Episode #137 The Debate Continues: General Endotracheal Anesthesia for ERCP
February 14, 2023Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
We are returning to the October 2022 APSF Newsletter for our featured article today, “Pro-Con Debate: Monitored Anesthesia Care Versus General Endotracheal Anesthesia for Endoscopic Retrograde Cholangiopancreatography” by Luke Janik, Samantha Stamper, Jeffrey Vender, and Christopher Troianos.
Check out the Article of the Month June 2022 Podcast by Anesthesia and Analgesia Editorial Board with interviewer Richard Prielipp and guests Luke Janik and Samantha Stamper. We are so excited to hear some of the A&A podcast clips featuring Luke Janik on the show today.
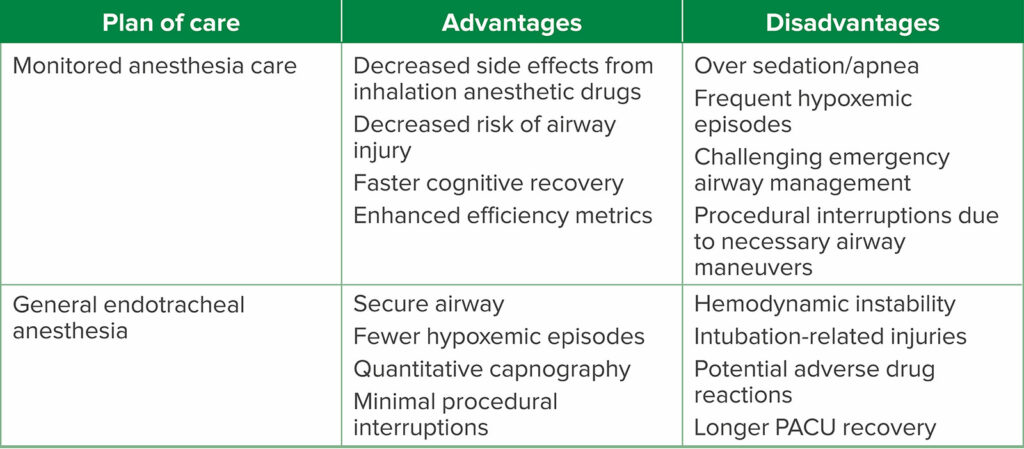
Check out Table 2 from the article.
Table 2: Advantages and Disadvantages of Each Anesthetic Plan of Care.
Here is the citation for the study that we talked about on the show today in support of general endotracheal anesthesia for ERCP.
- Smith ZL, Mullady DK, Lang GD, et al. A randomized controlled trial evaluating general endotracheal anesthesia versus monitored anesthesia care and the incidence of sedation-related adverse events during ERCP in high-risk patients. Gastrointest Endosc. 2019;89:855–862. PMID: 30217726.
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2023, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. We are back for the conclusion of our Pro-Con Debate on anesthesia care for ERCP to discuss final arguments in favor of general endotracheal anesthesia for ERCP. Check out episodes 134 and 135 which offered support for monitored anesthesia care for ERCP and episode 136 which provided the opening arguments for general endotracheal anesthesia for ERCP. Are you team MAC or team GA?
Before we dive into the episode today, we’d like to recognize Preferred Physicians Medical Risk Retention Group, a major corporate supporter of APSF. Preferred Physicians Medical Risk Retention Group has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Preferred Physicians Medical Risk Retention Group – we wouldn’t be able to do all that we do without you!”
We are returning to the October 2022 APSF Newsletter for our featured article today, “Pro-Con Debate: Monitored Anesthesia Care Versus General Endotracheal Anesthesia for Endoscopic Retrograde Cholangiopancreatography” by Luke Janik, Samantha Stamper, Jeffrey Vender, and Christopher Troianos. To follow along with us, head over to APSF.org and click on the Newsletter heading. Fifth one down is the Newsletter archives. Scroll down until you get to October 2022 and then scroll down until you get to our featured article today. I will include a link in the show notes as well.
This article is a reprint from Anesthesia and Analgesia from June 2022 with permission from the International Anesthesia Research Society. This article was also featured on the Article of the Month June 2022 Podcast by Anesthesia and Analgesia Editorial Board with interviewer Richard Prielipp and guests Luke Janik and Samantha Stamper. We are so excited to hear some of the A&A podcast clips featuring Luke Janik on the show today. I will include a link to this podcast episode in the show notes and we hope that you will check out the full Article of the Month June 2022 Podcast too.
Let’s take a listen as Luke Janik makes a strong case for the use of general endotracheal anesthesia for ERCP.
[Janik] “ In this Pro-Con debate, I argued in favor of using general anesthesia with endotracheal intubation. For ERCPs. I’m biased because this is my personal practice and it’s also the practice of my department. The use of the prone position during ERPC plays a huge role in my decision to intubate if a sedated patient in the prone position has laryngospasm vomit.
Aspiration, hypoxia, or any other issue that warrants emergent airway management. The very last thing I want to be doing is trying to urgently flip that patient back supine. Think about it. You have to call for the stretcher, wait for it to be brought into the room, organize the lines in the tubes, gather up the manpower for the flip, and then turn the patient all while trying to handle the ongoing emergency. When every second counts. You don’t want to lose that valuable time.
Now. I will say that the prone position in and of itself is not an absolute contraindication for IV sedation. In fact, I routinely do small mass excisions, hemorrhoidectomies, and other minor surgeries in the prone position while under sedation if the patient has a reassuring airway exam and a reassuring body habitus.
But, the environment you practice in shapes your decisions. And when we’re talking about ERCPs, we’re talking about a prone case involving a shared airway in an offsite location with limited resources. And I think in this situation, intubation is the most logical choice.
The reality is that there’s risk with every type of anesthetic, including general anesthesia with endotracheal intubation, and the risks of general anesthesia in the endoscopy suite are similar to the risks of general anesthesia in the operating room, including the potential for difficult mask ventilation, difficult intubation,, dental injury, aspiration risk, hemodynamic instability, post-op, nausea of vomiting, and the list goes on and on. The fact is there’s really no such thing as a full-proof anesthetic, even if you intubate a patient for ERCP, there’s still a potential that the tube could become dislodged, resulting in a lost airway.
So, the most important thing that we as anesthesia professionals can do is to recognize these risks and be prepared to deal with them in a timely manner. Now, regarding that, surgeons and endoscopists are often quick to point out that sedation is faster than general anesthesia. I’m not sure if this is necessarily true.
The data is mixed. Any time saved by quick turnover using IV sedation may actually be lost by the need for frequent interruptions to the procedure for airway management and management of hypoxic. I must say when I hear surgeons and endoscopists talk about efficiency and timing, they’re very quick to discuss anesthesia efficiency, but rarely ever do I hear them discuss the efficiency of the endoscopists, so the jury is still out on whether IV sedation is really more efficient than general anesthesia for ERCPs.
This was a really fun pro-con debate to have. Thanks for having me on the podcast. The beauty of a pro-con debate is that there is no right answer. It’s controversial by nature. The standard of care is not defined. So my take home point for the listener is that whether you choose general anesthesia, or whether you choose Ivy’s sedation for ERCPs.
Be sure to take into consideration the entire picture. Think about the environment that you’re in, the resources that are available to you, the equipment at your disposal, the patient characteristics, and the specifics of the procedure itself. Remember, by failing to prepare, you are preparing to. Thanks again.
It’s been a lot of fun.”
[Bechtel] “Thank you so much to Janik and A&A for contributing to the show today. Now, its time to get back into the article right where we left off last week. We left off with a call to action by the authors that “normalizing and accepting high rates of hypoxemia during MAC for ERCP, while in a remote location, in the prone position, and with limited airway access sets a dangerous precedent.” There is a real threat to patient safety from sedation-related adverse events during ERCP. Anesthesia professionals must remain vigilant and may need to consider general endotracheal anesthesia. There is evidence to support this practice as well.
Remember, the evidence for MAC instead of GA used retrospective and prospective studies for evidence, but the evidence in support of general anesthesia comes from a randomized controlled study. This is the 2019 study by Smith and colleagues that included patients at high risk for sedation-related adverse events undergoing ERCP who were randomized to receive either general endotracheal anesthesia or propofol-based monitored anesthesia care. Patients with the following risk factors were included STOP-BANG score greater than or equal to 3, abdominal ascites, BMI greater than or equal to 35, chronic lung disease, ASA physical status score greater than 3, Mallampati class 4 airway, and moderate to heavy alcohol use. Exclusion criteria included preceding EUS, emergent ERCP, presence of a tracheostomy, unstable airway, gastric outlet obstruction or delayed gastric emptying, and altered foregut anatomy. Sedation-related adverse event rates were 51.5% compared to 9.9% in the MAC versus GA groups respectively. The GA group had no events of hypoxemia or airway maneuvers compared to 19% of patients in the MAC group developing oxygen saturation below 90% and 45% requiring one or more airway maneuvers and 8% requiring bag-mask ventilation. 10% of the MAC ERCP procedures required interruption with conversion to GA and intubation for respiratory instability in 8% and retained gastric contents in 2%. The rates of vasopressor administration for hypotension occurred at similar rates for both groups. For efficiency metrics, there were no difference in procedure time, technical success, and patient recovery time. I will include this citation in the show notes as well. The data supports GA for ERCP. For many anesthesia professionals this likely makes sense since general anesthesia and intubation provides a secure airway and a controlled environment while helping to avoid preventable hypoxemic events and the risk for respiratory arrest.
Communication and team work with the gastroenterologist during ERCP is imperative. These physicians may think that MAC is more efficient than GA, requires less turnover time, and allows for more procedures to be completed each day. Keep in mind that any time saved by performing sedation will be lost during interruptions for airway maneuvers or conversion to GA. In addition, the efficiency of the GI suite depends on many different patient, personnel, and institution-related factors not just the type of anesthesia care. There are important risks to consider while providing general endotracheal anesthesia including potential for dental injury or trauma, residual neuromuscular blockade, hemodynamic instability, and adverse drug reactions, but MAC is not always the safer option especially for patients in the prone position. Since anesthesia professionals are tasked with keeping patients safe, the authors argue that due to the high risk for airway compromise, it may not be acceptable to provide MAC for ERCP.
Going forward, we need more evidence from large scale, multi-centered randomized controlled trials to help define the standard of anesthesia care for ERCP. At this time, both sides of the debate acknowledge that the first step to keeping patients safe is to make sure that a qualified anesthesia professional is providing the care.
Endoscopist led sedation for ERCP decreased from more than 50% of cases in 2005 to about 5% in 2014 in the United States, but this is a more common practice in Europe and other countries. Endoscopist led sedation for ERCP is associated with higher rates of sedation and procedural failure as well as poor patient and endoscopist satisfaction. This is a big threat to patient safety since propofol sedation should only be utilized by a qualified anesthesia professional who can quickly recognize and intervene during airway compromise to manage the airway in an emergency. Gastroenterology physicians, nurses, and techs are not trained to do this.
To conclude on the Con-side of the debate, the authors remind us that MAC during ERCP may compromised patient safety due to the risks for hypoxemia, airway maneuvers, and sedation-related adverse events especially in a remote location. Further, keeping patients safe during ERCP requires a qualified anesthesia professional with consideration for general endotracheal anesthesia over MAC.
We made it to the end of our great debate which is really helpful in the setting of increased demand for anesthesia care for complex endoscopy procedures without a clearly defined standard of anesthesia care based on large randomized controlled trials as well as considerations for a shared airway in patients with multiple comorbidities. Are you team MAC due to the benefits of fewer hemodynamic changes, decreased side effects from inhalational agents, faster cognitive recovery times, and shorter overall procedure time keeping in mind the risks of hypoxemia and airway compromise? Or are you team general endotracheal anesthesia with the benefits of a secured airway in a patient positioned prone in a remote location? Either way, we hope that you are team qualified anesthesia professional to provide the appropriate safe anesthesia care taking into consideration the patient comorbidities and clinical situation.
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
It is February which means it is time for an all new APSF Newsletter. We are looking forward to discussing the new articles on upcoming shows. Let us know if there are any articles that you want to hear about on this show and stay tuned for all new podcast episodes! Plus, you could be an APSF Newsletter author too. The next deadlines is right around the corner so mark your calendars for March 10th for the June issue. Some of the types of articles include case reports, Question and Answer, Letter to the Editor, Rapid Response as well as invited conference reports, editorials, and reviews all with a focus on anesthesia related perioperative patient safety issues. For more information, head over to APSF.org and click on the Newsletter heading. The last one down is guide for authors and I will include a link in the show notes as well.
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2023, The Anesthesia Patient Safety Foundation