Episode #136 The Debate Continues: General Endotracheal Anesthesia for ERCP
February 7, 2023Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
We are returning to the October 2022 APSF Newsletter for our featured article today, “Pro-Con Debate: Monitored Anesthesia Care Versus General Endotracheal Anesthesia for Endoscopic Retrograde Cholangiopancreatography” by Luke Janik, Samantha Stamper, Jeffrey Vender, and Christopher Troianos.
Check out the Article of the Month June 2022 Podcast by Anesthesia and Analgesia Editorial Board with interviewer Richard Prielipp and guests Luke Janik and Samantha Stamper. We are so excited to hear some of the A&A podcast clips featuring Luke Janik on the show today.
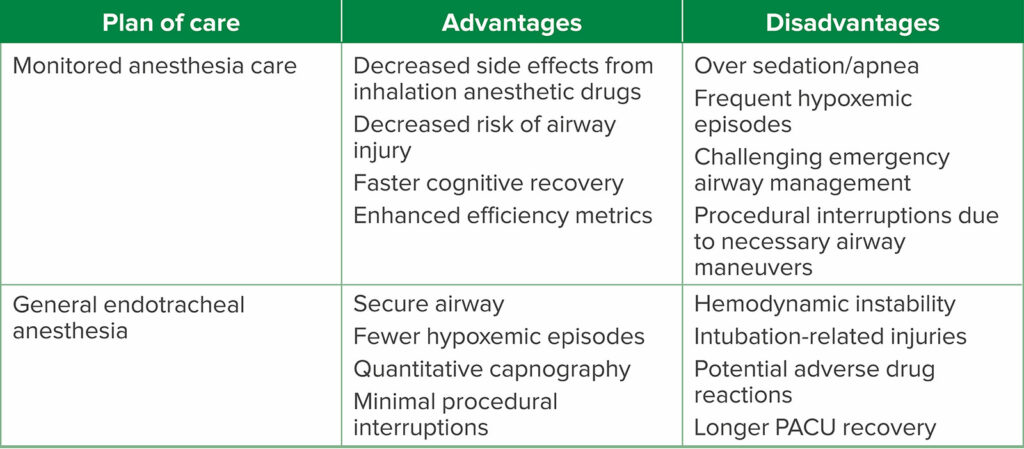
Here are the key considerations for MAC and GEA for ERCP from the article.
Table 2: Advantages and Disadvantages of Each Anesthetic Plan of Care.
We review the following article on the show today to discuss the risks associated with MAC for ERCP.
- Berzin TM, Sanaka S, Barnett SR, et al. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011;73:710–717. PMID: 21316669.
- Zhang CC, Ganion N, Knebel P, et al. Sedation-related complications during anesthesiologist-administered sedation for endoscopic retrograde cholangiopancreatography: a prospective study. BMC Anesthesiol. 2020;20:131. PMID: 32466744.
- Yang JF, Farooq P, Zwilling K, et al. Efficacy and safety of propofol-mediated sedation for outpatient endoscopic retrograde cholangiopancreatography (ERCP). Dig Dis Sci. 2016;61:1686–1691. PMID: 26825844.
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2023, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. This week, we are exploring the other side of the debate, arguments in favor of general endotracheal anesthesia for ERCP. We hope you listened to Episodes 134 and 135 which offered support for monitored anesthesia care for ERCP. If not, make sure you check it out because we are switching gears to talk about general anesthesia today.
Before we dive into the episode today, we’d like to recognize Medtronic, a major corporate supporter of APSF. Medtronic has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Medtronic – we wouldn’t be able to do all that we do without you!”
We are returning to the October 2022 APSF Newsletter for our featured article today, “Pro-Con Debate: Monitored Anesthesia Care Versus General Endotracheal Anesthesia for Endoscopic Retrograde Cholangiopancreatography” by Luke Janik, Samantha Stamper, Jeffrey Vender, and Christopher Troianos. To follow along with us, head over to APSF.org and click on the Newsletter heading. First one down is the Current Issue, October 2022 and then scroll down until you get to our featured article today. I will include a link in the show notes as well.
This article is a reprint from Anesthesia and Analgesia from June 2022 with permission from the International Anesthesia Research Society. This article was also featured on the Article of the Month June 2022 Podcast by Anesthesia and Analgesia Editorial Board with interviewer Richard Prielipp and guests Luke Janik and Samantha Stamper. We are so excited to hear some of the A&A podcast clips featuring Luke Janik on the show today. I will include a link to this podcast episode in the show notes and we hope that you will check out the full Article of the Month June 2022 Podcast too.
We are so excited to return to this article. For the last two weeks, we discussed the pro-side of the debate featuring arguments in favor of monitored anesthesia care for ERCP as well as the advantages and disadvantages of MAC for ERCP.
Today, we are exploring the Con-side of the debate, “GEA offers major advantages over MAC.” To start the show today, let’s check out Table 1 in the article and review the arguments in favor of general endotracheal anesthesia. Here we go.
- MAC is associated with unacceptably high rates of sedation-related adverse events at 20%, conversion to general endotracheal anesthesia at 3%, and hypoxemic episodes at 10-30%.
- The only randomized controlled trial to date comparing general endotracheal anesthesia to MAC in high risk patients demonstrated significantly higher rates of adverse events in the MAC cohort
- NORA carries inherent risk, often related to impaired oxygenation and/or ventilation and general endotracheal anesthesia provides a definitive airway
- While MAC may be feasible for healthy, nonobese patients in reality these patients are few and far between. Patients presenting for ERCP are typically ill, often obese, and usually have multiple risk factors for sedation-related adverse events.
- Efficiency metrics are unlikely to be improved by MAC since the time saved is likely offset by interruptions for necessary airway interventions.
Now, that we have heard the arguments, let’s hear from one of the authors, Luke Janik.
[Janik] “ Let me start by thanking and for having me on the podcast. I think this is a great topic to discuss. For years, sedation in the endoscopy suite was administered by the GI team without anesthesia professionals. So we have to ask what’s changed? Well, first of all, there’s been a big push in medicine towards minimally invasive means of diagnosis and treatment.
So part of what we’re seeing is related to the sheer volume of endoscopy cases. That are being performed. In addition, the patients that are coming through the GI suite are older, sicker, and more obese. But more importantly, I think what we’re seeing is that the value of having an anesthesia professional administering the sedation is becoming widely recognized when the GI team administers sedation without anesthesia profess.
They typically use a combination of fentanyl and midazolam titrated to effect, but this doesn’t always work out well. In fact, if you look at the data, there’s pretty good evidence that endoscopists directed sedation has higher rates of adverse events than sedation administered by an anesthesia professional and is more likely to require an unplanned inter.
Such as mask, ventilation, or intubation. The data also suggests that endoscopist directive sedation results in a higher rate of sedation, failure with poor patient satisfaction, as well as poor endoscopist satisfaction. So I really think we’ve reached the point where, GI physicians, GI nurses, and even hospital administrators have recognized the challenges that come with sedation for endoscopy and have largely embraced having an anesthesia professional provide the sedation.
Offsite anesthesia is really hard and it introduces many challenges. You’re far away from additional help and equipment. You’re in an unfamiliar environment with poor ergonomics. You may have decreased staffing such as anesthesia techs and nurses, and there are variable cultures of safety in each location at each.
The reality is it’s a very different environment than the operating rooms and any anesthesia professional who spent any time in a non-operating room. Anesthesia location knows exactly what I’m talking about. We’ve all been in the position where we can barely reach our equipment. We have to climb or jump over obstacles to get what we need.
We have to strain to see our monitors. We don’t have easy access to the patient and their airway, and our necessary equipment is just out of arm’s reach. And even though we have to laugh, Sometimes it feels as though these rooms were specifically designed to be as cumbersome and ergonomically inefficient as possible.
But when a problem starts to develop in an offsite location and you feel like you’re on an island, Everyone else in the room may be completely oblivious to what’s going on with the patient. They may be talking about sporting events and their favorite TV shows while you’re trying to rescue the patient, and so there’s a different atmosphere to being in an offsite location than being in an operating room.
And while each hospital is different, and some may have better offsite locations than others, the reality is anesthesia professionals will never feel quite as comfortable in offsite locations as they do in the operating room because they just don’t have the same, uh, attention to detail and resources that, uh, exist in the operating rooms.”
[Bechtel] What a great way to open the show! Thank you to A&A and Luke Janik for the clips. Now, let’s get into the article. Have you provided anesthesia care for an ERCP today, or this week, or this month? You may have since there are over 500,000 ERCP procedures performed yearly in the United States for the management of liver, biliary, and pancreatic disease and most commonly for bile duct stones and strictures of the biliary and pancreatic ductal systems. In the endoscopy suite, ERCP may be considered the highest risk procedure with the following procedural complications: pancreatitis, cholangitis/sepsis, post-sphincterotomy bleeding, duodenal perforation, and death. And let’s not forget the complications related to anesthesia care since there is a high rate of sedation-related adverse events during the procedure with an incidence of about 21%. How do we keep patients safe during anesthesia care for ERCP procedures? Safe anesthesia care should involve a qualified anesthesia professional providing the anesthesia for ERCP with general endotracheal anesthesia.
Let’s dig a little deeper into the options for anesthesia care for ERCP. These include endoscopist-directed sedation, MAC, and general endotracheal anesthesia. For endoscopist-directed sedation, a member of the GI team, usually a nurse, provides IV sedation with supervision by the endoscopist performing the procedure. In the past, conscious sedation with benzodiazepines and narcotics was used with high procedure failure rates, poor patient satisfaction and poor endoscopist satisfaction. Now, propofol sedation may be provided by non-anesthesia professionals with support from gastroenterology as safe and effective. For the MAC and GA options, an anesthesia professional is responsible for providing the anesthesia care while the endoscopist performs the procedure. Important considerations for the model of anesthesia care include available resources and personnel, procedural complexity, patient characteristics and comorbidities, and individual preferences.
One of the most important considerations is the location of the endoscopy suite in a NORA location that may be remote from the operating rooms. There are higher rates of severe complications including death and permanent brain damage in NORA locations than in adverse events that take place in the operating room. There is no time to let down our guard in the endoscopy suite especially during ERCP procedures. Closed claims data focusing on the GI suite reveal the highest percentage of anesthesia malpractice claims, the highest proportion of claims associated with oversedation, and the highest rate of MAC utilization. Challenges that anesthesia professionals face in the GI suite include older patients, often with significant comorbidities and unfamiliar locations, lack of resources, poor ergonomics, limited assistance, variable cultures of safety, and physical distance from addition anesthesia equipment and team members. Safe and effective anesthesia care for ERCP must take into considerations patient positioning prone or semi-prone, limited access to the airway, and use of the endoscope which may contribute to airway obstruction and laryngospasm.
It’s time to dive in to the data. First up, the 2011 prospective study by Berzin and colleagues of patients undergoing ERCP that revealed an overall rate of sedation-related adverse events of 21%. In the MAC patients, adverse events included hypoxemia with oxygen saturation less than 85% at 12.5%, unplanned mask ventilation at 0.6%, unplanned intubation at 3%, and procedural interruption at 5%. The authors conclude that while there were frequent sedation related events, procedural interruption did not occur often. It is important to note that for the 3% of patients who required unplanned intubation, the authors noted that airway access was easily obtained. Our next study is another prospective study from 2020 by Zhang and colleagues which revealed that sedation-related adverse events occurred in 18% of patients undergoing MAC for ERCP with 9% of patients developing hypoxemia and more than 33% of patients having multiple hypoxemic episodes. Even with these findings, the authors concluded that sedation delivered by anesthesia professionals was safe for ERCP. Over 3000 patients that underwent MAC for ERCP were studied in the retrospective study by Yang and colleagues which found an incidence of hypoxemia requiring airway manipulation of 28% with 1.6% of patients needing conversion to GA with an endotracheal tube for airway protection from food in the stomach. Once again, the conclusion was similar – sedation with propofol is safe for patients undergoing ERCP.
You may be asking yourself, “Is sedation for ERCP safe, feasible, or appropriate given the results of these studies?” It is quite concerning that up to one third of patients may develop hypoxemia and there is an unplanned intubation rate of up to 3% even if there are no long-term effects or more serious complications. These hypoxemic events may all be considered “near-miss” events. Without appropriate, rapid, and effective interventions, patients are at risk for significant morbidity and mortality. Keeping patients safe during ERCP requires using appropriate monitoring which must include pulse oximetry for oxygenation as well as capnography for ventilation to be able to detect hypoventilation and hypercarbia. Remember, once patients develop hypoxemia while receiving supplemental oxygen, there will already be significant hypoventilation and patients are at risk for further deterioration and respiratory arrest.
We still have more to talk about when it comes to providing safe anesthesia care for patients undergoing ERCP. Today, we have presented evidence about the risks of MAC for ERCP. We hope that you will tune in next week for our review of the benefits of general endotracheal anesthesia for ERCP. Plus, we will be hearing from Janik once again. The debate continues.
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
It is February which means it is time for an all new APSF Newsletter. We are looking forward to discussing the new articles on upcoming shows. Plus, you could be an APSF Newsletter author too. The APSF Newsletter is the official journal of the Anesthesia Patient Safety Foundation with an audience that includes anesthesia professionals, perioperative providers, key industry representatives, and risk managers. The next deadlines is right around the corner so mark your calendars for March 10th for the June issue. Some of the types of articles include case reports, Question and Answer, Letter to the Editor, Rapid Response as well as invited conference reports, editorials, and reviews all with a focus on anesthesia related perioperative patient safety issues. For more information, head over to APSF.org and click on the Newsletter heading. The last one down is guide for authors and I will include a link in the show notes as well. Plus, make sure that you click on the Subscribe via email heading as well and sign up to be on the APSF Newsletter email list so that you can get expedited access by email to our current APSF Newsletter issue.
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2023, The Anesthesia Patient Safety Foundation