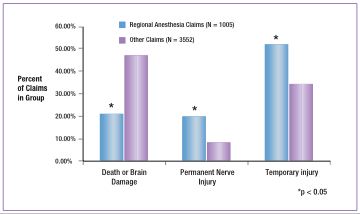
Figure 1: Outcomes in Regional Anesthesia Vs. Other Surgical Anesthesia Claims 1980-1999.
Many anesthesiologists perceive regional anesthesia to be a safer alternative to general anesthesia because it has been associated with reduced postoperative mortality caused by thromboembolic disease and myocardial infarction, improved postoperative analgesia, decreased incidence of early postoperative cognitive dysfunction, and shorter recovery times compared to general anesthesia.1,2 However, significant morbidity may directly result from regional anesthesia. The incidence of cardiac arrest associated with spinal blockade has been reported to be as much as 0.06%, and frequently results in death or brain damage.3-5 Other high severity complications associated with regional anesthesia include epidural hematoma, cauda equina syndrome, and unintentional intravenous injections of local anesthetic. Less severe injuries such as postdural puncture headache, inadequate analgesia, transient paresthesias, and back pain are more frequent sequelae of regional anesthesia. To determine the differences in liability claims associated with regional anesthesia compared to claims associated with other types of surgical anesthesia (general anesthesia and monitored anesthesia care), we utilized the database of the American Society of Anesthesiologists (ASA) Closed Claims Project. Because the database does not contain denominator data on all anesthetics performed, this analysis does not provide information comparing the incidence of injuries between regional and general anesthetics, but offers a perspective on the liability associated with each group. Claims between 1980 to 1999 that were associated with regional anesthesia and other surgical anesthesia were included in this analysis from a database of 5,802. Chronic pain blocks, postoperative pain blocks placed outside the operating room, eye blocks performed by ophthalmologists, and obstetric claims that involved no maternal injury were excluded. A more detailed analysis of regional anesthesia claims including eye blocks and peripheral nerve blocks, as well as a subset comparison of obstetric and non-obstetric neuraxial claims is reported elsewhere.5
Obstetrics was associated with approximately one-third (36%) of the regional anesthesia claims (n = 1005) and significantly influenced the demographics of this group, resulting in significantly more ASA 1-2, young, female patients compared to the other surgical anesthesia group (n = 3551). Epidural anesthesia was utilized most commonly in regional anesthesia claims (42%), followed by spinal blockade (34%), axillary blocks (6%), eye blocks (4%), interscalene blocks (2%), and intravenous regional anesthesia (IVRA).
The regional anesthesia group contained a significantly higher proportion of claims associated with temporary injury and permanent nerve injury compared to the other surgical anesthesia group, whereas death or permanent brain damage was present in a significantly higher proportion of other surgical anesthesia claims (Figure 1).
The primary damaging events (mechanism by which the injury occurs) were block-related in 48% of regional anesthesia claims (Table 1). Complication of block technique was the most common damaging event in these claims.
Table 1. Block-Related Primary Damaging Events in Regional Anesthesia Claims

Regional anesthesia claims with death or brain damage were associated with block-related primary damaging events in 49% of cases. Of these events, neuraxial cardiac arrest (i.e., the sudden onset of severe bradycardia or cardiac arrest during neuraxial block with relatively stable hemodynamics preceding the event) was the most common (37%), followed by unintentional intravenous injection (6%), and other block/anesthesia-related events (6%). In death or brain damage claims associated with regional techniques, the breakdown was as follows: 51% spinal blockade, 41% epidural, 2% interscalene block, 1% axillary block, and 5% miscellaneous blocks.
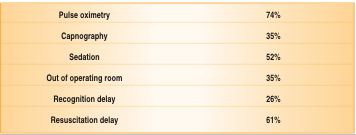
Eighty-four percent of the neuraxial cardiac arrest claims from the 1980s and 1990s (n = 81) were associated with either intentional (70%) or inadvertent intrathecal blockade (14%). The remainder of these claims was associated with lumbar epidural (12%), caudal epidural (2%), and thoracic epidural (2%) anesthesia. Outcome for neuraxial cardiac arrest resulted in death or brain damage in 91% of cases, and was similar between decades. The use of pulse oximetry and capnography in the 1990s claims (n = 31) did not prevent the occurrence of neuraxial cardiac arrest or improve the outcome of death or brain damage compared to the 1980s claims when these monitors were not widely available (Table 2). It is unclear if prevention or resuscitation of neuraxial cardiac arrest has improved over the last decade because the ASA Closed Claims Database lacks denominator data and is biased toward cases with poorer outcomes. Inadvertent intrathecal blocks and occurrence of cases outside the operating room may account for some of the delays in recognition and resuscitation of neuraxial cardiac arrest. The rapid onset of bradycardia/asystole and the intense loss of sympathetic tone caused by spinal blockade (which reduces circulating blood volume) may explain why some cases of neuraxial cardiac arrest may be refractory to prompt treatment.
Table 2. Associated Factors: 1990s Neuraxial Cardiac Arrest Claims (n=31)
A greater proportion of regional anesthesia claims were associated with permanent nerve injury compared to the other surgical anesthesia group (Figure 1). Lumbosacral nerve root, paraplegia, and median nerve damage were significantly more common in the regional anesthesia group compared to the other surgical anesthesia group. Brachial plexus, ulnar nerve, and femoral/sciatic nerve injuries occurred in a greater proportion of other surgical anesthesia claims compared to regional anesthesia claims. Eighty-four claims of injuries to the neuraxis were identified in the regional anesthesia group, and 36 cases (44%) were associated with hematoma. Outcomes for neuraxial injuries, including hematoma, anterior spinal artery syndrome, spinal cord infarct, and other/unknown causes, were poor and resulted in permanent neurologic damage in the majority of cases. Neuraxial injury caused by herniated discs and infections such as meningitis and abscess demonstrated full recovery in the majority of cases. Vascular surgery was the most common operation associated with hematoma (56%), and coagulopathy was associated with 72% (n = 26) of all hematoma claims. Needle trauma above L1 occurred in 17% of hematoma claims with neuraxial injury. The most common presenting symptom was increased motor block out of proportion to the local anesthetic used (83%), followed by increased sensory block (53%), and back pain (25%). A median delay of 1 day from symptom onset to diagnosis was thought to contribute to the poor neurologic recovery in the majority of hematoma claims. Heightened vigilance for symptoms and signs of epidural hematoma (e.g., increased motor block) and prompt diagnostic work-up and treatment may improve neurologic outcome.
Claims associated with regional anesthesia had a significantly lower percentage of claims with payment to the plaintiff compared to the other surgical anesthesia group, a lower median payment, a higher percentage of claims judged to have met appropriate care standards, and a lower percentage of payment in cases with appropriate standard of care. These differences may reflect the greater proportion of regional anesthesia claims with temporary injury compared to other surgical anesthesia claims.
In summary, regional anesthesia accounts for approximately one-fifth of professional liability claims. Most of the injuries from regional anesthesia claims are temporary, and approximately one-half of the temporary claims are associated with obstetrics. High severity injuries continue to result from neuraxial cardiac arrest and neuraxial hematomas associated with coagulopathy. Heightened vigilance and prompt diagnosis and treatment may improve outcome in these cases.
Dr. Lee is an Assistant Professor in the Department of Anesthesiology at the University of Washington, Seattle, WA.
References
- Rodgers A, Walker N, Schug S, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ 2000;321:1493.
- Wulf H, Biscoping J, Beland B, et al. Ropivacaine epidural anesthesia and analgesia versus general anesthesia and intravenous patient-controlled analgesia with morphine in the perioperative management of hip replacement. Ropivacaine Hip Replacement Multicenter Study Group. Anesth Analg 1999;89:111-6.
- Auroy Y, Narchi P, Messiah A, et al. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology 1997;87:479-86.
- Auroy Y, Benhamou D, Bargues L, et al. Major complications of regional anesthesia in France: The SOS Regional Anesthesia Hotline Service. Anesthesiology 2002;97:1274-80.
- Lee LA, Posner KL, Domino KB, et al. Injuries associated with regional anesthesia in the 1980s and 1990s: A Closed Claims Analysis. Anesthesiology (in press).


 Issue PDF
Issue PDF