducer that is intended to demonstrate with “stop-light” type signals in real time that cricoid pressure is being performed correctly. In addition, the exhibit was offered as a demonstration of how it is possible to use readily available inexpensive resources to facilitate the translation of a clinical idea for new technology into a working prototype of an invention, thus encouraging more innovation in biomedical devices.
Safety Spirit Also Shines on Technical Side
In the Technical (commercial) Exhibits at the ASA meeting, both the usual presentations as well as a few new displays with patient safety implications were exhibited.
As customary, airway management and safety issues were prominent in the displays. (As often stated in this report, the induction of deep unconsciousness and muscle relaxation before genuine confirmation that a patient’s airway can be comfortably managed and accessed is still [even with all the recent attention and device development] one of the least improved and most dangerous things anesthesia professionals do.) Video laryngoscopes have proliferated greatly and were featured prominently throughout the exhibit hall with heavy promotions. There were many varieties of sizes and shapes, and also models having several different placements for the new improved-resolution video screens. A large assortment of blades was available, including sets with bright color coding for different sizes. In another exhibit, a new version of standard blades for direct laryngoscopy was promoted as significantly improving the operator’s view of the larynx as the blade has 2 different bulbs, an L.E.D. bright white light and a separate UV light. In photographs and the exhibit demonstration, this combination of lights gave clearer, more nuanced visualizations with greater detail and no incandescent glare. A new design of laryngeal mask airway was shown that does not have an inflatable cuff, but rather a circumferential outer edge made of a soft gel-like substance that is meant to conform easily to the pharyngeal wall. Another exhibit again featured laryngeal mask devices with pressure indicators incorporated on the cuff pilot tube to help prevent excessive pressure on the pharyngeal wall that could conceivably cause structural damage of several types.
A genuine advance in “airway” devices was a new type of Magill forceps manufactured by a small Florida company. This instrument has unique features. The arms open in a vertical rather than horizontal axis, and there are no traditional jaws at the distal end (the ones with the sharp serrated edges that often puncture an endotracheal tube cuff during nasal intubations). Rather, there is a metal ring that separates into top and bottom semicircles, allowing the operator to grasp the tube tip firmly and easily with no danger to the cuff and guide the tube into the larynx.
Another new airway tool that has potential special application in ICU patients intubated for extended periods, as well as for acute patients in the OR, was a special catheter intended to clean out the lumen of an endotracheal tube with an inflatable cuff that has an action analogous to that of a Fogarty catheter pulling out a clot from a clogged artery. This could relieve an acute obstruction from a mucus plug or simply clean out accumulated intraluminal secretions that are reducing airway compliance. The periodic prophylactic removal of “biofilm” inside the tube is suggested by the manufacturer to help prevent ventilator-associated pneumonia in ICU patients.
A new exhibit featured a different type of CO2 adsorbent that is not pebble-like granules of the traditional chemicals but, rather, is a solid lithium-based micropore cartridge that is fitted inside the standard absorber head where the granules usually go. It was claimed that this type of device does not absorb volatile anesthetic gases as the granules do, thus reducing total agent use and also promoting significantly faster wash-in and wash-out of inhalation anesthetics. The claim was that this cartridge is much slower to desiccate (reducing the potential for Monday-morning carbon monoxide production) and has much less potential for toxic compound A production. The used cartridges are intended for return to the manufacturer for recycling and reuse in making more cartridges.
With all the recent emphasis from the APSF and other groups on the dangers of narcotic-induced postoperative hypoventilation/respiratory depression, it is logical that manufacturers responded with special efforts to highlight monitoring products designed to detect problems and sound an alarm before patient injury occurs. Several versions of face-mounted sampling devices for expired CO2 detection were shown, including an update of the original dual nasal/oral sampling cannula with an appendage that looks like a small spoon hanging down over and in front of the patient’s mouth to capture mouth-breathing expired CO2. A version of the traditional “venti-mask” O2 face mask now includes an internal catheter sticking down into the inside of the mask that connects to the capnograph sampling line. Another type of approach was an acoustic sensor that is affixed to the neck to “listen” for the rate and qualities of inspiratory sounds that can be automatically analyzed to diagnose central and/or obstructive hypoventilation. A corollary in another exhibit was a bite block intended for use in upper GI endoscopy that now includes both a port for supplemental O2 insufflation and another port for capnographic sampling for ventilation monitoring.
Medication safety in the OR was touted by the various exhibitors of premixed IV medications and also of various labeling systems, including those that will automatically read the barcode on a medication ampule/vial and then print an appropriate label (including date, time, and operator) on the small printer affixed to the side of the anesthesia machine that can be immediately applied to the just-filled syringe of that medication.
The various devices that use infrared light to outline subcutaneous veins so as to facilitate intravenous cannulation have evolved with more configurations, including hand-held, floor-standing, and side-mounted varieties. One model has an “inverse” mode that is intended to illuminate veins below skin of darker colors.

Dr. John H. Eichhorn, Professor of Anesthesiology at the University of Kentucky, Founder of the APSF Newsletter (Editor until 2002), and Consultant to the APSF Executive Committee, shakes hands with the Opening Session speaker for Anesthesiology 2011, Dr. Atul Gawande. Dr. Gawande is an Associate Professor, Harvard School of Public Health, and Associate Professor of Surgery, Harvard Medical School, and New York Times best-selling author of numerous books on improving patient safety.
The panoply of other displays that were offered by multiple manufacturers as promoting patient safety included several types of products that have been presented previously, including ultrasound devices for both vascular access and nerve block placement, infusion pumps with new algorithms and “safer” programming protocols, patient warming devices (particularly this year more fluid warmers), various temperature monitoring techniques (including for brain temperature), and, of course, information management systems that both create highly legible anesthesia records that are more defensible if challenged and also capture maximum demographic and financial information intended to enhance practice revenue generation.
Finally, one of the great bright spots of the Technical Exhibits was the proliferation of high-fidelity simulators of various shapes and sizes intended to teach and help perfect techniques in a multitude of anesthesia procedures. Complementing the familiar mannequin simulators was the addition of several new “virtual reality” type computer-based simulators, particularly ones offering training in placement of regional anesthesia blocks, in some ways similar to at least the idea of the simulator described above in the Scientific Exhibits that teaches CVC placement. It certainly was interesting to walk down an exhibit aisle and see an attendee with a large elaborate video visor on gesturing into thin air (including sometimes extensive “body English”) with the motions of performing a regional anesthetic. Perhaps this is a harbinger of things to come.
Overall, patient safety persisted as a distinct focus among both types of exhibits at the 2011 ASA Annual Meeting. This emphasizes both continued success in improving anesthesia patient safety and also the significant challenges yet remaining.


 Issue PDF
Issue PDF