We respond to Yerdon et al.’s call to action on intraoperative hypotension (IOH). Although we applaud and agree with the authors’ suggestions, they omit an important cause of IOH: the amount of anesthesia given. When appropriate, simply decreasing anesthesia delivery will often improve MAP, avoiding hypotension and the administration of unnecessary fluid and potentially harmful vasoactive medications.
TO THE EDITORS
Yerdon, Sherrer, and Chappell’s comprehensive APSF article underscores the crucial link between intraoperative hypotension (IOH) and adverse postoperative outcomes, such as acute kidney injury, myocardial injury after non-cardiac surgery, delirium, stroke, readmissions, and mortality. Their article highlights the profound impact IOH has on patients and the healthcare system. However, IOH may be incurred by significant practice variation, making it a modifiable risk factor that demands attention from all anesthesia professionals.1
To prevent, diagnose, and treat IOH, they propose continuous noninvasive blood pressure and intense hemodynamic monitoring, focusing on maintaining mean arterial pressure (MAP). They also suggest goal-directed hemodynamic and fluid therapy. They identify the multifactorial causes of IOH, including reduced myocardial contractility, vasodilation, hypovolemia, bradycardia, and extrinsic compression of heart chambers.
We fully support their call to action. However, we believe the primary and often overlooked cause of IOH is excessive anesthesia,2 which the authors do not address.
In addition to the measures suggested by Yerdon et al., IOH can also be avoided by incorporating a strategy to reduce the administered anesthesia when appropriate (Figure 1). This simple adjustment can often raise MAP, prevent IOH, and reduce the need for vasopressors, inotropes, and fluids, thereby improving patient outcomes. Processed electroencephalogram (EEG) monitoring best accomplishes this adjustment and minimizes the risk of accidental awareness.3
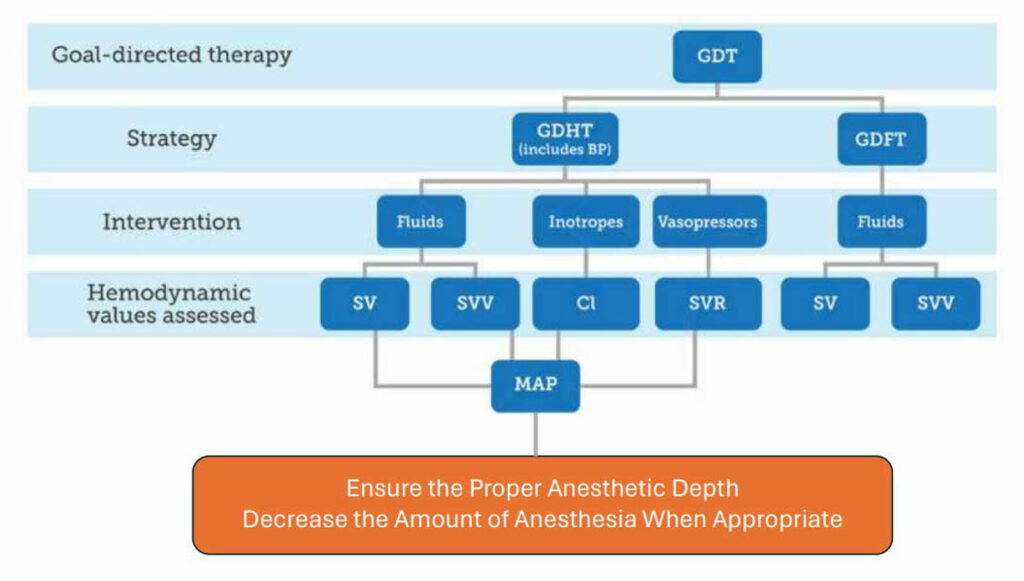
Figure 1. Yerdon’s proposed goal-directed therapy algorithm (blue section). A very common cause of IOH is the delivery of too much anesthesia. Adding “Ensure the Proper Anesthetic Depth, Decrease the Amount of Anesthesia When Appropriate” (orange section) to Yerdon’s algorithm is suggested. Often, this alone will improve the MAP and eliminate the need for additional fluid and/or vasoactive medications that can be detrimental.
Donald H. Lambert, PhD, MD, is a Professor of Anesthesiology at the Boston Medical Center, Boston, MA, USA.
Laura A. Lambert, MD is a Professor of Surgery at the University of Utah/Huntsman Cancer Institute, Salt Lake City UT, USA.
Mauricio Gonzalez, MD, is a Clinical Associate Professor of Anesthesiology at the Boston Medical Center, Boston, MA, USA.
The authors have no conflict of interest.
REFERENCES
- Yerdon, A, Sherrer, DM, Chappell, D. Intraoperative hypotension: a public safety announcement for anesthesia professionals. APSF Newsl. 2024;39(2):42-45.
- Lambert DH. Myocardial and Acute Kidney Injury Associated With Hypotension: Is It Associated With the Depth of Anesthesia and Compensatory Vasopressor Use? Anesth Analg. 2022;134(4):e16-e18. doi:10.1213/ANE.0000000000005894
- Lambert DH. Response to APSF Monitoring Recommendations – EEG to Assess Anesthetic Depth. APSF Articles Between Issues. March 12, 2023.

 Articles
Articles