Episode #147 Keeping Patients Safe During Liver Transplantation
April 25, 2023Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
Our featured article today is “Evolving Safety Challenges in Patients Presenting for Liver Transplantation Today: A Single-Center Experience” by Khoa Tran, MD; Ashraf Sedra, MD; Joseph Szokol, MD, JD, MBA. Check out the article here.
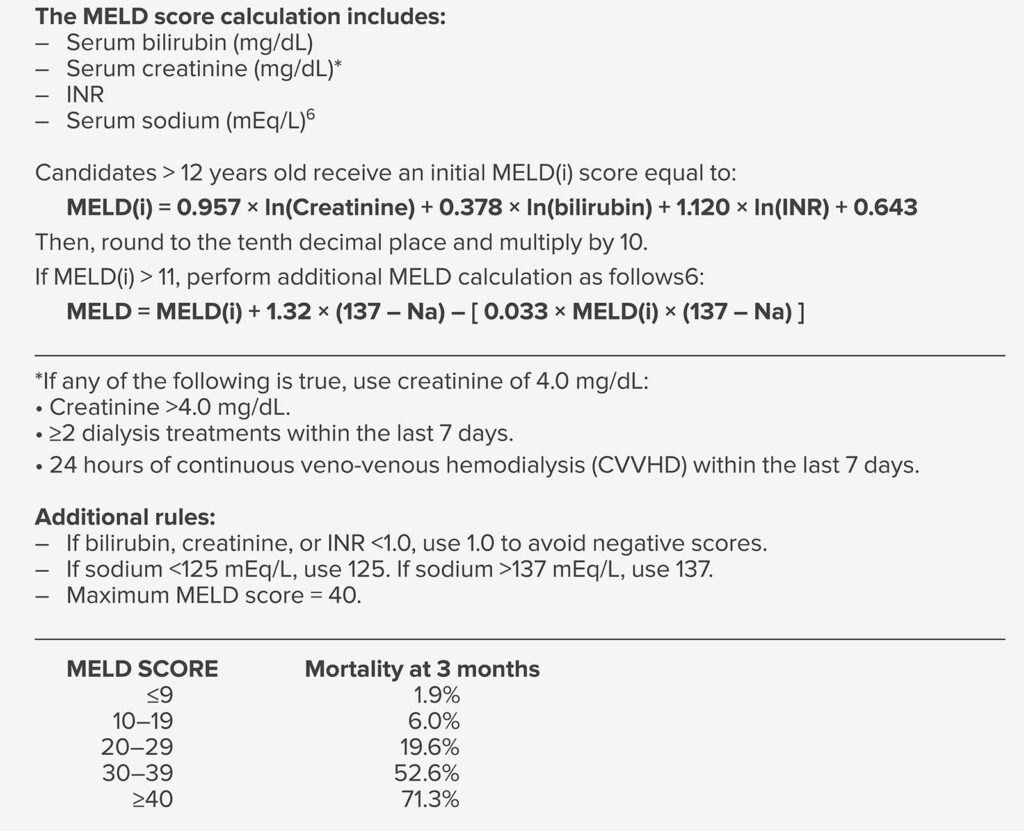
Table 1: MELD Score Components and 3 Month Mortality Prediction5
Did you know that dedicated liver transplant anesthesia teams are associated with reductions in the following?
- Transfusions
- time of postoperative ventilation
- length of stay in the intensive care unit
- perioperative mortality
The patient identification and ABO verification process are very important during liver transplantation. Here are some of the considerations.
The necessary information for verification includes the following:
- Organ type
- Donor and recipient ID
- Donor and recipient ABO blood type
- Recipient date of birth and medical record number
This information must be checked and confirmed by two licensed health care professionals at the following times:
- During living donor registration
- Prior to living donor organ recovery
- Prior to organ receipt in the operating room if recipient surgery starts before organ receipt in the operating room.
- And Upon organ receipt in the operating room.
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2023, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. This week, we are checking out another article from the February 2023 APSF Newsletter. Have you taken care of patients for one of the most challenging cases in the operating rooms with frequent hemodynamic changes, the possibility for massive blood loss and coagulopathy in sick patients and often takes place in the middle of the night. That’s right. Today, we are talking about keeping patients safe during anesthesia care for liver transplantation.
Before we dive into the episode today, we’d like to recognize Merck, a major corporate supporter of APSF. Merck has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Merck – we wouldn’t be able to do all that we do without you!”
Our featured article today is “Evolving Safety Challenges in Patients Presenting for Liver Transplantation Today: A Single-Center Experience” by Tran, Sedra, and Szokol. To follow along with us, head over to APSF.org and click on the Newsletter heading. First one down is the current issue. From here, scroll down until you get to our featured article today. I will include a link in the show notes as well. We have talked about anesthesia patient safety in different areas of the hospital from the maternity wards to non-operating room anesthesia suites, but this time, we are heading into the main operating room to talk about one of the most challenging cases, liver transplant. So, go ahead and grab a cup of coffee or tea because here we go!
The authors kick off the article by discussing the Institute of Medicine report, “To Err is Human” published over 20 years ago which reported that up to 98,000 deaths occurred in hospitals each year due to medical errors across all specialties. Over the past 20 years, there has been a significant improvement in anesthesia patient safety with improvements in training, equipment, and standardized protocols. If we turn our focus to providing anesthesia care for liver transplantation patients, we can see that this remains one of the most challenging perioperative cases for anesthesia professionals and the entire multidisciplinary team including anesthesia, surgery, nursing, and critical care teams; plus perfusionists, blood bank, and dialysis professionals. These are not easy cases: technically challenging surgery, sick patients often with multiple comorbidities related to liver failure, and an intraoperative course where you cannot let your guard down with hemodynamic instability, acid-base and metabolic derangements, coagulation complications, large fluid shifts, and a higher rate of intraoperative death than any other surgical procedure.
Let’s talk about the liver transplantation procedure. More liver transplants are being performed each year, but keep in mind that the number of donated organs has reached a plateau. In 2002, the Model for End-Stage Liver Disease or MELD based system was started to make sure that the sickest patients could receive their transplant first. Check out Table 1 in the article which reviews the MELD score components and the 3-month mortality prediction. We are going to review it now. The MELD score calculation includes the following:
- Serum bilirubin
- Serum creatinine
- INR
- And Serum sodium
From here, patients who are greater than 12 years old receive an initial MELD score calculation. Check out the equation in Table 1. If the initial MELD is greater than 11, then you can perform an additional MELD calculation. There are additional rules that may apply when calculating the MELD score that are included in the table. For example, if the patient has received dialysis or continuous veno-venous hemodialysis therapy in the past 7 days, then the creatinine value for the MELD calculation should be 4. Another additional consideration is that the Max MELD score is 40. Once you have calculated the MELD score, you can use this value to determine the mortality at 3 months. For a MELD score less than or equal to 9, the 3-month mortality is 1.9%. For MELD score between 10 and 19, the 3-month mortality increases to 6%. For MELD scores between 20 and 29, the 3-month morality is 19.6% and this increases to 52% for MELD scores between 30-39. Once the MELD score reaches 40, the 3-month mortality is at 71.3%. As the MELD score increases, patients are more likely to have abnormal levels of bilirubin, creatinine, INR, and sodium and these changes are associated with increased perioperative risk as well. Not only is the anesthetic management during liver transplant surgery technically challenging, but the patients presenting for this surgery have significant comorbidities leading to increased risk for perioperative complications. Patients presenting for liver transplant surgery today have the following characteristics that differentiate them from patients presenting 20 years ago in the pre-MELD era:
- Higher MELD scores
- Advanced liver disease
- Older age
- More significant preoperative comorbidities
- More renal and electrolyte abnormalities
- Increased transfusion and vasopressor requirements during surgery
The authors describe additional considerations for patient location on the transplant waiting lists due to the significant competition in heavily populated areas where there are more transplant centers. For example, the author’s institution is the University of Southern California which is a high-volume transplant center in the Los Angeles metropolitan area that must compete with two other centers and all three centers are within a 20-mile radius. Did you know that the second busiest liver transplant program in the United States is the combination of Keck Hospital and Children’s Hospital Los Angeles? The competition between busy transplant centers may be a threat to patient safety when centers are driven to perform more transplant surgeries with even more challenging patients added to the waiting list. As a result, providing safe anesthesia care during liver transplant surgery has become more challenging over time. The good news is that the authors provide an overview of processes developed and used at the University of Southern California to help keep patients safe. Don’t turn that dial because we are going to review these safety considerations next.
Does your hospital have a designated liver transplant anesthesia team? This is such an important part in helping to keep patients safe that in 2011, the Organ Procurement and Transplant Network/United Network for Organ Sharing instituted the requirement that all transplant centers appoint a director of liver transplant anesthesia. If you are a director at your institution, way to go! This was an important first step in the formation of the independent subspeciality of liver transplant anesthesia. The next step was the creation of liver transplant anesthesia teams and fellowships for additional training. If we look at the literature, dedicated liver transplant anesthesia teams are associated with reductions in the following:
- Transfusions
- time of postoperative ventilation
- length of stay in the intensive care unit
- perioperative mortality
Outside of the operating room, the liver transplant anesthesia team has a few other vial roles. Anesthesia professionals may be involved with the patient selection committee along with a multidisciplinary team of transplant coordinators, surgeons, hepatologists, nephrologists, infectious disease specialists, and social workers. At the author’s instruction, this committee meets every week to discuss possible patients for the waiting list taking into consideration the liver history, additional comorbidities, social support, substance abuse, and finances. The next step is an ordered review of possible exclusion criteria. It is imperative that anesthesia professionals are involved at this early step to make sure that patients are evaluated before presenting for liver transplant. This also allows time for patients to be evaluated in the preoperative anesthesia clinic for further evaluation by an anesthesia professional.
The next process includes Pre-transplant evaluation and ABO verification. Blood type verification is a critical step that must be done at multiple and defined points during the transplantation process to help keep patients safe and make sure there is compatibility between the donors and recipients.
The necessary information for verification includes the following:
- Organ type
- Donor and recipient ID
- Donor and recipient ABO blood type
- Recipient date of birth and medical record number
This information must be checked and confirmed by two licensed health care professionals at the following times:
- During living donor registration
- Prior to living donor organ recovery
- Prior to organ receipt in the operating room if recipient surgery starts before organ receipt in the operating room.
- And Upon organ receipt in the operating room.
Keep in mind that if the recipient surgery begins before organ arrives in the operating room, then the verification must take place prior to induction of anesthesia or prior to incision. Another important step is electronic verification of all blood components intraoperatively. This is such an important step since liver transplant surgery may require up to 10 times as many units of blood products as a heart transplant procedure. The barcode scanning process for verification is important so that one-person verification may be performed with increased workflow efficiency in the face of a potential massive transfusion. This process also helps to decrease the risk for transfusion error from misidentification.
We have time to introduce one more process today. The author’s provide insight into the patient blood management program at Keck University of Southern California or Keck USC. There is a risk of overuse of blood transfusions. This was highlighted by the Joint Commission’s Overuse Summit in in 2012 and blood transfusion made the top 5 list. Even before the summit, Keck was working to keep patients safe without blood transfusions with the Transfusion Free Surgery and Patient Blood Management Program which was started in 1997 to help patients in the Jehovah’s Witness community. Two years later, in 1999, the first successful transfusion-free living donor liver transplantations were performed at Keck using acute normo-volemic dilution. Over the next five years, there were 27 liver transplantations with living donor and deceased donors performed in Jehovah’s Witness patients at the USC-University Hospital. Given the success of this program, it is important to evaluate the use of blood products for other patients and during other surgeries. Higher rates of blood transfusions are associated with increases in the following:
- Length of hospital stay
- Rates of Infection
- Graft Failure
- Mortality
Minimizing blood product administration is an important consideration during liver transplant to help keep patients safe and decrease cost and hospital length of stay. And we are going to talk about strategies to help do this next week! Plus, we will be discussing intraoperative hemodialysis during liver transplantation. So, mark your calendars.
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
Have you joined the conversation on twitter? If so, we would love for you to tag us in a tweet using #ASPF podcast and tell us where you like to listen to the show or you can tag all of the liver transplant anesthesia professionals that you know!! Thanks for listening and we can’t wait to hear from you soon!
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2023, The Anesthesia Patient Safety Foundation