Episode #229 Revolutionizing Anesthesia Care for Cardiac Patients: Shorter and Safer Dual Antiplatelet Therapy with Next-Gen Stents
November 20, 2024Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
Our featured article from the October 2024 APSF Newsletter is “New Drug-Eluting Cardiac Stents and Dual Antiplatelet Therapy: How Short is Too Short?” by Janak Chandrasoma, Abigail Song, Joseph Szokol, and Antreas Hindoyan. This article has it all, history, a literature review, and guidelines.
Thank you to Janak Chandrasoma for contributing to the show today.
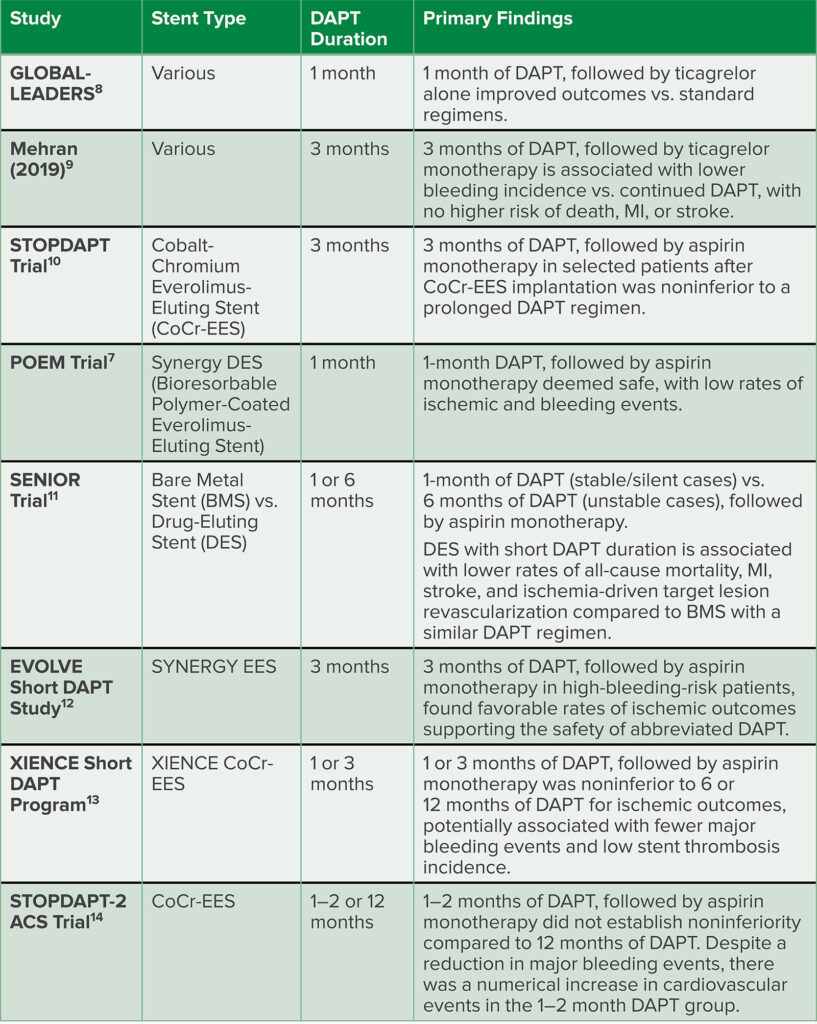
Check out Table 2 in the article for a review of the literature for shorter duration DAPT and the newer DES. The data to support the newer stents reveals the following:
- Lower rates of ischemia
- Shorter duration of DAPT which decreases the bleeding risk
- Comparable to bare metal stents in terms of all-cause mortality, myocardial infarction, stroke, and ischemia-driven target lesion revascularization.
Table 2: Summary of Recent Studies Examining Abbreviated DAPT Regimens.
Subscribe to our YouTube Channel here: https://www.youtube.com/@AnesthesiaPatientSafety
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2024, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. Last week, we asked the question, “How long do patients need to continue dual-antiplatelet therapy following placement of a drug eluting stent?” We will go into more detail today, but the short answer is that newer generation drug-eluting stents have decreased rates of in-stent thrombosis permitting shorter duration of dual antiplatelet therapy. According to the American College of Cardiology and the American Heart Association a shortened duration of dual-antiplatelet therapy of 1-3 months is reasonable. According to the European Society of Cardiology, in patients with high risk of bleeding, you may consider discontinuation of P2Y 12 receptor inhibitor therapy after 3 months. Don’t turn that dial because we have more to discuss when it comes to keeping patients with drug eluting stents safe during anesthesia care.
Before we dive into the episode today, we’d like to recognize BD, a major corporate supporter of APSF. BD has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, BD – we wouldn’t be able to do all that we do without you!”
Our featured article again today is from the October 2024 APSF Newsletter. It is “New Drug-Eluting Cardiac Stents and Dual Antiplatelet Therapy: How Short is Too Short?” by Janak Chandrasoma, Abigail Song, Joseph Szokol, and Antreas Hindoyan. To follow along with us, head over to APSF.org and click on the Newsletter heading. First one down is the current issue, October 2024. Then, scroll down until you get to our featured article today. I will include a link in the show notes as well.
Let’s do a quick review from last week and then return to the article. Plus, we have exclusive content from one of the authors.
Remember, the first-generation stents were made of a standard bare metallic stent and a coated polymer mixed with an anti-restenotic drug such as sirolimus or paclitaxel. Newer-generation drug-eluting stents include biodegradable polymer stents or bioresorbable scaffolds. These have a lower rate of in-stent thrombosis and may need a shorter duration of dual antiplatelet therapy without compromising patient safety.
An important consideration with every type of cardiac stent when deciding on the optimal duration of dual antiplatelet therapy is balancing the risks. On one hand, there is the risk of in-stent thrombosis and on the other, there is the risk of bleeding complications. Last week, we talked about how to determine which patients are high risk using the PRECISE-DAPT Score or the ARC-HBR Criteria which includes major and minor criteria. To calculate the PRECISE-DAPT score, you can head over to precisedaptscore.com and use their web calculator. There, you will need to input the hemoglobin level, age, white blood cell count, creatinine clearance, and if there was a prior bleeding event to get the patient’s score and their calculated bleeding risk. Check out the link in the show notes.
The authors highlight criteria for High Bleeding Risk in Table 1 in the article. We are going to go through it now. High Bleeding Risk is defined as the presence of at least one of the following:
- Age greater than or equal to 75 years old
- Oral anticoagulation planned to continue after PCI
- Anemia with a hemoglobin of less than 11g/dL
- Transfusion within the past 4 weeks
- Platelet count < 100,000/ml
- Hospital admission for bleeding within the past 12 months
- Stroke within the previous 12 months
- History of intracerebral hemorrhage
- Severe chronic liver disease
- Chronic kidney disease defined as creatinine clearance <40mL/min
- Cancer within the previous 3 years
- Planned major, noncardiac surgery in the next 12 months
- Glucocorticoids or NSAIDS planned for more than 30 days after PCI
- And expected non-adherence to greater than 30 days of DAPT.
And now, it’s time to get back into the article, right where we left off. These are evidence-based recommendations that we are talking about and there is a lot of newer evidence to support the safety and efficacy of a shorter duration of dual antiplatelet therapy. Patients who are at high bleeding risk are good candidates for these newer stents. The data to support the newer stents reveals the following:
- Lower rates of ischemia
- Shorter duration of DAPT which decreases the bleeding risk
- Comparable to bare metal stents in terms of all-cause mortality, myocardial infarction, stroke, and ischemia-driven target lesion revascularization.
Let’s take a closer look at Table 2 and some of the evidence. This is going to a fast and furious literature review!!
First, the global-leaders study evaluated various stent types with 1 month DAPT therapy. The primary findings were that 1 month of DAPT followed by Ticagrelor alone improved outcomes versus standard regimens.
The 2019 Study by Mehran evaluated various stents with 3 months DAPT and found that 3 months DAPT, followed by ticagrelor monotherapy is associated with lower bleeding incidence compared to continued DAPT with no higher risk of death, MI, or stroke.
The STOPDAPT Trial evaluated the cobalt-chromium everolimus eluting stent with 3 months of DAPT. The results were that 3 months DAPT followed by aspirin along in selected patients was non-inferior to prolonged DAPT.
The Poem Trial evaluated the synergy DES, a bioresorbable polymer-coated everolimus eluting stent with 1 month DAPT and found that 1 month DAPT followed by aspirin along was safe with low rates of bleeding and ischemic events.
The SENIOR trial compared bare metal stents and drug-eluting stents with 1 month of DAPT in stable or silent cases compared to 6 months DAPT in unstable cases followed by aspirin monotherapy. The results were that DES with short DAPT duration is associated with lower rates of all-cause mortality, MI, stroke, and ischemia-driven target lesion revascularization compared to BMS with similar DAPT duration.
The EVOLVE Short DAPT Study looked at the Synergy DES with 3months of DAPT followed by aspirin monotherapy in high-bleeding-risk patients and found favorable rates of ischemic outcomes supporting the safety of shortened DAPT.
We have two more studies to go. The XIENCE Short DAPT Program studied the XIENCE DES with 1 or 3 months DAPT followed by aspirin alone was non-inferior to 6 or 12 months of DAPT for ischemic outcomes, potentially associated with fewer major bleeding events and low stent thrombosis incidence.
Finally, the STOPDAPT-2ACS Trial studied the cobalt chromium everolimus eluting stent and found that 1-2 months DAPT followed by aspirin alone did not establish non-inferiority compared to 12 months DAPT. There was a reduction in major bleeding events, but also a numerical increase in cardiovascular events in the 1-2 month DAPT Group. Whew!! What an exciting review of the new studies.
The studies highlighted in Table 2 include updated evidence that several societies have used to update their guidelines. First, the American College of Cardiology and The American Heart Association give a Class 2a or moderate recommendation for a shorter duration of DAPT. Select patients undergoing PCI may safely transition to P2Y12 Inhibitor monotherapy and discontinue aspirin after 1-3 months of DAPT where the benefits outweigh the risks.
The European Society of Cardiology guidelines are different. These guidelines highlight that following PCI for non-ST-segment elevation acute coronary syndrome, DAPT with a potent P2Y12 receptor inhibitor and aspirin is generally recommended for 12 months regardless of stent type unless contraindicated. There are specific clinical cases including high bleeding risk with a Precise-DAPT score greater than 25 or meeting the ARC-ABR criteria in which clinicians may consider a shorter duration for DAPT of less than 12 months. Clinicians may consider modifying the regimen depending on ischemic and bleeding risks, adverse events, comorbidities, concomitant medications, and drug availability. An important consideration is that for non-ST-segment elevation acute coronary syndrome patients with stent implantation who are at high bleeding risk, discontinuation of P2Y12 receptor inhibitor therapy after 3-6 months should be considered. In addition, in patients who are at very high bleeding risk, such as a bleeding event within the past 30 days or with an imminent nondeferrable surgery, a 1 month duration of therapy with aspirin and Clopidogrel may be considered.
Finally, the American College of Chest Physicians updated its recommendations in 2022 for duration of DAPT after drug-eluting stent placement. This is a conditional recommendation for patients scheduled for elective surgery who have had stent placement within the last 3-12 months and are on DAPT. If you work in a preoperative anesthesia clinic, then it is very likely that you have seen patients who fit this scenario. The updated recommendation is for the discontinuation of the P2Y12 inhibitor prior to surgery, based on indirect evidence and expert opinion suggesting the safety of stopping P2Y12 inhibitors in patients with stents implanted more than 3 months prior.
Check out Table 3 in the article for a quick reference guide for these updated guidelines.
We made it to the end of the article. The authors highlight that newer generation stent technology has led to less stent thrombosis. This has led cardiology experts to update the recommendations for the duration of DAPT on these new drug-eluting stents to 1-3 month courses of anticoagulation in patients with stable coronary artery disease. Bare metal stents have largely been replaced by these newer stents with their enhanced performance. A multi-disciplinary approach with the cardiologist, surgeon, and anesthesiologist is required to make clinical decisions regarding the duration of DAPT and urgent surgery and this may lead to a very short course of DAPT. There is a call to action for anesthesia professionals to be mindful of these shorter duration of DAPT and be aware that the duration for anticoagulation of as little as one month may be recommended for patients with recent stent placement based on the evidence of enhanced safety profile of these newer generation stents.
Before we wrap up for today, we are going to hear from another APSF article. Here he is now.
[Chandrasoma] “Hi, my name is Janak Chandrasoma, and I’m with the Department of Anesthesiology at the Keck Medical Center of USC.”
[Bechtel] I asked Chandrasoma what he hopes to see going forward. Let’s take a listen to what he had to say.
[Chandrasoma] “I work at the Preoperative Clinic at USC, and I’m really excited for this data to come out because For a long time, anaesthesiologists have just been in the dark with regards to how long you need to wait for dual antiplatelet therapy.
And I constantly have conversations with our anaesthesiologists where I tell them, you know, this six month thing, it’s totally out of date. So I’m hoping, really, that this changes practice for a lot of people. I’m really excited about it.”
[Bechtel] “Thank you so much to Chandrasoma for contributing to the show today. We are really excited to hear about this shortened duration of dual anti-platelet therapy. It will really help us in our preoperative anesthesia clinics for timing of surgery and decisions about dual anti-platelet therapy.
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
Thank you so much to all of our listeners. If you get a chance, we would love for you to give us a 5 star rating and leave us a review. This helps other people interested in anesthesia patient safety to find our show and become listeners too! You can also share this podcast with your anesthesia colleagues, members of your perioperative team, the surgeons that you work with, trainees, students, and more. We are looking forward to continuing to bring you the latest in anesthesia patient safety.
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2024, The Anesthesia Patient Safety Foundation