Episode #113 Difficult Airway Management: What’s New in 2022?
August 30, 2022Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
There is a new 2022 ASA Guidelines for difficult airway management with changes from previous guidelines. Today, we are going to be talking about these updated guidelines as we review the June 2022 APSF Newsletter article by John Fiadjoe and David Mercier, “Anesthesia Patient Safety Foundation Update: 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway.”
Here is the link to the Friday Forward blog by Robert Glazer which discusses the 4 stages of change.
Tune in today as we go through Part 1, Part 2, and the Non-emergency pathway for Part 3. We’ll be back next week to continue the conversation on difficult airway management.
For a historical perspective of the return of the patient safety literature summaries that are back in the APSF Newsletter and on the website, check out the article by John Eichhorn published in between issues on August 1 2022, “That Which is Old is New Again – APSF Newsletter “In the Literature” Synopsis Summaries Reappear.”
Check out the In The Literature Section to stay up to date on the latest in anesthesia patient safety.
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2022, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. This week, we are headed back into the June 2022 APSF Newsletter. We have a brand-new show, new content and new guidance for difficult airway management.
But before we dive into the episode today, you’ve heard me recognize our corporate supporters on this show, but there’s another supporter who is absolutely essential – YOU! Every individual donation matters so much. Please visit APSF.org and click on the Our Donors heading and consider making a tax-deductible donation to the APSF.
One of the 10 APSF Patient Safety Priorities is Airway Management including airway management difficulties, skills, and equipment. This topic is near and dear to the hearts and clinical practice of all anesthesia professionals and is a critical part of keeping patients safe during anesthesia care. As I mentioned on the show last week, there are new 2022 ASA Guidelines for difficult airway management with changes from previous guidelines. Today we are going to be talking about these updated guidelines as we review the June 2022 APSF Newsletter article by John Fiadjoe and David Mercier, “Anesthesia Patient Safety Foundation Update: 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway.” To follow along with us, head over to APSF.org and click on the Newsletter Heading. First one down is the current issue, June 2022. Then scroll down until you see our featured article today. I will include a link to this article in the show notes as well.
Are you ready for it? Updated Difficult Airway Management Guidelines? There are some big changes with these recent updates. Change can be good and represent new ways to keep patients safe in the face of the continued patient safety threats of human factors, team-based performance, and cognitive errors with improved clinical decision-making during critical situations. The APSF article authors point out that change may also be difficult and introduce Robert Glazer, founder and chairman of the Board of a global partner marketing agency and author of a weekly blog called “Friday Forward.” I will include a link to the blog in the show notes as well. Glazer describes the four stages of change and I’m going to read through them now:
- Confusion and surprise—“Huh? why did you change that?”
- Reacting to differences—“Why is this different, not sure I like that.”
- Pining for the past—“Oh, I wish I had the old version back.”
- Adaptation and acceptance—“Hmm, this may actually be better, I think I like it.”
What was your reaction to the updated airway management guidelines from the ASA? What stage did you start at? What stage are you in now? We are going to get into the revised guidelines now and work towards that last stage of change, adaptation and acceptance. So, go ahead and fix that cup of coffee or tea, set off on your walk or jog because here we go.
Did you know that the first ASA Practice Guidelines for Management of the Difficult Airway was published in 1993? Then, these guidelines are reviewed every 5 years by the Committee on Practice Parameters with a complete revision at least every 10 years. This latest version was published in January 2022 and represents the revision of the 2013 version of the guidelines developed by an international task force with anesthesiologists and methodologists from the United States, India, Ireland, Italy, Switzerland and several subspeciality organizations as well. For anesthesia professionals who take care of pediatric patients, the guidelines have expanded to include evidence and expert opinion on pediatric difficult airway management as well. There may be a lot of changes in the revised guidelines and that it is because a lot of work went into these considerations including 560 references, surveys of expert consultants, ASA members, and 10 participating organizations, and updates on the equipment and available technology.
The TL;DR of these revised guidelines is consideration for continued oxygen delivery throughout difficult airway management and during extubation as well as using capnography for confirmation of successful tracheal intubation. But we are not going to stop at there. We are getting into all of the details of the airway management algorithm so don’t touch that dial.
Another important consideration for these new guidelines is the focus on paying attention to the passage of time while performing airway management. This is important because during critical situations there may be a tendency towards task fixation with multiple failed attempts at the same approach without considering alternative techniques. This puts the patient for increased risk of airway trauma and persistent failure to secure the airway. This is a call for increased situational awareness while working through the airway algorithm which may even mean that you end up at the surgical airway pathway earlier. One option is to assign the role of arbiter of task fixation to a member of the healthcare team who is not involved in hands-on airway management to help guide the healthcare team through the difficult airway algorithm.
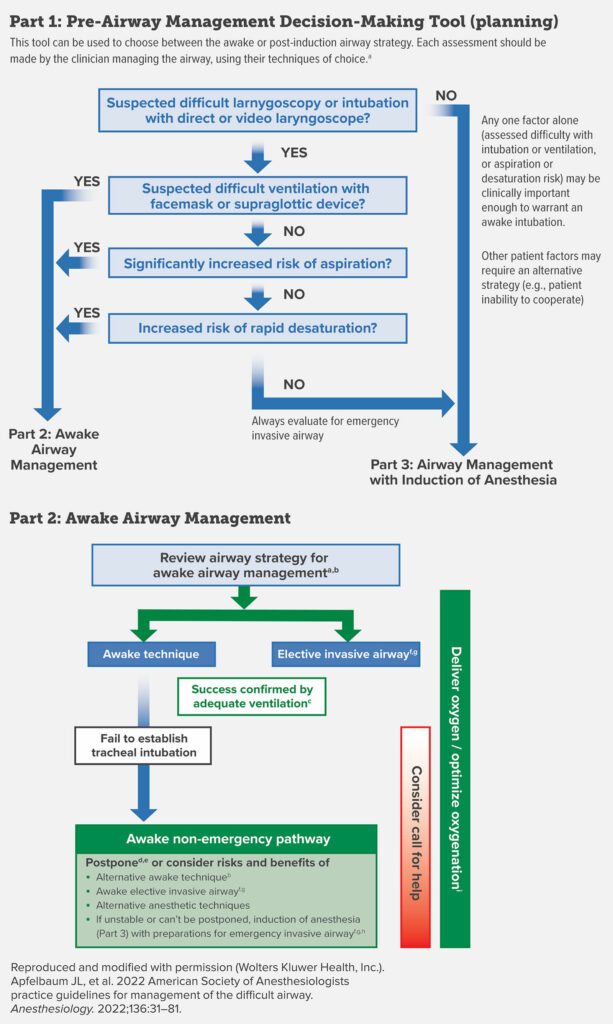
A threat to patient safety that was identified since the previous guidelines were published is judgement error in not performing an awake intubation when it is indicated which has led to complications and failure to secure the airway. As a result, the updated guidelines include a pre-induction decision chart for awake compared to asleep airway management. Check out Figure 1 in the article and we will be going through it as well. It is important to consider an awake intubation for adult patients in the following situations:
- Difficult ventilation (either face mask or supraglottic airway
- Increased risk of aspiration
- Intolerance of brief apnea
- Expected difficulty with emergency invasive airway access
Let’s go through part 1 now. This is the Pre-airway Management Decision-Making Tool which can be used when deciding between securing the airway awake or post-induction. First, do you suspect difficult laryngoscopy or intubation with direct or video laryngoscope? If the answer is No, then you may proceed to part 3 and airway management with induction, but the chart reminds us that any single factor may be enough of an indication for securing the airway awake and don’t forget about additional considerations including patient’s ability to cooperate and hemodynamic stability. Now, if the answer to the first question was YES, there is a series of 3 additional questions.
- Do you suspect difficult ventilation with facemask or supraglottic device?
- Is there a significantly increased risk for aspiration?
- Is there an increased risk for rapid desaturation?
If the answer is YES to any of these questions, then proceed to Part 2 Awake Airway Management. If the answer is No, then continue to the next question in the series. If you made it through all 3 additional questions with No answers then you can proceed to part 3 and airway management with induction, but don’t forget to evaluate for emergency invasive airway as well.
Next up, let’s review part 2 of the chart and awake airway management. The first step here is to review the airway strategy for awake airway management. It is up to the airway manager to complete an assessment and decide on equipment and technique for awake airway management based on previous experience, available resources including equipment and the availability and competency of help, and the clinical context. Awake airway management may include flexible fiberoptic intubation scope, video laryngoscopy, direct laryngoscopy, supraglottic airway, combined devices, and retrograde wire-aided.
Here are some important considerations for keeping patients safe during an awake intubation.
- Anatomical and physiologic airway difficult risk
- Aspiration risk
- Infection risk
- Other exposure risk
- Equipment and monitoring check
- Role Assignment
- Back-up and Rescue plans.
Now, we are proceeding with awake airway management. It is important to deliver oxygen and optimize oxygenation throughout the procedure. This may include low or high-flow nasal oxygen, head elevated position, and non-invasive ventilation during preoxygenation.
The first branch point is an awake technique or an elective invasive airway. An invasive airway may include surgical cricothyroidotomy, needle cricothyroidotomy with a pressure-regulated device, large-bore cannula cricothyroidotomy, or surgical tracheostomy as well as retrograde wire-guided intubation and percutaneous tracheostomy. There are rare situations where rigid bronchoscopy or ECMO may be options as well. Keeping patients safe during elective invasive airways also means that this procedure is performed by someone trained in the invasive airway technique whenever possible.
At this point, either awake intubation or elective invasive airway, if the procedure is successful, then it is critical to confirm placement and ensure adequate ventilation with capnography.
What do you do if the awake intubation is unsuccessful? This is the time to consider calling for help and you can proceed to the awake non-emergency pathway. This pathway includes either postponing the procedure or consider the risks and benefits of the following:
- An alternative awake technique
- An awake elective invasive airway
- Alternative anesthetic techniques
- And finally, if the patient is unstable or if airway management is absolute necessary after a failed awake intubation, this is the time to proceed with induction of anesthesia with preparations for possible emergency invasive airway
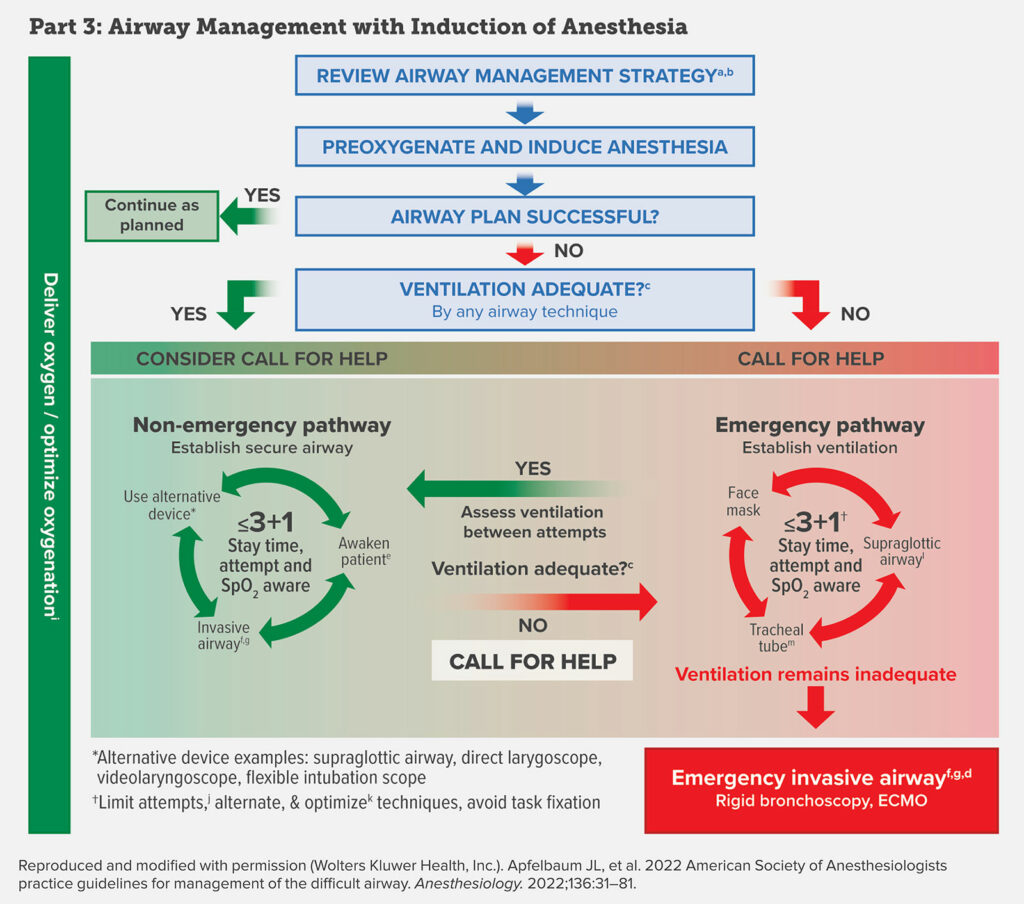
We are moving on to Part 3 of the Chart. This is Airway Management with Induction of Anesthesia. Remember, throughout these steps it is important to deliver oxygen and optimize oxygenation to help keep patients safe. The first step is to review the airway management strategy. This is such an important step during awake or asleep airway management and includes deciding on the technique for securing the airway based on the airway manager’s choice of technique and experiences, the patient, the procedure, and the available equipment. The next step is Pre-oxygenation and Induction of Anesthesia. Now, was your airway plan successful? If it was, then confirm adequate ventilation with capnography and proceed as planned. If the airway plan was unsuccessful, are you able to provide adequate ventilation? Let’s go through the YES, adequate ventilation by face mask or supraglottic airway pathway first. You will want to consider calling for help at this point. You are now on the non-emergency pathway with a goal to establish a secure airway.
The chart is a cycle with less than or equal to 3+1, Stay time, attempt and SPO2 aware in the middle and 3 options of use alternative device, awake patient, invasive airway. The less than or equal to 3+1 refers to limiting attempts at tracheal intubation and supraglottic airway insertion to decrease risk for bleeding, edema, airway trauma which may lead to increased difficulty with mask ventilation or securing the airway. Keep in mind that persistent attempts at any airway intervention, even inadequate mask ventilation, may lead to a delay in an emergency invasive airway and increased risk for complications. The approach here is to limit attempts with any technique class, that is face mask, supraglottic airway, tracheal tube to 3 attempts and reserve one attempt for a clinician with high skills. Hence, 3+1. As you work through the non-emergency pathway to secure the airway, it is critical to make sure that you are providing adequate ventilation. As long as you are, then you remain on the non-emergency pathway. Alternative devices may include supraglottic airway, direct laryngoscope, video laryngoscope, and flexible fiberoptic scope. In addition, when you are on the non-emergency pathway, you still have the option to awake the patient and this may be a life-saving decision. When deciding to awake the patient and postpone the case and intubation, the goal is to bring the patient back with appropriate resources to be successful in the future including personnel, equipment, patient preparation, or planned awake intubation.
So far we have stayed in the planning phases and green areas which represent adequate ventilation on the airway management chart, but there is still so much to talk about include the emergency pathway and pediatric difficult airway management. You will have to tune in next week as we continue the conversation and check out the show notes for the updated adult difficult airway infographic.
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
There’s a new revitalized column in the APSF Newsletter and section on the website called “In the Literature.” You can find it by heading over to APSF.org and clicking on the patient safety resources heading. Fifth one down is in the literature. This section includes summaries of current patient safety literature that is of interest to our readers. This is not a brand new idea for the APSF since literature summaries have formed an integral part of the APSF Newsletter since the original Newsletter in 1986 which included a column called “From the Literature.” For more information, check out the article by John Eichhorn published in between issues on the first of August 2022, “That Which is Old is New Again – APSF Newsletter “In the Literature” Synopsis Summaries Reappear.” Which summaries have you read so far? Are there any articles you would like to see summarized in this section? Have you completed a literature summary that you would like to see included in this section? You can contact that Newsletter editors at any time. This is a great way to stay up to date on the latest in anesthesia patient safety.
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2022, The Anesthesia Patient Safety Foundation