Episode #61: Anesthesia Patient Safety Triple Threat
September 7, 2021Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
This is the part 2 of our mini-series on high-flow nasal oxygen. We continue our review of the article, “Safe Use of High-Flow Nasal Oxygen With Special Reference to Difficult Airway Management and Fire Risk” by Cooper, Griffiths, and Ehrenwerth from the October 2018 APSF Newsletter. You can check out the article here: https://www.apsf.org/article/safe-use-of-high-flow-nasal-oxygen-hfno-with-special-reference-to-difficult-airway-management-and-fire-risk/
Today, we review clinical scenarios when high-flow nasal oxygen may be used including pre-oxygenation prior to induction of general anesthesia, continued oxygen delivery and CO2 removal during intubation, improved oxygenation during awake fiberoptic or videoscopic intubation, and providing respiratory support following extubation.
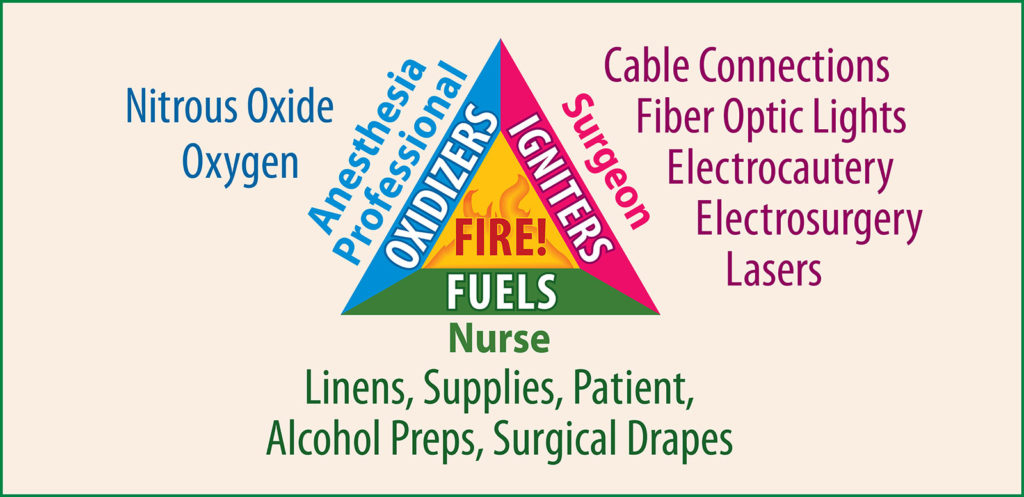
We must stay vigilant to prevent OR fires and it is important to be aware of the components of the fire triad.
Check out this case report on a brief ignition in the operating room while using high-flow nasal oxygen: Onwochei D, El-Boghdadly K, Oakley R, et al. Intra-oral ignition of monopolar diathermy during transnasal humidified rapid-insufflation ventilatory exchange (THRIVE). Anaesthesia 2017;72:781–783.
Finally, we review upcoming Anesthesia patient safety events and educational opportunities. Check out the calendar here and save the dates. https://www.apsf.org/events/category/conferences-events/
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be apart of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
© 2021, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel and I am your host. Thank you for joining us for another show. Last week, we talked about one of the most popular articles from the APSF website but there is more to the article which highlights several threats to patient safety that anesthesia professionals need to watch out for. It is an anesthesia patient safety triple threat that includes difficult airway management, operating room fire risk, and oxygen delivery to avoid hypoxemia. The article offers practical considerations to help keep patients safe from these threats as well. So, get ready!
Before we dive into the episode today, we’d like to recognize GE Healthcare, a major corporate supporter of APSF. GE Healthcare has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, GE Healthcare- we wouldn’t be able to do all that we do without you!”
Once again, this week, we will be discussing an article by authors, Cooper, Griffiths, and Ehrenwerth called “Safe Use of High-Flow Nasal Oxygen With Special Reference to Difficult Airway Management and Fire Risk” from the October 2018 APSF Newsletter. To follow along with us, head over to APSF.org and click on the Newsletter headings. Fifth one down is the Newsletter Archives. Then scroll down until you get to October 2018. Then, look over in the left-hand column and scroll down until you come to our featured article today. I will include a link in the show notes as well.
Last week, I read several quotes from one of the authors, Jeremy Cooper, an anesthesiologist who practices cardiothoracic anesthesia at Auckland City Hospital in New Zealand and we are so happy to have him contribute content from across the pond. We will be hearing more from him at the end of the show today too.
We will start with a rapid review of the contraindications before we discuss the clinical applications. Some relative contraindications may include: Partial nasal obstruction, disruption of the airway, laser or electrocautery close to the high flow delivery, contagious pulmonary infections with may include tuberculosis and Covid-19, nasal infection, contraindications to high concentrations of oxygen, patients younger than 16 years old, and patients who cannot tolerate hypercarbia from prolonged periods of apnea.
The absolute contraindications include: use of high flow nasal oxygen when alcohol-based skin preparation solutions are used, patients with a communication between the nasal and intracranial space, significant pneumothorax without a chest tube in place, complete nasal obstruction, active epistaxis or recent functional endoscopic sinus surgery.
Now, that when we know when we may not be able to use high flow nasal oxygen, let’s talk about when we may want to use this technology. The clinical scenarios include pre-oxygenation prior to induction of general anesthesia, continued oxygen delivery and CO2 removal during intubation, improved oxygenation during awake fiberoptic or videoscopic intubation, and providing respiratory support following extubation. We are going to take a closer look at each of these clinical applications.
First, high flow nasal oxygen delivery may be used to improve pre-oxygenation instead of a fitted face mask with 100% oxygen from the anesthesia breathing circuit. The benefits of using high flow nasal oxygen delivery is that you don’t need to use the facemask while at the same time delivering CPAP with decreased pulmonary shunting. Finally, you don’t need to remove the high-flow nasal oxygen cannula during intubation so you can continue to provide adequate oxygenation, but more on that very shortly.
The second clinical application involves the use of high-flow nasal oxygen delivery during intubation which can provide apneic oxygenation and increase the time until desaturation occurs. You may want to consider using high flow during your next rapid sequence intubation or difficult intubation. That way even when mask ventilation is not used prior to intubation, the patient can still receive adequate oxygenation with limited CO2 accumulation, during the first 20 minutes in particular. Keep in mind that there is no volatile anesthesia delivery with the high-flow system and it may be necessary to give supplemental IV anesthesia during a prolonged intubation attempt. Also, after the first 20 minutes or so, CO2 may accumulate and ventilation to remove CO2 may be necessary.
The third scenario for high-flow use is to provide oxygenation during an awake oral or nasal fiberoptic or videoscopic intubation. Being able to deliver oxygen and provide CPAP while performing an awake fiberoptic oral intubation can help to prevent desaturation. The authors point out that the benefits of CPAP from high flow nasal oxygen are continued even when the mouth is open during intubation, but to a lesser degree than when the mouth is closed. Patients with partial airway obstruction who require awake intubation may be good candidates for high-flow nasal oxygen during the intubation since this can reduce the work of breathing and decrease airway resistance. If you need to perform an awake nasal fiberoptic intubation, then you may be able to continue to use the high-flow nasal cannula during topical preparation, but you will need to move the nasal cannula on the intubation side during the attempt.
The next clinical scenario takes place after extubation for patients who need additional respiratory support in order to avoid re-intubation. Remember, high-flow nasal oxygen can delivery CPAP at 3-4cm H2O when the mouth is open as well as a high concentration of oxygen. This also allows patients the ability to talk during this treatment. Keep in mind, that not all nasal cannulas are the same and healthcare professionals or patients may just remove the nasal cannula, thinking that it is just a low-flow nasal cannula, and the patient may develop hypoxemia and respiratory failure.
Now, what if we head back into the operating room and consider using the high-flow nasal oxygen delivery to improve oxygenation, decrease work of breathing and increase CO2 elimination during surgery when patients are sedated or receiving IV anesthesia while breathing spontaneously. This set-up may be especially useful for procedures ear the larynx, face, and neck. You may want to consider using high-flow nasal oxygen the next time you take care of a patient undergoing a tracheostomy procedure for example.
Let’s take a closer look at a few more clinical scenarios when high-flow nasal oxygen may be used and how we can help to keep patients safe during these cases. The use of high-flow nasal oxygen requires a careful risk-benefit analysis prior to use. So, here we go.
What is the risk of fire when using high-flow nasal oxygen under the surgical drapes? Remember, the high flow is capable of delivering a much higher concentration of oxygen which can serve as an oxidizer. There is a ready fuel source in the drapes and swabs in the surgical field. The ignition source is close by too if there is a laser or electrocautery or “Bovie” used during the surgery. It is important to consider duration of HFNO use, adhesion of drapes to create barriers to O2 flow, flow rate, FiO2 of HFNO, and OR room air exchange rates. By careful evaluation of the components of the fire triad, the oxidizer, fuel, and ignition source, it is possible to reduce the risk of fire. For example, the high-flow nasal oxygen system can be used with an air/oxygen blender to decrease the FiO2 delivered and decrease the risk of fire while still providing the benefit of CPAP to the patient.
Patients with a severe partial airway obstruction may require an emergent awake tracheostomy. These patients are at risk for loss of airway and hypoxia. One technique for the management of these patients during the procedure is to use high-flow nasal oxygen with careful IV sedation if appropriate. The benefits include improved oxygenation with prolonged time to desaturation and decreased work of breathing. Plus, patients may be more cooperative. This must be balanced against the risk of airway fire which may be increased depending on the FiO2 used with the high-flow.
What about patients presenting to the OR for elective airway surgery? Can high-flow nasal oxygen be used for these procedures? Yes! There may be a role for high-flow in cases such as microlaryngoscopy, when IV sedation or TIVA is used and patients are able to maintain spontaneous ventilation. Patients may require intermittent bag mask ventilation if there are prolonged periods of apnea while using the high-flow in order to avoid significant hypercarbia. Patients may benefit from improved oxygenation which can occur even when there are prolonged periods of apnea, decreased work of breathing, and some CO2 washout especially in the first 20 minutes or so. The risks in this case include increased risk of fire especially when lasers and electrocautery are used. Another technique that is used for airway management during microlaryngoscopy is intermittent jet ventilation. Jet ventilators may have a safety feature to reduce the FiO2 and decrease the fire risk. In addition, during jet ventilation, room air is entrained leading to a decreased FiO2 as well. Many high-flow systems are designed to deliver only 100% oxygen and may include written warnings to not use these high-flow nasal oxygen devices in close proximity to any ignition source which includes electrosurgery, electrocautery, and lasers. There is a case report of an OR fire when a high-flow nasal oxygen system was used during a hard palate biopsy procedure leading to a brief ignition and subsequent burn on the monopolar instrument. The monopolar was immediately removed and there were no patient or staff burns. The case was able to be completed by turning off the high-flow anytime the electrocautery was used. I will include a link to the case report in the show notes as well.
The authors provide some general considerations for high-flow nasal oxygen use. Let’s review them now.
- More research and reporting is needed for high-flow nasal oxygen fires. This will help to determine the difference in accidental flash flames and spreading flames. Spreading flames are responsible for more burn damage. We also need more information about ignition frequency with cases performed using alternative ventilation techniques in order to compare the fire risk during similar procedures with high-flow nasal oxygen.
- One way to help decrease the fire risk is to use high-flow with an oxygen/air blender to reduce the FiO2, but still deliver some of the benefits.
- There are case reports of fire with the use of High-flow nasal oxygen and we must remain vigilant to decrease the risk.
- Further evaluation of the oxygen pollution around the head and neck area from the high flow nasal oxygen. Remember when the oxygen concentration is greater than 30% around the head and neck there may be an increased risk for fire and there is an even higher risk when the actual procedure is occurring on the head and neck as well.
What does the future hold for high-flow nasal oxygen? In 2018, the authors predicted that this technology would be used by more anesthesia professionals in the operating room. One obstacle to this use is bringing the device into the operating room and assembling it when needed. If the high-flow device could be connected directly to the anesthesia workstation in the future, this would facilitate use in the OR during surgery and anesthesia and may be something that is available on future anesthesia machines.
This was an excellent review of high-flow nasal oxygen delivery with the benefits of improved oxygenation, reduced work of breathing, delivery of CPAP, and some CO2 removal which must be balanced by the risk of airway fire. It’s use must include weighing the risks and benefits and reviewing the relative and absolute contraindications in order to help keep patients safe.
Before we wrap up the show for today, I asked Cooper what’s next for his research and projects. Here is what he wrote in: “For myself …I am leading a NZ project to make everyone follow the ASA guidelines about how to safely insert central venous lines, published in January 2020. It’s a careful project and will take time, but dilation of major arterial vessels still happens unfortunately. And I still work and teach the trainees and hope one day to visit the USA again.”
Thank you so much to Cooper for his contributions to the show today and we are looking forward to perhaps hearing more about your safe central line insertion project in the future.
If you have any questions or comments from today’s show, please email us at [email protected].
Visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. October is another big month for Patient Safety Panels and Educational Opportunities. You can check out the full listing at APSF.org and clicking on the Conferences and Events Heading. The October events are part of the American Society of Anesthesiologists Annual Meeting, Anesthesiology 2021. First up is the ASA/APSF Ellison C. Pierce Jr. MD Patient Safety Memorial Lecture, “Anesthesia Safety in an Asymmetrical World” given by Angela Enright and the APSF Panel called, “Clinician Safety: To Care is Human.” For more information about these events head over to the website and I will include a link in the show notes. If you are attending any of these events, be sure to share your experience on Twitter and tag us @APSForg. We can’t wait to hear from you!
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2021, The Anesthesia Patient Safety Foundation