Production pressure poses a threat to safety, whether it be worker safety in the factory, passenger and crew safety during airplane flight, or patient safety in the operating room.1,2 The anesthesia care team, like any work group, is challenged with maintaining production quality in the face of varying workplace conditions. To evaluate threats to patient safety in the current healthcare climate, it is useful to examine some basic components of quality and mechanisms of quality control.
Quality of care in medicine has been defined by three components: structure, process, and outcome.3 Structure refers to health care resources and their organization, including facilities, equipment and personnel. The process of care is how these resources are used to care for patients. This includes adherence to standards and guidelines, as well as the many individual tasks involved in patient preparation, anesthesia induction, maintenance, emergence and recovery. The outcome is the end result of the patient’s exposure to medical care. In anesthesia, desired outcomes include no harm to the patient, good surgical conditions, and satisfactory postoperative pain control. A desired economic outcome is low cost. A safe anesthesia care process is neither absolutely necessary nor sufficient to ensure a good outcome, as there are factors outside the anesthesiologist’s control (patient physiology, surgical skill, luck) that also contribute to patient outcomes. However, it is believed that a safe process will maximize the chances of a good outcome, and safety in provision of anesthesia care is supported by professional standards, guidelines, and customary practice.
Other contributors to this newsletter have addressed recent trends in production pressure that threaten anesthesia patient safety. Production pressure stems from components of the structure of anesthesia care that are outside the direct control of the anesthesia care team and its leadership. For example, recent trends have seen the surgical caseload increase while reimbursement levels declined and manpower shortages made hiring difficult, leaving the anesthesia team faced with increasing production (changing the process) and maintaining safety (outcomes) with little, if any, control over resources (underlying structure of care). This raises a number of questions:
- Can productivity be increased without eroding quality?
- How can the production process be adjusted to use resources more efficiently?
- What is the upper limit of safe production?
Structure, Process and Outcome: An Example from an Academic Medical Center
The University of Washington Medical Center in Seattle has been faced with increasing surgical caseloads and a relatively fixed number of attending anesthesia staff for the past 10 years. With 17 operating rooms and 10 other anesthetizing locations, 24 FTE (full-time equivalent) attending anesthesiologists have seen a 100% increase in cases between 1991 and 2000 (from roughly 8,000 to 16,000 cases/year). A number of structural components have remained fixed, while others have changed. The number of operating rooms has remained constant, although some rooms remain open for longer hours each day to accommodate the increased caseload. Anesthesia care is provided under a team model, with one attending anesthesiologist supervising anesthesia residents and CRNAs. The number of anesthesia resident positions has remained unchanged; additional CRNAs have been hired to meet anesthesia coverage needs (all working under anesthesiologist supervision). Less than one FTE anesthesiologist has been added to the staff over this period.
Efficient Use of Fixed Resources: Increasing Productivity with Team Anesthesia Care
The challenge to increase productivity with a fixed number of attending anesthesiologists and operating rooms presented several options:
- increase anesthesia hours/day (keep rooms open longer)
- shorten case turnover time
- shorten case duration
- reduce case delays and cancellations
- increase case concurrency (assign each attending anesthesiologist more teams to supervise concurrently)
Each of these options had limits. For example, case duration was controlled by surgeons and was also affected by the teaching mission of the hospital (teaching extends case time). Concurrency was limited by payer regulations as well as teaching goals and policies. An average concurrency of two rooms/attending anesthesiologist was the general goal. For teaching and safety reasons, concurrency was restricted to one room/attending during introductory training (July and August for CA-1 residents and the beginning of cardiac and obstetrics rotations for more advanced residents). A Presurgery Screening Clinic was established to better organize pre-anesthesia patient evaluation and reduce case delays and cancellations. This clinic was staffed by one attending anesthesiologist and one anesthesia resident plus specially trained nurses. After efficiencies were achieved in turnover time, delays and cancellations, and selected rooms were kept open longer each day, attention was turned to optimizing concurrency.
Examination of data from >83,000 anesthetics administered from 1992-1997 showed that mean monthly concurrency before resource restrictions hovered around 1.6 rooms/attending anesthesiologist and never reached the optimum of two rooms/attending. With attention to increasing concurrency, mean monthly concurrency reached two rooms/attending anesthesiologist and continued to hover at that level. The highest concurrency was 2.2 rooms/attending anesthesiologist.4 These increases in concurrency were achieved by increasing the efficiency of attending anesthesiologist resources as well as adding CRNAs to the staff. We adjusted the scheduling process to reduce the number of cases conducted by solo attending anesthesiologists and to limit scheduled 1:1 concurrency to the introductory situations described above. Unscheduled 1:1 concurrency and solo anesthesiologist care still occurred in cases of resident or CRNA absenteeism (e.g., illness). At the lowest mean monthly concurrency levels, corresponding to periods of resident and CRNA shortages, about 14% of cases were conducted by a solo attending anesthesiologist. This was reduced to about 9% when concurrency increased to a monthly mean of two rooms. With increased concurrency of case supervision and more efficient case assignments, the mix of anesthesia teams changed from 72% of cases with residents, 14% supervised CRNAs and 14% solo attending anesthesia care to a mix of 63% residents, 28% supervised CRNAs, and 9% solo attending anesthesia care.4
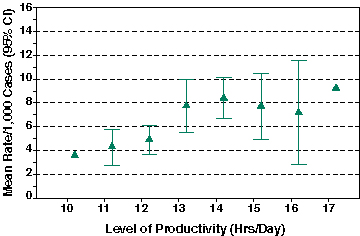
Figure 1: Critical incident rates by productivity level. Triangles represent mean monthly rates of critical incidents at each productivity level. The 95% confidence intervals of the means are displayed as error bars. The lowest (10 hr) and highest (17 hr) productivity levels occurred in single months, so no error bars are provided. Mean monthly rates of critical incidents increased at higher productivity levels (p=0.001). (Adapted from Posner KL, Freund PR. Anesthesiology 1999;91:843.)
The economic goal of optimizing concurrency and other efficiency efforts was to increase productivity, i.e., complete more cases with fixed or declining resources. We measured productivity by dividing total attending anesthesia hours (time units) by the sum of clinical days worked by all attending anesthesiologists each month. This measure captured increased caseload resulting from more efficient use of resources (concurrency, turnover time, delays, etc.) and extended working hours per FTE anesthesiologist. Productivity was highly correlated with concurrency. Productivity increased from an average of 11-12 hours/clinical day to 15-16 hours/clinical day as our anesthesia service achieved more efficient use of resources.4
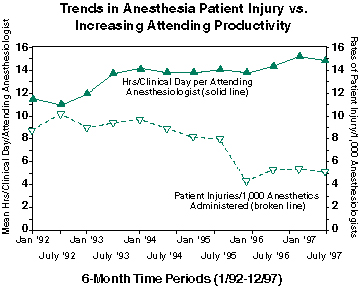
Figure 2: Trends in patient injury by increasing productivity over time. Filled triangles and solid line indicate hours/clinical day for each 6-month period. Open triangles and broken line represent patient injuries/1,000 anesthetics as read on the right-hand vertical axis. During a period of steadily increasing productivity, anesthesia-related patient injuries declined.
Quality Control: Anesthesia Outcomes
Our Anesthesia Service uses a self-reporting CQI Program to track critical incidents and adverse outcomes associated with anesthesia care.5 We were concerned that the increases in productivity might degrade the quality of anesthesia care and examined our CQI database for any evidence of erosion of patient safety. We looked at trends in patient injury or increased levels of care caused by anesthesia problems (i.e., mechanical ventilation in the PACU due to prolonged neuromuscular blockade) that might be correlated to the drive for increased productivity. We also investigated trends in critical incidents (close calls with no resulting injury or increased level of care) and productivity.4
The results of our investigation of productivity vs. quality were somewhat surprising. As shown in Figure 1, we did find an increase in reported critical incidents at higher productivity levels.4 This was not unexpected, and might be interpreted as an indication that we were pushing the limits of safety. Critical incidents are thought to be early warning signs of patient safety concerns and are expected to be correlated with actual adverse outcomes (which, being rare, are more difficult to track). However, we saw a marked decrease in patient injuries and a trend toward lower human error rates at higher productivity levels. The highest patient injury rates occurred at the lowest productivity levels; the lowest patient injury rates occurred at the highest productivity levels (Figure 2). We don’t know if this result suggests that anesthesia teams successfully compensated at higher productivity levels to prevent incidents from progressing to bad outcomes, or if the assumption of critical incidents as indicators of adverse outcomes is incorrect. Other possible explanations may be differences in reporting rates (our data are based on self-reported incidents and outcomes) or other factors such as staff turnover. It is possible that increased productivity corresponded with increased acceptance and appreciation of critical incident reporting for quality improvement, resulting in increased identification of potential safety problems and consequent increased reporting of critical incidents.
Conclusion: Is Increased Productivity Stretching the Limits of Anesthesia Patient Safety?
This case example is drawn from one academic medical center and is limited in the generalizations that can be drawn. There are also limitations in the data used in the analysis, including the self-report nature of the CQI data and the retrospective nature of the analysis with lack of control over extraneous variables. Our example does not indicate that patients are being harmed by increases in efficiency and productivity within a team anesthesia model of care. However, the unexpected decrease in patient injuries with a concurrent increase in critical incidents could be interpreted as a warning. If anesthesia teams became more adept at rescuing adverse events and preventing patient injury at higher productivity levels, can this level of production and safety be maintained over the long term? It is still too early to answer this question. While we can conclude from our limited data that anesthesia care in our institution is still a safe process with generally favorable outcomes, we cannot predict continued safety under continued resource restrictions. It appears that anesthesiologists have effectively maintained the impressive improvements in patient safety that have occurred over recent decades. However, we should remember that the link between the process of care and the outcome is tenuous. Continued favorable outcomes should not be interpreted as evidence that risk of patient injury has not increased. We can only conclude that any erosion in anesthesia patient safety that may be underway has not yet resulted in readily identifiable adverse outcomes that may be the result of pushing the limits of production.
Dr. Posner is Research Associate Professor, and Dr. Freund is Professor (as well as Chief, Anesthesia Clinical Services), University of Washington Medical Center, Department of Anesthesiology, University of Washington, Seattle, WA .
References
Gaba DM, Howard SK, Jump B. Production pressure in the work environment. California anesthesiologists’ attitudes and experiences. Anesthesiology 1994;81:488-500.
Weinger MB, Englund CE: Ergonomic and human factors affecting anesthetic vigilance and monitoring performance in the operating room environment. Anesthesiology 1990;73:995-1021.
Donabedian A. The quality of care. How can it be assessed? JAMA 1988;260:1743-1748.
Posner KL, Freund PR. Trends in quality of anesthesia care associated with changing staffing patterns, productivity, and concurrency of case supervision in a teaching hospital. Anesthesiology 1999;91:839-847.
Posner KL, Kendall-Gallagher D, Wright IH, Glosten B, Gild WM, Cheney FW. Linking process and outcome of care in a continuous quality improvement program for anesthesia services. Am JMed Qual 1994;9:129-137.

