Episode #30 Airway Emergency Preparedness in MRI
February 2, 2021Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
We are returning to the Rapid Response to Questions from our readers column for the show today. Thank you to Dr. Nagpal for submitting this rapid response which appeared in the APSF February 2020 Newsletter, “Airway Emergencies and Safety in Magnetic Resonance Imaging (MRI) Suite.”
We review the four zones in the MRI environment:
- I = Area that is freely accessible without special clearance or supervision needed
- II = Area between Zone I and Zone III
- III = Area in close proximity to the scanner that contains the control room and requires screening prior to entry and supervision.
- IV = Area that contains the MRI scanner
Here is an important graphic for MRI Safety for equipment. Plastic oral airways and bag mask ventilation units are MRI-safe devices while Laryngeal Mask Airways and Endotracheal Tubes are MRI-conditional devices. Metal laryngoscopes are MRI-unsafe and contain ferromagnetic material. There are MRI-conditional laryngoscopes available for use in Zone IV.
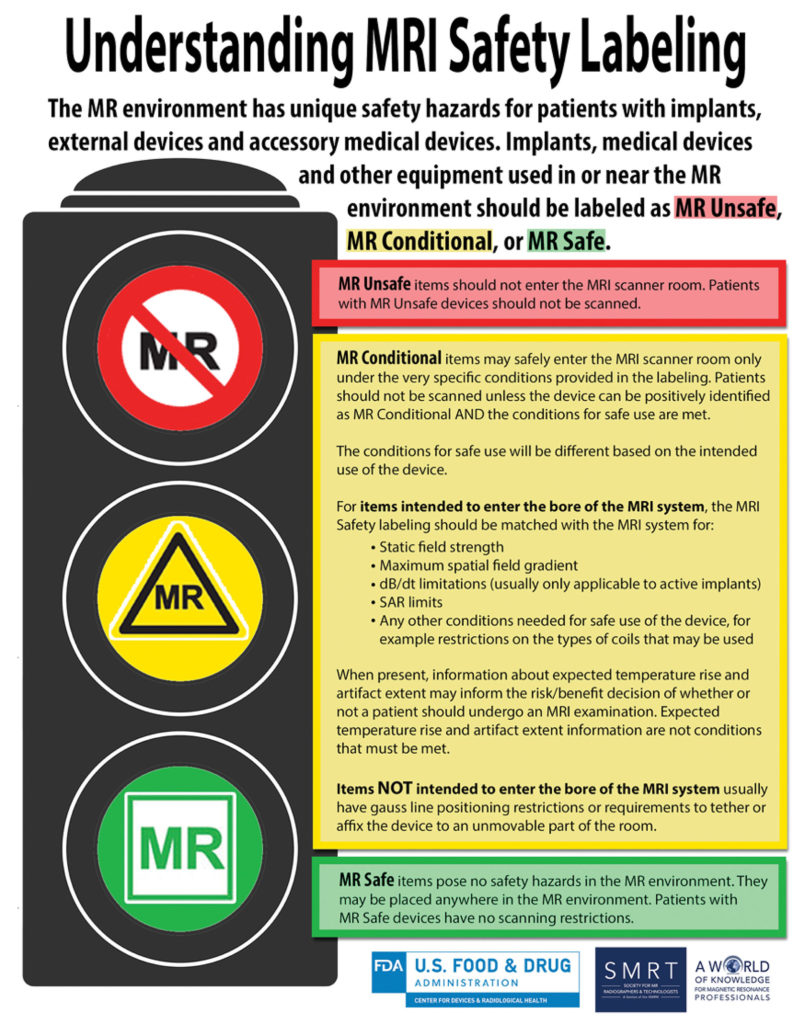
Figure 1: United States Food and Drug Administration. Understanding MRI Safety Labelling. https://www.fda.gov/media/101221/download Accessed on Dec 7, 2019.
For more information about MRI safety, you can check out this resource: http://mrisafety.com/
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
© 2021, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel and I am your host. Thank you for joining us for another show. If you follow APSF on twitter, and we hope that you do at @ APSForg, then you may have seen the tweet from December, “How do you provide safe #anesthesia care in the #MRI suite? In this #APSFRapidResponse article, the authors discuss the basics of MRI safety as well as the need for MRI-compatible equipment.” Well today, we are going to dive into that #APSFRapidResponse article.
Before we dive into today’s episode, we’d like to recognize Merck, a major corporate supporter of APSF. Merck has generously provided unrestricted support as well as research and educational grants to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Merck – we wouldn’t be able to do all that we do without you!”
Our Rapid Response article for today comes to us from the APSF February 2020 Newsletter. Follow along with us by clicking on the Newsletter heading, 4th one down is ASPF Newsletter archives. Then scroll down to February 2020. Then scroll down to the Rapid Response Column on the left and click on the first article. Today, we will be discussing, “Airway Emergencies and Safety in Magnetic Resonance Imaging (MRI) Suite.” Thank you to Dr. Nagpal for submitting this rapid response that I am going to read now.
“Dear Rapid Response:
Are MRI-compatible laryngoscopes recommended or required in the MRI environment?
I am an anesthesiologist presently working in a community hospital and care for patients who receive anesthesia as part of their MRI exam. We have conventional laryngoscopes and blades available in MRI zone III and an MRI-compatible anesthesia machine in zone IV. If we need to intubate a patient, the expectation is that we can move the patient to zone III for intubation and return to zone IV to complete the study. I believe we should purchase MRI-conditional laryngoscopes and blades to be available in zone III, but am told it is not essential and many other institutions do not have MRI-compatible laryngoscopes.
Please let me know your thoughts on this patient safety question.”
This is a great question and so important for anyone providing anesthesia in an MRI environment. Let’s review the response.
Let’s start with what we know about providing anesthesia in remote locations and the MRI environment is often one of the most remote locations due to the locations of the MRI scanner in a hospital. The American Society of Anesthesiologists closed claims project provides some data on the risk involved with anesthesia in remote locations. Findings from this project revealed that claims for death and severe respiratory events were more common in remote locations and during monitored anesthesia care cases. 7 out of the 10 radiology claims came from the MRI environment and 4 of these claims were found to be due to over sedation. The authors write that the patient safety concerns in the MRI environment are significant and warrant having MRI compatible laryngoscopes available for airway management in emergency situations during anesthesia care in the MRI environment. It also imperative to not only have MRI-compatible laryngoscopes available, but also a process for airway management during emergencies that is specific to this unique environment. Unlike the operating room, where equipment and additional persons to help are often immediately available, the MRI environment demands an understanding of the dangers of an MRI scanner to patients and staff.
So, with that, let’s review the MRI environment considerations. First, we will define the zones. There are four zones in the MRI environment, I through IV. Zone 1 includes the area with magnetic fringe fields less than 5 Gauss and includes the areas that are freely accessible without special clearance or supervision. This is often a public area, prior to patient check-in and registration. Zone II represents the area between Zone I and Zone III and it is often where patients are screened for MRI safety during registration and while being supervised by staff. Patient dressing rooms and holding areas are located in this zone. Zone III is the first restricted environment and this area contains the control room. Due to the proximity of the magnet room and the stronger levels of fringe, gradient or magnetic fields, patients and staff must be screened prior to entering Zone III in order to prevent possible harm. Zone IV includes the room with the MRI scanner. Even when the scanner is not in use, the MRI magnetic field is always on and you cannot see it, but any ferromagnetic object of piece of equipment in Zone IV may become a lethal projectile. The greatest risk would be patient or staff death or injury but even if no person is harmed a projectile in the Zone IV may damage the scanner leading to closure for repair or necessitating a costly and dangerous magnet quench event.
Now that we have reviewed the four MRI zones, let’s talk about the labeling for devices and equipment that may be found in the MRI environment. The categories include MR unsafe, MR conditional, and MR safe. There is a figure in the article that includes these definitions and I will include it in the show notes as well. MR unsafe equipment and devices should not to be brought into the MRI scanner or Zone 4. In addition, patients who have MR unsafe devices should not be brought into the MRI scanner. The next category is MR safe and this includes equipment that has no potential for harm in the MRI environment and may be brought into Zone 4. Patients with MR safe devices may be scanned without any restrictions.
The final category is MR conditional. What does this mean? This label is attached to devices that may be brought into the MRI scanner only under certain conditions which are specified in the labeling. Patients with MR Conditional devices can only be scanned if their device is identified as MR conditional and the specific conditions for safety have been met. It is important to remember that the specific conditions may be different depending on the device. For MR conditional items to go through the bore of the MRI scanner, the specifications for the device must match the MRI system including the static field strength, the maximal partial field gradient and other conditions depending on the device. In addition, there may be information about temperature rise and artifact extent that may be helpful when deciding on the risk/benefit analysis for performing an MRI, but these are not conditions that are included in the MR conditional labeling.
It is time for a quick quiz…what category do LMAs and endotracheal tubes fit into? Since these airway devices have small amounts of ferromagnetic material in the pilot balloon, they are MR conditional devices. Using them in an MRI scanner is safe for patients, but may impact the image quality. Other safe airway devices include plastic oral airways and bag mask ventilation units. Older Metal laryngoscopes are MR unsafe since their function is unreliable in Zone IV and the nickel in the battery is ferromagnetic. There are single-use and reusable laryngoscopes that are MRI-conditional that may be used in Zone IV.
Now, that we have reviewed the zones and safety labels for the MRI environment, let’s turn our attention to the most recent ASA Practice Advisory that addresses providing anesthesia and emergency airway management in the MRI environment. The advisory helps to answer our question because it states that MRI safe or MRI conditional airway devices must be immediately available in the MRI suite. Remember, when providing anesthesia care in the MRI environment, you must be ready to enter Zone IV quickly so you will also need to confirm that you do not have any ferromagnetic objects or equipment in your pockets prior to entering the scanner. It is important to make sure that the only airway equipment located in MRI zone III is MRI safe or conditional so that it may be brought into zone IV if needed in an emergency. This is an important safety check to make sure that MRI unsafe equipment is not brought into the MRI scanner during an emergency.
For an airway emergency in the MRI scanner, initial bag-mask ventilation may allow you to be able to move your patient safely to zone III or even zone II where you can safely use any necessary airway equipment and resuscitation equipment to secure the airway and stabilize the patient. In addition, it will be easier for additional healthcare professionals to help take care of the patient if needed when you are in zone II rather than the scanner. Some patients may not be able to be moved safely out of zone IV prior to securing the airway such as for patients with massive aspiration or if you are unable to provide adequate oxygenation and ventilation with bag-mask ventilation. In this case, you will need to use MRI safe or conditional airway equipment. Then, as soon as the airway is secure, it is imperative to move out of zone IV. During the emergency, as long as the patient remains in zone IV, it is important to have someone in charge of making sure that it is safe for emergency personnel and equipment to enter Zone IV. Newer MRI scanners come equipped with tables that can be undocked from the scanner and moved out of zone IV in case of an emergency.
What does the response to an airway emergency in the MRI scanner look like at your hospital? There will be differences depending on the location and emergency personnel available at each hospital. There are some components that need to be in place including collaboration with the radiology department for the location and safety of emergency equipment that can be used in the MRI scanner as well as maintaining an area for resuscitation in close proximity to Zone IV. It is important to have standard operating procedures and policies for emergency airway management in the MRI environment and these policies will need to be updated routinely depending on changes in location, equipment, and availability of anesthesia professionals and other emergency personnel. The Covid pandemic and changes to airway management policies at off-site locations may have necessitated updating the policies in order to help keep patients and healthcare professionals safe as well. This is also a good time to incorporate simulations to make sure that the radiology, anesthesia, and other emergency responders can work together for airway emergencies in the MRI environment…especially in zone IV.
Our rapid response asked about having MR-safe-conditional laryngoscopes and airway equipment immediately available in the MRI environment in case of emergency to bring into zone IV rather than relying on always being able to bring the patient out of the scanner to zone III and making sure that no MRI-unsafe equipment is brought into zone IV. There is a real risk of injury to patients or staff or damage to the scanner if MRI-unsafe equipment is brought into the scanner. Remember, it is difficult to turn off the magnet field from the MRI scanner…this requires a “quench” which is expensive and can be dangerous. Thus, it is so important to maintain MRI safety standards in the face of emergencies in the MRI scanner. This is a call for healthcare institutions and individuals to maintain the highest level of safety in MRI environments including off-site locations, intraoperative MRI operating rooms and even free-standing radiology centers. The APSF acknowledges the risk to anesthesia patient safety in the MRI environment. In fact, this falls under two of the APSF Patient Safety priorities, “safety in non-operating rooms locations” which includes non-operating room MRI scanner locations as well as “airway management difficulties, skills, and equipment.”
When taking care of patients in an MRI environment, it is important to be in the zone, to use sports terminology, and remember the zones as well as to stay vigilant about only using MRI safe-conditional equipment in the MRI scanner…even in an emergency.
Okay, that’s all the time that we have for today. Thank you for joining us for another Rapid Response to Questions from our readers show. If you have any questions or comments from today’s show, please email us at [email protected].
Visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today. Plus, you can find us on twitter and Instagram! See the show notes for more details and we can’t wait for you to tag us in a patient safety related tweet or like our next post on Instagram!! Follow along with us for anesthesia patient safety pictures and stories!!
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2021, The Anesthesia Patient Safety Foundation

