As a complement to the article by Kadis and Loskove in the Fall 2012 ASPF Newsletter,1 we wish to expand the clinician’s attention from the intubation of the difficult airway to the critical time of the difficult airway extubation. This is an area of patient safety that has not been addressed sufficiently in our opinion. We would like to contribute our systematic approach.
The Patient
The following case scenario was abstracted from actual patients and events that may not be unique to any one institution and serves as an illustration of the problem discussed in this report.
A 60-year-old woman presented with ischemic heart disease for emergent coronary artery bypass surgery. Following easy mask ventilation, experienced anesthesia providers were unable to intubate the patient in the operating room using standard laryngoscopy. The airway was secured with a videolaryngoscopic device and use of a bougie. After surgery, she was transported intubated to the ICU per the cardiac surgical postoperative protocol. A sign identifying her difficult airway was placed above her bed per the anesthesiology department’s airway protocol for such instances. At the transfer of care to ICU team, the anesthesiologist mentioned the need to contact the anesthesiology service at the time of anticipated extubation. On postoperative day #3, she met extubation criteria and was on minimal vasopressor support. She was extubated, but developed significant respiratory distress followed shortly thereafter by cardiac arrest. The anesthesiology team responded immediately to the overhead page at the time of the code. During CPR, she could not be intubated, and the surgical airway remained a futile effort. The ICU team caring for the patient did not consult with the anesthesiology team prior to extubation on the specifics of her airway management.
The Problems
1. The assessment of risks/benefits of extubation appeared to be limited immediately prior to the event.
2. Advanced airway devices are usually not immediately available in an ICU unless specifically requested.
3. Emergency intubating conditions are often suboptimal especially during CPR.
4. Despite difficult airway identification, no additional steps were taken to prepare for potential respiratory failure after extubation.
5. Following transfer of care from the anesthesia team to a non-anesthesiology ICU team creates a high risk for loss of critical information/preparation needed at a later stage of care, in this case at the time of extubation.
Background

Figure 1. Difficult Airway Extubation ETT Sticker Identification.
In 1993 the American Society of Anesthesi-ologists published a difficult airway algorithm that recommended a nonsurgical device (LMA, jet ventilation, or combitube) as a trial in the “cannot intubate-cannot ventilate” scenario.2 A closed claims analysis comparing years 1985-1992 and 1993-1999 following publication of these guidelines showed a decrease in claims involving death or brain damage during induction of anesthesia. However, no similar observations could be made for airway claims relating to maintenance, extubation, or recovery from anesthesia.3 In addition, 100% of claims originating outside of the perioperative location involved death or brain damage.2 No information is available specifically addressing the re-intubation of the difficult airway in out-side of OR locations. In fact, in many hospitals, anesthesiology teams are part of first responders to code situations and airway management challenges for surgical and non-surgical patients alike. In these circumstances we are the first ones to identify and deal with a difficult airway. It remains our responsibility to establish a functioning mechanism to follow up with such patients that subsequently will leave our purview, to be cared for by non-anesthesiology teams in surgical and medical ICU’s or step down units. Extubation is a time when airway complications can occur, and resources and expertise in ICUs may be inadequate for dealing with acute respiratory failure of a patient with known difficult airway.
Literature regarding difficult intubations is plentiful, but evidence and recommendations on tracheal extubation have been a relatively neglected area of focus.4 Identification of a difficult airway by ID bracelet and/or inclusion with the allergy list has been useful for tracking patients throughout their hospital stay and improving safety.1 However, as evidenced by the case above, simple identification of a difficult airway patient may not prevent poor outcomes at the time of extubation. Recently the Difficult Airway Society (DAS) has published guidelines for the management of extubation.4 These guidelines codify an “at risk” extubation as one with a known difficult airway at intubation, an airway that may have deteriorated because of surgery, or where flexion-extension is now limited (application of halo or cervical spine fixation).4 It is recommended that practitioners should proceed through a 4-step algorithm: 1) plan to extubate, 2) prepare to extubate, 3) perform extubation, and 4) provide post extubation care.4 A specific requirement to consult with airway specialists prior to intended extubation to capitalize on their expertise remains unaddressed.
Preparation for any extubation should involve medical optimization of the patient to ensure success. This includes achieving cardiopulmonary stability as well as correcting metabolic derangements, normalizing temperature, and ensuring proper neuromuscular function.4 Coordination of appropriate resources and consultations is also necessary, particularly in the known difficult airway scenario: 1) choosing location of extubation (ICU versus operating suite), 2) ensuring proper equipment availability (cricothyroidotomy kit, video laryngoscopy, fiberoptic bronchoscopy, intubating laryngeal mask airways, airway exchange catheter) and 3) ensuring appropriate staff are available (anesthesia provider-otolaryngologist).
The Solution
The clinical practice committee in the department of anesthesiology developed a pathway for extubation of patients with a difficult airway identified by anesthesia providers after these intubated patients leave the immediate purview of the anesthesiology service. The committee determined that because the patients frequently were transferred to ICUs or were intubated in offsite locations with an ICU destination determined later (cardiology catheterization laboratory, electrophysiology, CT, MRI, interventional radiology, etc.), a hospital-wide policy rather than departmental policy would be needed, and it should be applicable to adults and pediatric patients alike. Goals of the policy were to improve awareness of patients that had an “at risk” extubation, secure pre-extubation consultation with the anesthesiology service, allow for full preparedness before extubation, and accomplish safe reintubation if needed in a setting of post-extubation respiratory failure.
Difficult Airway Extubation Policy
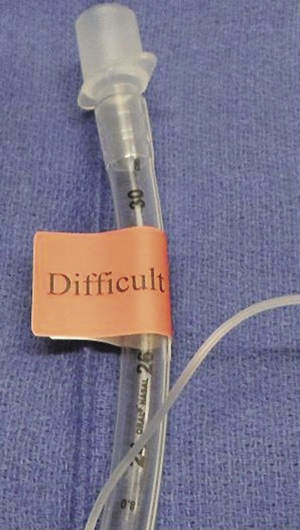
Figure 2. Difficult Airway Red Sticker Placed on ETT.
Part 1: Identification and Communication of At Risk Extubation
After identification of a difficult airway patient who remains intubated, the anesthesia care team 1) places red stickers [Figure 1] on the endotracheal tube [Figure 2], 2) completes a bedside 8½ × 11 inch sign [Figure 3] to be placed above the patient’s bed, and 3) places a red note in the progress notes section of the patient’s chart [Figure 4], or an equivalent flag in the electronic record system. The anesthesia care team must complete all paperwork before leaving the operating room or immediately following intubation in an offsite location. Stickers and a copy of the policy are placed in all emergency code bags. Lastly the policy also requires that a physician-to-physician sign out of the case and difficult airway specifics occur.
Part 2: Planning and Preparing for Extubation Prior to the intended extubation, the policy requires that the anesthesiology department must be contacted to evaluate the patient. In addition, the patient must then be extubated in the presence of an anesthesiology member, intensivist with airway expertise, neonatologist, or pediatric otolaryngologist (the latter two being age specific). This check before intended extubation allows for proper preparation for difficult airway management. If airway difficulty or ability to oxygenate is tenuous, elective extubation in the operating room can be arranged with proper equipment and surgical teams in place.
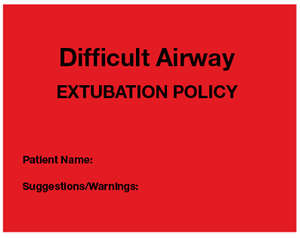
Figure 3. 8-1/2 × 11 inch sign with description of airway placed at head of bed.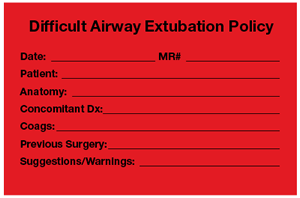 Figure 4. Difficult Airway Documentation in Progress Notes.
Figure 4. Difficult Airway Documentation in Progress Notes.


 Issue PDF
Issue PDF