Episode #140 Combating Cognitive Bias in Anesthesiology
March 7, 2023Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
We are back for Part 2 of our series on cognitive bias in anesthesiology. This is a threat to anesthesia patient safety, so we need the tools to be able to recognize cognitive bias when it occurs, acknowledge the implications for patient safety, and work to reduce the impact of cognitive bias when we provide anesthesia care. Our featured article today is “Recognizing and Combating Cognitive Bias in Anesthesiology: Implications for Patient Safety” by George Tewfik, Stephen Rivoli, and Monica Harbell from the February 2023 APSF Newsletter.
Have you heard of the “bias blind spot?” This is a phenomenon that occurs when a person experiences a false sense of being invulnerable to cognitive bias. For more information, check out this article.
Stiegler MP, Tung A. Cognitive processes in anesthesiology decision making. Anesthesiology. 2014;120:204–217. PMID: 24212195
Check out Figure 1 in the article which reveals strategies that may enable medical professionals to combat bias, via prevention, recognition, and active interventions to mitigate their effect in a real-time basis.
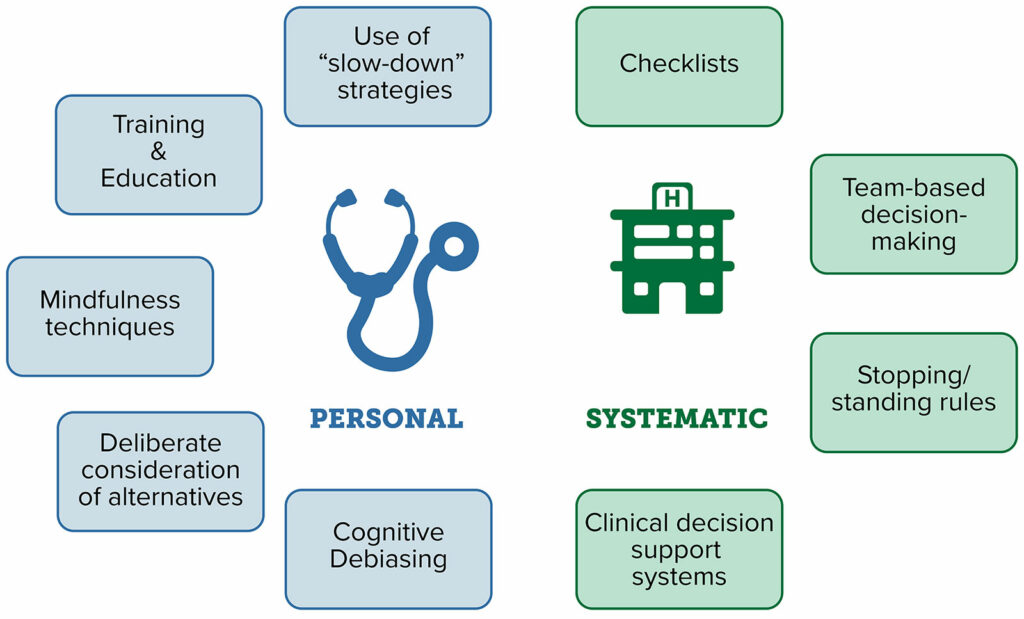
Figure 1: Strategies that may enable medical professionals to combat bias, via prevention, recognition, and active interventions to mitigate their effect in a real-time basis.
The deadline for the June 2023 APSF Newsletter is just two days away, March 10. So, what are you waiting for, get your submissions in. https://www.apsf.org/apsf-newsletter/guide-for-authors/
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2023, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. Last week, we cracked open the February 2023 APSF Newsletter to talk about cognitive bias in anesthesiology and its impact on anesthesia patient safety. If you haven’t listened to episode #139 yet, make sure that you check it out. Today, we are back for Part 2.
Before we dive into the episode today, we’d like to recognize Fresenius Kabi, a major corporate supporter of APSF. Fresenius Kabi has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Fresenius Kabi – we wouldn’t be able to do all that we do without you!”
Our featured article today is once again “Recognizing and Combating Cognitive Bias in Anesthesiology: Implications for Patient Safety” by George Tewfik, Stephen Rivoli, and Monica Harbell from the February 2023 APSF Newsletter. To follow along with us, head over to APSF.org and click on the Newsletter heading. First one down is the Current Issue. From here, scroll down until you get to our featured article today. I will include a link in the show notes as well.
Cognitive bias occurs in medicine when a healthcare professional creates a subjective reality which changes and affects their perception of a data point and then may alter their diagnosis and management going forward. This is a threat to patient safety and has been implicated in medical errors during the perioperative period. Let’s take a moment to review several types of cognitive bias that may occur during anesthesia care from Table 1 in the article.
- Anchoring Bias is the over-reliance on initial impressions and/or information with an inability to incorporate new data. This occurs when the operating room team fixates on bronchospasm as the cause of airway resistance instead of recognizing a kinked endotracheal tube.
- Ascertainment bias is a type of sampling error that occurs when the results found are not truly representative of the intended target and are influenced by the observer. When post-induction hypotension is thought to be due to the induction dose of anesthetic medications without recognizing an alternative diagnosis such as hypovolemia requiring IV fluid resuscitation.
- Availability bias involves making decisions based on the accessibility of data which occurs when the anesthesia professional taking care of a bleeding patient does not change the choice of blood products due to the length of time it takes to obtain lab results.
- Bandwagon Effect or Diagnostic Momentum involves the inability to consider alternatives once a diagnosis or determination has been made. This cognitive bias may occur for an individual or a team.
- Confirmation bias occurs when the anesthesia professional only observes or seeks information to confirm their own opinion instead of seeking additional data. Have you every repeatedly checked your patient’s the blood pressure, even changing the cuff size and location, in order to try to get a reassuring result, instead of recognizing that the patient is hypotensive, and it is not a device error?
- Framing Effect involves an impact on decision-making based on how information is presented, such as by a trusted source. This is an important one in anesthesiology since it may have a big impact on anesthesia trainees.
- Search Satisficing or Premature Closure involves failing to continue to seek data once something has been identified. This may occur during emergence, if the anesthesia professional accepts the belief that the patient is having delayed wakeup due to residual inhaled anesthetic instead of evaluating for another cause.
It’s time to get back into the article right where we left off last week. Now that we know how to recognize the different types of cognitive bias, we can talk about how to reduce cognitive bias and decrease medical errors. The authors describe several effective interventions for reducing cognitive bias. Let’s go through them.
- First up is improvement of knowledge and experience via tools such as simulation, feedback, and education.
- Another intervention is improvement of reasoning and decision-making skills using tools such as reflective practice and metacognitive review.
- The third intervention is improvement of assistance in decision-making with aids such as electronic health records and integrated decision support.
Are any of these interventions part of your practice already? The most important approach may be increasing awareness of these confounding factors through education of medical personnel. The type of education may include learning materials, scholarly publications, didactics, and simulation. Understanding the interaction between errors and cognitive bias is important. Fixation errors occur when the focus is maintained on only one aspect of a situation while ignoring the other areas that are more relevant. This type of error may occur due to anchoring bias. Increased awareness is a powerful tool to help reduce anchoring bias and fixation error with strategies such as ruling out the worst-case scenario, understanding that first assumptions may be wrong, consideration of artifacts as the last explanation of a problem, and avoiding use of a prior conclusion with current team members.
We can’t rely only on increased awareness though to fight cognitive bias. Have you ever thought that you could not be affected by cognitive bias? Have you heard of the “bias blind spot?” This is a phenomenon that occurs when a person experiences a false sense of being invulnerable to cognitive bias and this phenomenon occurs more often in providers with greater cognitive sophistication. For more information check out the 2014 article by Stiegler and Tung, “Cognitive processes in anesthesiology decision making.” I will include a link in the show notes as well.
Let’s look at the different strategies that may reduce cognitive bias including interventions directed at the clinician individually as well as systemic or system-wide ones. Check out Figure 1 in the article and we are going to review the strategies to reduce cognitive bias through prevention, recognition, and active interventions that you can implement in your clinical practice.
The personal strategies include the following:
- Use of slow-down strategies
- Training and education
- Mindfulness techniques
- Deliberate consideration of alternatives
- And Cognitive debiasing
Systematic strategies include the following:
- Checklists
- Team-based decision-making
- Stopping/Standing rules
- Clinical decision support systems
We have talked about many of these strategies on past shows as ways to help keep patients safe during anesthesia care. Checklists may be used for different clinical scenarios ranging from the preoperative evaluation to the time out to emergency treatment for malignant hyperthermia and local anesthetic systemic toxicity to help keep patients safe during anesthesia care and to help decrease risk of adverse events in the operating room. During studies in the simulated environment, the use of checklists results in a 6-fold reduction in management errors during crisis management. This significant reduction occurs even after adjusting for learning or fatigue effects. The use of clinical decision support systems is another important consideration which may involve the use of integrated prompts in electronic health records. This may be something as simple as a reminder that pops up when it is time to re-dose an antibiotic during a long surgical procedure or a red flag for critical lab values.
We need to continue to evaluate the effectiveness of these strategies. One of the biggest limitations is the lack of objective evidence to support the implementation and use of the following strategies:
- The Stopping and Standing Rules – this is a method that can help determine with information-gathering can stop.
- The “Must-Not-Miss Alternative” – for this method, the clinician evaluates diagnoses that must be considered before making the final diagnosis.
It is also important to make a distinction between the efficacy of some of these strategies to improve diagnosis and treatment or patient outcomes. The authors provide the example of implementation of clinical decision support systems that are designed to increase following best practices and decreasing medical errors, but this strategy has not been shown to improve clinical diagnosis. Many of the studies focus on metrics to determine if the new intervention reached the desired endpoint rather than evaluating the effect on clinical diagnosis and patient outcomes.
We made it to the action part of the article and the podcast.
[action music]
The authors describe a plan to help recognize and combat cognitive bias in anesthesiology that involves a two-step approach. The first step is education and awareness. Anesthesia professionals must acknowledge that cognitive bias exists and can have an impact on patient care and patient safety. We must be especially vigilant of bias when detecting changes in patients, diagnosis of clinical conditions, and treatment of pathologies. This first step may seem simple, but it is critical to help keep patients safe.
Step 2 involves implementation of customized interventions on a personal level and system-wide level, and these will be different depending on the institution, team, individual, and clinical situation. Here are some examples:
- The bandwagon effect may be combated at a larger institution by intraoperative consultation with colleagues.
- At smaller institutions, the use of checklists or cognitive aids and consultation with other perioperative providers may be used to decrease diagnostic momentum.
- Anesthetic departments and institutions should implement an adverse event review process and make sure to discuss what role cognitive bias played in the event.
- Simulation training may be used for trainees and practicing clinicians to work through educational scenarios that highlight cognitive bias in action followed by training to utilize strategies, such as modeling team-based situational awareness and improving interdisciplinary communication, to help combat it.
Going forward, it is critical to remain vigilant to identify cognitive bias during anesthesia care and take the necessary steps to keep patients safe. There is a call to action for anesthesia professionals to receive training in recognizing and combating cognitive bias. In addition, customized strategies to combat cognitive bias need to be implemented at individual and institutional levels to improve patient safety.
Before we wrap up for today, we are going to hear from Stephen Rivoli again. I asked him, “What do you hope to see going forward?” Let’s take a listen to what he had to say.
[Rivoli] “Going forward as a profession, a society, as healthcare in general, as we move toward that perfect culture of safety, we’re going to need to continue to address the effect of cognitive biases on patient safety. And we, the authors believe that central in that, and the first step on that path is education.
And that’s why we wrote the article. But going forward in the future, research needs to be done to help develop more tools to help us further and make more progress. Promising examples would be cognitive aids, checklists, information technology. All of these will likely have a role in the future.”
[Bechtel] Thank you so much to Rivoli for contributing the show today. We will be on the lookout for more research on cognitive bias and the development of specific tools in the future.
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
We’ll be back next week with more from the February 2023 APSF Newsletter. And speaking of newsletters, the deadline for the June 2023 APSF Newsletter is just two days away, March 10. So, what are you waiting for, get your submissions in. You could be the next anesthesia patient safety newsletter author. Before you know it, we might be talking about your article right here on this show. For more information, check out the guide for authors over at apsf.org under the newsletter heading. I will include a link in the show notes as well.
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.

