Central venous catheterization is a common procedure with more than 5 million central venous catheters (CVC) implanted each year in the United States.1,2 Approximately 8% of hospitalized patients require central venous access during the course of their hospital stay.2
Appropriate selection of cannulation site depends on the indication, short vs. long-term requirements, as well as the associated risks. Site of cannulation is also dependent on convenience, ease of access, as well as patient anatomy and comfort. Common sites for insertion include the internal jugular, subclavian/axillary, and femoral veins. While previous research has demonstrated that risks of mechanical complications between jugular and subclavian sites of insertion are approximately equal,2-7 some suggest that insertion at the subclavian site may be associated with a lower risk of infection and thrombosis compared to the internal jugular site.5
Studies have shown that employing ultrasound (US) guidance among those who are experienced in its proper use for central vein catheterization can reduce the rate of failed punctures, complications, as well as performance time.5,7-9 Evidence to support US-guidance when inserting through the internal jugular vein includes several meta-analyses and recent clinical practice guidelines; however, a comprehensive review for subclavian vein insertion has not been performed. Thus, our group conducted a systematic review and meta-analysis of randomized controlled trials to determine the safety and efficacy of US-guided subclavian vein catheterization compared to the traditional “blind” landmark method.10 The following highlights our recently published systematic review and describes the technique of US- guided vein catheterization.
Summary of Our Recent Work
A search of Medline, EMBASE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and CINAHL (to September 2014) was conducted.10 We included all randomized control trials comparing US to the landmark technique for subclavian catheterization in adult populations. Since there are variations in the US technology used across specialties, sonographic Doppler or two-dimensional (2D) US imaging, as well as dynamic and static use of US were considered in our study. Outcomes of interest included safety and failure of catheterization.
Ten out of 601 studies met inclusion for review (N=2,168 study participants). We found that overall complication rates were reduced with US compared to the landmark group (odds ratio, 0.53; 95% CI, 0.41-0.69). Other subgroup analyses suggested that dynamic 2D US decreased inadvertent arterial puncture, pneumothorax, and hematoma formation. These adverse events, although uncommon, are clinically significant and potentially life-threatening. Use of routine US may prevent misadventures of the needle that lead to these complications.10
Our analysis also suggested that the use of dynamic 2D US significantly reduced failed catheterization rates when compared to the landmark technique (risk ratio, 0.24; 95% CI, 0.06-0.92). A review by the Cochrane group (investigating US use for femoral and subclavian line insertion) also suggested benefits of US use; however, this publication did not include more recent studies identified in our study.11 In summary, significant decreases in both failed catheterizations and adverse events are associated with dynamic 2D US-guidance. These results should still be interpreted with caution as the included studies had wide variation with regards to the patient populations, clinical settings, operator experience, as well as details of the US technique. Despite these limitations, significant decreases in both failed catheterizations and adverse events are associated with dynamic 2D US-guidance. Our group’s recommendations on how to perform US-guided subclavian vein cannulation are reviewed below.10
US-Guide Subclavian Vein Catheterization Technique
The subclavian vein and artery are found at the junction of the intrathoracic cavity and the extrathoracic zone (Figure 1). The subclavian vein extends from the axillary vein as it passes above the first rib and under the subclavius muscle and the clavicle. Depending on the patient’s size, adipose tissue and muscle structure, the subclavian vein is situated approximately 1–4 cm deep below the skin and easily identified by US.
In order to image the axillary and subclavian veins, the supine patient is placed in Trendelenburg (5–10°), to promote venous drainage towards the upper thorax and increase the axillary vein diameter, and potentially decrease the risk of entrainment of air. We recommend beginning imaging in short axis, in order to display the vessels transversely, and placing the probe at the distal clavicle where the axillary artery and vein are the largest and most superficial (Figure 2). The axillary artery can be identified by pulsations, while the vein will collapse under the probe’s pressure or with deep inspiration. Another way to confirm the location of the axillary vein is to use color or pulsed wave Doppler. This is most effective in the long axis view achieved by rotating the probe 90° (Figure 3).
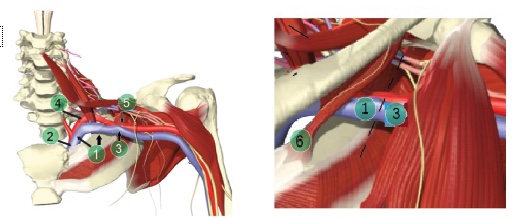
1. Subclavian vein 2. Brachiocephalic vein 3. Axillary vein 4. Subclavian artery 5. Axillary artery 6. Subclavius muscle
Figure 1.
Subclavian and axillary vein/artery anatomy. The subclavian artery (SCA) and subclavian vein (SCV) borders are at the lateral edge of the first rib, and not specifically to the clavicle (although this is easier to remember). The third part of the SCA continues as the axillary artery and the axillary vein becomes the SCV at the lateral border. The third portion of the subclavian artery runs downward and lateral from the lateral margin of the scalenus anterior to the outer border of the first rib, where it becomes the axillary artery. (Gray’s Anatomy: The Anatomical Basis of Clinical Practice [40th ed.], Churchill-Livingstone, Elsevier, 2008, ISBN 978-0-443-06684-9.) & (With permission of Denault et al. Basic Transesophageal and Critical Care Ultrasound 1st Edition, CRC Press Taylor & Francis Group 2016; Anatomical images with permission of Primal Pictures, Wolters Kluwer Health.)
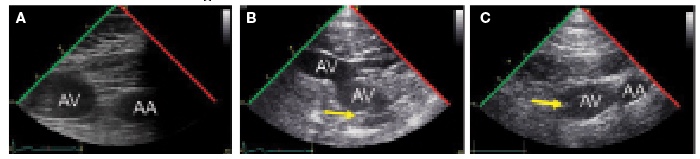
Figure 2. Ultrasound of axillary vasculature. (A–C) Ultrasound examination in a transverse plane of the subclavian vein (SCV), axillary vein (AV) and axillary artery (AA) from (A) under the clavicle, (B) mid-clavicular and (C) distal positions. Air bubbles (arrow) are often seen in patients with an ipsilateral peripheral venous catheter. (With permission of Denault et al. Basic Transesophageal and Critical Care Ultrasound 1st Edition, CRC Press Taylor & Francis Group 2016; Anatomical images with permission of Primal Pictures, Wolters Kluwer Health.)

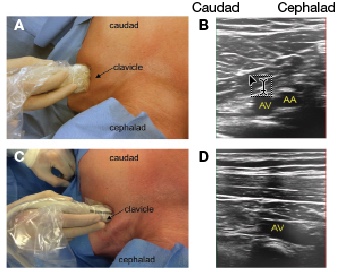
Figure 3. Axillary vein. (A, B) Transverse and (C, D) longitudinal position of the ultrasound probe with imaging of the left axillary vein (AV) and the left axillary artery (AA). (With permission of Dena ul t et al. Basic Transesophageal and Critical Care Ultrasound 1st Edition, CRC Press Taylor & Francis Group 2016.)
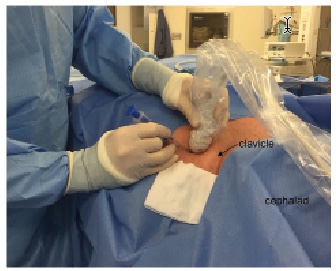
Figure 4. Positioning of operator, probe, and needle.
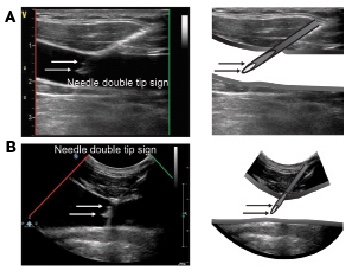
Figure 5. Double tip sign. Ultrasound images of the needle in a long axis view with the double tip sign are shown using (A) linear and (B) curvilinear microconvex probes. (With permission of Denault et al. Basic Transesophageal and Critical Care Ultrasound 1st Edition, CRC Press Taylor & Francis Group 2016.)
The ideal spot to puncture the vein is approximately located at a third of the distance between the clavicle and axilla (at this location the vein being cannulated is anatomically speaking the axillary vein, Figure 4). In a patient who is awake, local anesthesia is administered by inclining the needle 45° towards the probe’s center with a short axis view. Tilt the probe to the patient’s head once the needle has penetrated a few centimeters of subcutaneous tissue to visualize the luminescent tip, or the needle’s shaft, which will produce a characteristic “double echo” sign (Figure 5).
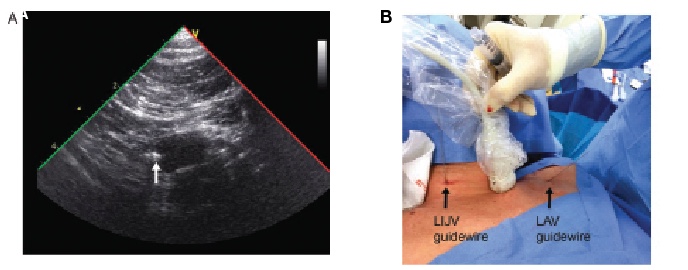
Figure 6. Axilary vein guidewire. (A) Guidewire coming from the left axillary vein (LAV) (arrow) (B) In order to see the guidewire the ultrasound probe can be positioned above the LAV or along the left internal jugular vein (LIJV) just above the left clavicle. (With permission of Denault et al. Basic Transesophageal and Critical Care Ultrasound 1st Edition, CRC Press Taylor & Francis Group 2016.)
After confirming the needle is aligned towards the center of the vein, continue introducing the needle (with continuous aspiration applied to the syringe), until the needle is seen penetrating the vein and blood enters the syringe. At this point, the US probe can be put aside and, with the needle held in place, the guidewire can be advanced into the vessel (Figure 6). Confirm that the guidewire is in the axillary vein prior to dilation and catheter insertion. If the guidewire is not well seen, examine the adjacent internal jugular vein to exclude malposition of the guidewire in the internal jugular vein. Another location for misplacement of the guidewire is in the ipsilateral innominate vein, and can be excluded by moving the US beam downwards to the clavicle to visualize this vessel.
In summary, given the proposed benefits of dynamic US use, we would encourage practitioners to review and adopt this technique when cannulating the subclavian vein.
References
- McGee DC, Gould MK. Preventing complications of central venous catheterization N Engl J Med 2003; 348: 1123-1133.
- Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med 1994; 331:1735-1738.
- Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med 1996; 24:2053-2058.
- Ruesch S, Walder B, Tramer MR. Complications of central venous catheters: internal jugular versus subclavian access–a systematic review. Crit Care Med 2002; 30:454-460.
- Parienti JJ, Mongardon N, Megarbane B, et al, and the 3 SITES Study Group. Intravascular complications of central venous catheterization by insertion site. N Engl J Med 2015; 373:1220-1229.
- Marik PE, Flemmer M, Harrison W, et al. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: a systematic review of the literature and meta-analysis. Crit Care Med 2012; 40: 2479-2485.
- Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A. The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation. Health Technol Assess 2003; 7:1-84.
- Hind D, Calvert N, McWilliams R, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ 2003; 327:361
- Kaye AD, Fox CJ, Hymel BJ, et al. The Importance of Training for Ultrasound Guidance in Central Vein Catheterization. MEJ Anesthesiol 2011; 21: 61-66.
- Lalu MM, Fayad A, Ahmed O, et al. Canadian Perioperative Anesthesia Clinical Trials Group. The importance of training for ultrasound guidance in central vein catheterization. Crit Care Med 2015; 43:1498-1507.
- Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev 2015; 1:CD011447.
Carly C Barron is a faculty member in medicine at the University of Ottawa. Andre Denault is a faculty member in the Department of Cardiac Anesthesiology, Montreal Heart Institute, Division of Critical Care of the Department of Medicine, Centre Hospitalier de l’Université de Montréal and is supported by institutional departmental funds.
Manoj Lalu is a Post-Doctoral Fellow in the Department of Anesthesiology, The Ottawa Hospital, Regenerative Medicine Program, The Ottawa Hospital Research Institute and is supported by the Heart and Stroke Foundation of Canada.
Sources of Funding and Conflicts of Interest: The authors have no conflicts of interests to declare.


 Issue PDF
Issue PDF