Episode #145 A Framework for Perioperative Care for Patients infected with Mpox
April 11, 2023Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
Our featured article today is from the February 2023 APSF Newsletter. We are reviewing the article, “Perioperative Considerations for Patients with Mpox” by Jonathan M. Tan, Randy Loftus, Sara McMannus, Desiree Chappell, Melanie Hollidge, MD, Michelle Beam, Morgan Hellman, Raquel Bartz, Richard A. Beers, and Jonathan E. Charnin. To follow along with us, head over to APSF.org and click on the Newsletter heading.
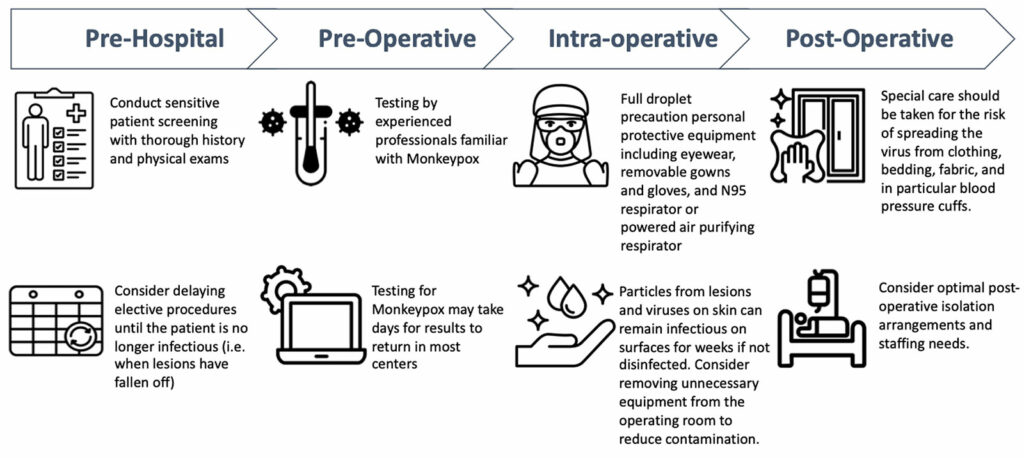
Check out Figure 1 in the article which is a framework for perioperative considerations for patients with mpox. This is based on the joint statement of support and recommendations from the American Society of Anesthesiologists and the Anesthesia Patient Safety Foundation from August 31, 2022.
Check out the current recommendations from the Centers for Disease Control and Prevention website. https://www.cdc.gov/poxvirus/mpox/clinicians/index.html
Here is a comprehensive list of recommended products for disinfection from the EPA website. https://www.epa.gov/pesticide-registration/disinfectants-emerging-viral-pathogens-evps-list-q
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2023, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. Have you provided care for a patient with Mpox, previously known as monkeypox? This is a global health concern with over 78,000 confirmed cases and several thousand probably cases within over 109 countries as of November 7, 2022. Today we are going to review the current evidence and go through a framework for perioperative care for patients infected with Mpox.
Before we dive into the episode today, we’d like to recognize Edwards Lifesciences, a major corporate supporter of APSF. Edwards Lifesciences has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Edwards Lifesciences – we wouldn’t be able to do all that we do without you!”
Our featured article today is from the February 2023 APSF Newsletter. We are reviewing the article, “Perioperative Considerations for Patients with Mpox” by Tan and colleagues. To follow along with us, head over to APSF.org and click on the Newsletter heading. First one down is the current issue. Then, scroll down until you get to our featured article today. I will include a link in the show notes as well.
The World Health Organization changed the preferred name for this virus to Mpox in November 2022 which was first detected in humans in 1970 in the Republic of the Congo and then spread to nonendemic countries in 2022. Anesthesia professionals and members of the healthcare team need to be prepared to keep patients with mpox safe in the perioperative arena with considerations that we will discuss based on the current literature, professional society statements, and current knowledge on the management of infection control of enveloped viruses.
To kick things off, let’s learn a little more about this virus. Mpox is an enveloped, double-stranded DNA virus in the Poxviridae family and orthopoxvirus genus. There are two viral subtypes, the Congo Basin and West African strains. The West African subtype is the dominant strain worldwide and has an estimated mortality rate of 1%. The Congo Basin strain is less dominant, but more easily transmissible between humans with up to a 10% mortality rate. Complications of Mpox include the following: secondary infections, bronchopneumonia, sepsis, encephalitis, and corneal infection leading to vision loss. There is rare nosocomial transmission which may occur through direct contact with affected skin or environmental surfaces and or via respiratory droplets. Given the modes of transmission, anesthesia professionals need to be prepared for infection prevention in the anesthesia work environment.
General recommendations from the WHO issued guidelines for the clinical management and infection prevention and control published in June 2022 include the following:
- contact and droplet precautions for any confirmed patient
- use of respirators and airborne precautions for aerosol-generating procedures.
Check out Figure 1 in the article which is a framework for perioperative considerations for patients with mpox. This is based on the joint statement of support and recommendations from the American Society of Anesthesiologists and the Anesthesia Patient Safety Foundation from August 31, 2022. I will include a link to the statement in the show notes as well. Let’s go through the figure now which is broken down into the following phases: Pre-hospital, Pre-operative, Intra-operative, and Post-Operative.
Pre-Hospital considerations include the following:
- Conduct sensitive patient screening with thorough history and physical exam.
- Consider delaying elective surgery until the patient is no longer infectious as evidenced by when the lesions fall off.
Pre-operative considerations include:
- Testing by experienced professionals familiar with mpox keeping in mind that results may take days to return in most centers.
Once you get into the operating room, the considerations include the following:
- Full droplet precaution personal protective equipment with eyewear, removable gowns and gloves, and N95 respirator or powered air purifying respirator.
- Keep in mind that particles from lesions and viruses on skin can remain infectious on surfaces for weeks if not disinfected. Consider removing unnecessary equipment from the operating rooms to reduce contamination.
During the post-operative period, it is important to consider the following:
- Special care needs to be taken to decrease the risk for viral spreading from clothing, bedding, fabric and this includes blood pressure cuffs. It is also important to consider what is the best postoperative isolation arrangement for the patient which addresses appropriate staffing needs as well.
Next up, let’s talk about screening patients and considerations for elective surgery. It is important to identify patients with Mpox or Mpox exposure before surgery if possible. Mpox exposure includes direct contact with skin lesions or bodily fluids of an infected individual or indirect contact through objects that come into contact skin lesions or bodily fluids. This includes bed linens. Patients with Mpox infection may present with a wide range of symptoms from minimal or no symptoms to fever, malaise, weakness, lymphadenopathy, and a rash that make take 4 weeks to resolve. The skin lesions in Mpox infection may be widespread or limited to a few lesions, may be painful, and often occur in the genital or anorectal areas. Patients with Mpox or report Mpox exposure should have elective surgery deferred until there is no concern for transmission.
Check out Figure 2 in the article for procedural timing considerations for patients exposed or diagnosed with Mpox. Let’s take a closer look at it. For Emergent Procedures, do not delay the surgery and proceed with infection control precautions in all phases of care. For Elective surgery in a patient who reports being exposed, it is important to delay surgery past the 21-day incubation period. During this time, patients should be screened for prodromal symptoms and rashes should be tested for Mpox. For symptomatic patients who are scheduled for elective surgery, keep in mind that the rash usually appears 1-4 days after prodromal symptoms and the infectious period is usually about 4 weeks after the appearance of the rash, but more time may be required. Going forward with elective surgery after an Mpox infection should occur once all lesions have crusted over, fallen off, and smooth skin appears underneath. This timing will vary between patients. Delaying elective surgery for patients with Mpox is important to decrease the risk of Mpox transmission, but this may be challenging since the duration of the infectious period, including the incubation period and the time until the rash resolves, is variable. Patient with active lesions and rashes consistent with Mpox should not undergo elective surgery.
Let’s look a little closer at the preoperative period. If there is a concern for Mpox infection during the preoperative exam, it is important to take the necessary steps to decrease the risk of transmission including wearing appropriate personal protective equipment. Healthcare professionals should not attach social stigmas with Mpox infections. Patients may report unexplained rectal or genital pain or perioral sores that should prompt screening for Mpox exposure or risk factors. Screening tools may be implemented into the electronic health record to help with perioperative screening. Check out Table 1 in the article for clinical questions that can help guide screening and perioperative decision-making with patients suspected to have Mpox.
Here are some questions that you can ask:
- Does the patient have a current or recent history of fevers, chills, malaise, headache, lymphadenopathy, flu-like symptoms?
- Does the patient have a current or recent rash?
- Where is the rash located?
- What is the rash appearance?
- Is the rash attributable to another known etiology?
- Has the patient had recent contact with a known or suspected Mpox case?
- Has the patient recently participated in large parties and gatherings involving intimate sexual contact?
- What is the current epidemiology (incidence and prevalence) of Mpox in the region?
We are going to discuss the considerations for Mpox testing next. Check out the current recommendations from the Centers for Disease Control and Prevention website and I will include this link in the show notes as well. Testing involves the use of polymerase chain reaction assays from DNA sampled from the lesions. Routine preoperative testing is not recommended. Since Mpox does not stay in the blood for very long, blood sample testing is not recommended. In addition, the test results may take several days to return. If you are in the operating room providing care for a patient and there is a concern for an Mpox infection, it is important to contact your local infection control officer or an infectious disease specialist at your institution in order to limit further exposures and determine the exposure risk for health care workers on the care team. There is postexposure vaccination for prophylaxis available which should be administered within 4 days of exposure to help prevent disease. If the vaccination is administered between 4 and 14 days after exposure, there may be some benefit, but it likely be less effective.
Let’s continue our discussion by moving into the operating room and talking about how to decrease the risk of transmission when providing anesthesia care for a patient with Mpox. This virus is a large virus that spreads from lesions and virus on the skin that remain infectious on surfaces for a long time without appropriate disinfection. One study found Mpox virus to still be viable on a household surface 15 days after contact with the infected individual. Transmission may occur when clothing, bedding, or other fabric including the non-invasive blood pressure cuff, is moved. In addition, Mpox virus was found in the air during bed linen changes. Here are the key intraoperative considerations:
- Avoid frequent and rapid removal of the blood pressure cuff since this can spread the virus.
- All fabric that was in contact with the patient should be discarded in sealed waste bags to prevent aerosolization of the viral particles.
- Provide care in a negative pressure room for any aerosol generating procedures
- Full droplet precaution PPE with an N95 or power air purifying respirator, eyewear, and removeable gown and gloves when providing care for patients with Mpox.
- Remove unnecessary equipment from the OR during the procedure.
- Limit OR traffic during the procedure.
- Avoid multiple anesthetics in the same room.
- Continue to follow evidence-based anesthesia work area infection control measures such as frequent hand hygiene and postinduction environmental cleaning.
- Use of United States Environmental Protection Agency (EPA)-registered disinfectants can be used to inactivate the virus. These may include cleaning solutions with active ingredients of isopropyl alcohol, quaternary ammonium, or ethyl alcohol. I will include a link to a list of recommended disinfection products found on the EPA website in the show notes.
Now, that we have made it out of the OR and into the postoperative period, we still need to remain vigilant to provide safe anesthesia care while minimizing patient transport and movement of infected patients and any exposed health care providers across the health care system. Consider expedited dismissal from the OR when applicable or consideration for recovery in the OR with the anesthesia team prior to discharge to an isolation room. Patients with Mpox who must undergo emergency surgery may require postoperative ICU admission and hospitalization with appropriate isolation and health care providers utilizing full PPE. If members of the health care team have unprotected exposure, they may require up to three weeks of isolation and if lesions develop then the duration of isolation will extend until they are no longer infectious.
As we wrap up for today, the authors provide a call to action in conclusion that I will read now:
“Patients presenting with Mpox and/or exposure present unique perioperative considerations. Anesthesia care team providers can leverage current knowledge and pragmatic approaches for infection prevention and control to optimize perioperative patient and provider safety.”
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
For more great anesthesia patient safety content, we hope that you will
Check out the newest February APSF Newsletter
Share the Anesthesia Patient Safety Podcast with your colleagues and catch up on any missed episodes
Consider donating to the APSF and supporting our mission
And connect with us on Twitter by following us @APSForg. We can’t wait to hear from you.
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2023, The Anesthesia Patient Safety Foundation