Episode #114 Difficult Airway Management: What’s New in 2022, Part 2
September 6, 2022Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
There is a new 2022 ASA Guidelines for difficult airway management with changes from previous guidelines. Today, we are returning to talking about these updated guidelines as we review the June 2022 APSF Newsletter article by John Fiadjoe and David Mercier, “Anesthesia Patient Safety Foundation Update: 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway.” This is Part 2.
Tune in today as we go through the emergency pathway for Part 3 and considerations for difficult airway management in pediatric patients.
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2022, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. This week, we are headed back into the June 2022 APSF Newsletter and returning to our discussion of the revised and updated difficult airway guidelines. We kicked off the show last week by reviewing the four stages of change. We hope that you are working your way towards adaptation and acceptance as we continue the conversation today.
Before we dive into today’s episode, we’d like to recognize Fresenius Kabi, a major corporate supporter of APSF. Fresenius Kabi has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Fresenius Kabi – we wouldn’t be able to do all that we do without you!”
One of the 10 APSF Patient Safety Priorities is Airway Management including airway management difficulties, skills, and equipment. This is such an important topic for anesthesia patient safety. The new 2022 ASA Guidelines for difficult airway management dropped this year with changes from previous guidelines. Today, we are headed back into the June 2022 APSF Newsletter article by John Fiadjoe and David Mercier, “Anesthesia Patient Safety Foundation Update: 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway.” To follow along with us, head over to APSF.org and click on the Newsletter Heading. First one down is the current issue, June 2022. Then scroll down until you see our featured article today. I will include a link to this article in the show notes as well. If you haven’t listened to Episode 113 yet, we hope that it is up next on your playlist.
Let’s take a moment to do a quick review from last week. One of the most important considerations on the revised difficult airway management algorithm is for continued oxygen delivery throughout difficult airway management and during extubation as well as using capnography for confirmation of successful tracheal intubation. In addition, it is important to consider an awake intubation for adult patients in the following situations:
- Difficult ventilation (either face mask or supraglottic airway
- Increased risk of aspiration
- Intolerance of brief apnea
- Expected difficulty with emergency invasive airway access
We went through part 1 and 2 of the chart last week. We’re going to pick back up where we left off in Part 3.
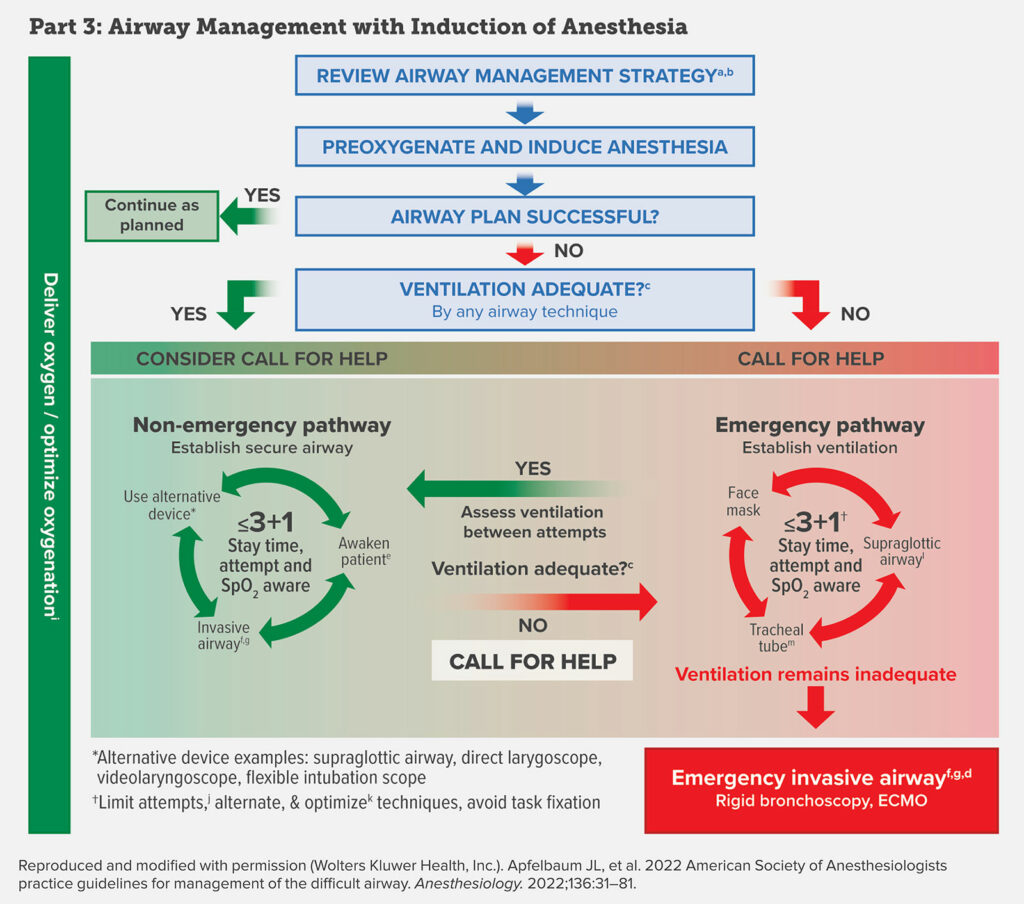
This is Airway Management with Induction of Anesthesia. The first step is to review the airway management strategy. This is such an important step during awake or asleep airway management and includes deciding on the technique for securing the airway based on the airway manager’s choice of technique and experiences, the patient, the procedure, and the available equipment. The next step is Pre-oxygenation and Induction of Anesthesia. Now, was your airway plan successful? If it was, then confirm adequate ventilation with capnography and proceed as planned. If the airway plan was unsuccessful, are you able to provide adequate ventilation? Last week, we went through the YES adequate ventilation by face mask or supraglottic airway pathway. This week, we are headed over to the emergency pathway.
Your heart rate may be increasing right now and you will notice that on the chart, this pathway is highlighted in RED which means that at this time adequate ventilation is not possible. This is the time to call for help! The priority is to establish the ability to ventilate. Once again on the chart there is the less than or equal to 3+1 in the middle of a cycle with three options including face mask, supraglottic airway, and tracheal tube. For the less than or equal to 3+1, this represents limiting the total number of attempts, or alternative techniques and optimizing the patient in between attempts, and avoiding task fixation. It is critical not to continue with the same technique that did not work on earlier attempts because this may lead to increased risk for bleeding, edema, and airway trauma which may further increase the difficulty of mask ventilation and securing the airway. The approach suggested here is to limit attempts with any technique class including face mask, supraglottic airway, and tracheal tube to three and then reserving one additional attempt by a clinician with higher skills. In between each attempt, it is so important to optimize the patient which may include suction, muscle relaxants, and repositioning. During face mask ventilation, you may need and oral or nasal airway or two handed mask grip to establish ventilation. When placing a supraglottic airway, optimization may include evaluating the device size, design, and even first generation compared to second generation devices. In addition, you will want to consider a supraglottic airway with intubating capability for either the initial or rescue supraglottic device. If ventilation with this supraglottic device is successful then you will move back over to the non-emergency pathway and have the option of securing the airway with an endotracheal tube through the supraglottic device. Other consideration for the option of placing an endotracheal tube is to use video laryngoscopy for the initial or rescue tracheal intubation.
Between each attempt, it is important to assess ventilation with capnography and if you establish adequate ventilation then you can move over the non-emergency pathway and work through the algorithm to establish a secure airway or awaken the patient.
If you progress through the emergency pathway and ventilation remains inadequate, this is the time for an emergency invasive airway. Options may include surgical cricothyroidotomy, needle cricothyroidotomy with a pressure-regulated device, large-bore cannula cricothyroidotomy, or surgical tracheostomy. In rare clinical cases, rigid bronchoscopy and ECMO may be required. Keep in mind that the emergency invasive airway should be obtained by an individual with appropriate training in the invasive airway techniques whenever possible.
After establishing an emergency invasive airway, it is important to ensure adequate ventilation and confirm with capnography. Additional considerations for post-operative care depends on the patient and procedure and airway access and may include steroids, racemic epinephrine, counseling, documentation, team debriefing, and encouraging patient difficult airway registry. Whew, we made it through the adult difficult airway management algorithms.
Do you do time-out procedures prior to an anticipated difficult airway? This is an important step while working to keep patients safe during this critical time. The airway management time out should be completed prior to proceeding with securing the airway or induction of anesthesia. The time out should include role identification including the primary airway manager, the backup airway manager, the required equipment and any backup equipment, and the person available for help.
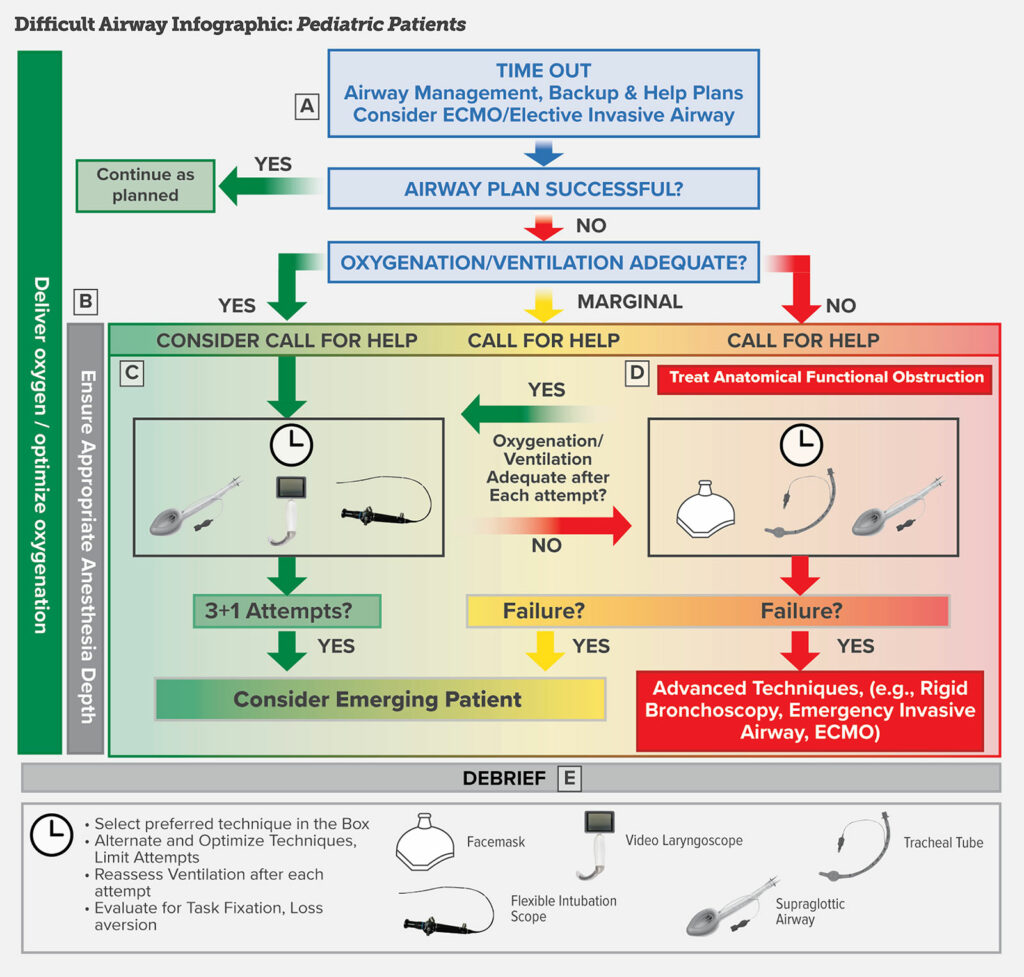
Now, we are moving on to one of the brand new sections for the guidelines and this is the pediatric algorithm. Here we go! You can find the pediatric algorithm in the article and I will include it in the show notes as well. There are three main tools to help with difficult airway management in a child.
- The supraglottic airway
- Flexible intubation scope
- And the video laryngoscope
Keep in mind that these devices may be combined during airway management if you are unsuccessful with the individual devices. In addition, it is important to ensure adequate ventilation in between attempts to secure the airway and when ventilation is easy, you can utilize these devices or combination of devices to secure the airway. If you are unable to establish adequate ventilation, then this becomes the priority and options include facemask, supraglottic airway device, adjuncts, and best attempt to perform tracheal intubation with the technique that is most likely to be successful. Once again, it is vital to limit the number of attempts. A difference in the pediatric algorithm is the importance of determining if an obstruction is functional or anatomical because the treatments are different. For functional obstructions, medication administration is necessary to break a laryngospasm or bronchospasm. For an anatomic obstruction, airway devices including oropharyngeal, nasopharyngeal and supraglottic airway devices may be required for treatment. Following securing the airway or emergence, a team debrief is an important part of the difficult airway management algorithm to discuss lessons learned, express difficult emotions, and identify areas for improvement in the future.
We are going to go through the difficult airway infographic for pediatric patients. Here are some highlights to be on the lookout for:
- Early considerations for ECMO in pediatric airway management.
- Airway management after inhaled induction of anesthesia is common for pediatric patients while awake intubation is much less common.
- Importance for maintaining adequate depth of anesthesia with ventilation assessment after every intubation attempt
- Goal to minimize number of attempts
- Rigid bronchoscopy may be considered by a clinician trained with this device for rescue
- Be careful with airway exchange catheters because there is an increased risk for pneumothorax and pneumomediastinum if the catheter perforates the airway and a smaller margin for error in pediatric patients.
Let’s work our way through the infographic now. The first step is the Time out to identify the plan for airway management with a team-based approach. It is important to assign the following: the primary airway manager, the backup manager, the primary equipment and backup equipment and the person or people to call for help. In certain situations when noninvasive airway management is likely to fail, it is necessary to contact an ECMO team or otolaryngologic surgeon to assist. This may be for patients with congenital high airway obstruction or an airway tumor.
After the time out and proceeding with your airway management plan, if you were successful, then you may continue as planned. If your initial airway management plan was unsuccessful, are you able to provide adequate oxygenation and ventilation? If the answer is YES, then you stay on the green non-emergency pathway. Make sure that you continue to deliver oxygen throughout the airway management procedure and consider calling for help. The next attempt should be with the technique or device most familiar to the primary airway manager which may include a supraglottic device, video laryngoscopy, flexible bronchoscopy or a combination of these devices. Other techniques may include lighted stylet or rigid stylet depending on the clinician preference. Make sure that you optimize patients in between attempts with alternative devices as needed and assess ventilation after each attempt. Once again, it is critical to limit the number of attempts with the following strategy: one attempt at direct laryngoscopy with consideration for video laryngoscopy instead of a direct laryngoscopy attempt making sure that the total attempts by the primary airway manager is only 3 with one additional attempt by a secondary airway manager. Then, after 4 attempts, consideration for emerging the patient and reversing anesthetic drugs if possible. Further attempts to secure the airway may be considered only if the risks and benefits to the patient favor continued attempts at airway management.
What if you are unable to provide adequate oxygenation or ventilation? Now, you are on the marginal or emergency pathway. This is the time to call for help. The first step is to treat any functional or anatomical obstruction. Next, attempt to improve ventilation with facemask, tracheal intubation, and supraglottic device. If these devices and attempts fail, then you need to consider emerging the patient (as long as you are able to provide some oxygenation and ventilation) or proceeding with advanced invasive airway techniques with may include rigid bronchoscopy, emergency invasive airway, or ECMO.
After all cases of difficult airway management, it is important to conduct a team debrief. This will help to highlight what went well during the procedure, what areas need improvement, and to provide emotional support to team members especially if there is a patient morbidity or mortality.
As we begin to wrap up for today, we are returning to the article to discuss updates to the guidelines related to devices and technology. The use of a video laryngoscope for patients with an anticipated difficult airway has been shown to provide a better laryngeal view and improved first-attempt success compared to direct laryngoscopy in several meta analyses with equivocal results comparing video-assisted laryngoscopy to flexible intubation scopes. In addition, studies have revealed equivocal results for hyper-angulated video laryngoscopes compared to non-angulated video laryngoscopes in patients with anticipated difficult airways. The combination of techniques may be helpful as well such as using a flexible intubation scope through a supraglottic airway had a higher first-attempt success rate than using the flexible intubation scope alone.
After securing the airway for a patient with a difficult airway, extubation is another critical time because you do not want to have to reintubate the patient if at all possible. Make sure you have a clear extubation plan in place with a strategy for reintubation if necessary. Your plan will depend on the healthcare team members, extubation location, and available equipment. You may want to leave an airway exchange catheter in place or consider placing a laryngeal mask for possible rapid reintubation. Keeping patients safe following difficult airway management depends on clear documentation of how the airway was secured in the medical record which may be used for future airway management procedures. Patients will need this information as well in the form of a letter for their records and should be encouraged to register with an emergency notification service.
Check out figures 3 and 4 in the article for the black and white difficult management algorithms for adult and pediatric patients. These guidelines received approval from the ASA House of Delegates at the ASA annual meeting in October 2021.
To wrap up the show for today, I will read the authors’ conclusion about the new guidelines:
“They highlight the importance of risk assessment, provide a new decision tree to help determine when to consider awake airway management, awareness of task fixation and time passage, limiting the number of tracheal intubation attempts, and assessing ventilation after every intervention. Finally, they highlight the need to confirm intubation with capnography, plan for extubation, document the airway management in the medical record, and provide documentation to the patient. Welcome to the final stage of change.”
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today. Have you joined the conversation on twitter? If so, we would love for you to tag us in a tweet using #ASPF podcast and tell us where you like to listen to the show. Thanks for listening and we can’t wait to hear from you!
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2022, The Anesthesia Patient Safety Foundation