Episode #133 Perioperative Considerations for Methylene Blue Administration and Serotonin Toxicity
January 17, 2023Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
Thank you for joining us for an article from our archives show.
Our featured article is from the June 2015 APSF Newsletter. It is “Methylene Blue and the Risk of Serotonin Toxicity” by Adair Locke.
Check out Figure 1 in the article. It is a visual representation of the Serotonin Toxicity Triangle which depicts the interactions between the different classes of serotonergic drugs that may produce serious serotonin toxicity.
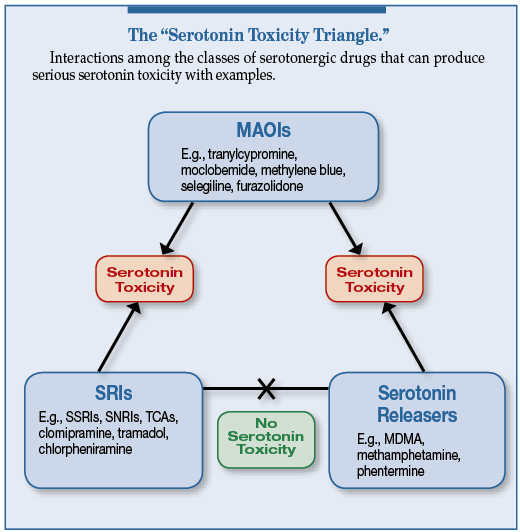
Figure 1. Classes of serotonergic drugs that can produce severe serotonin toxicity with examples (not an exhaustive list). SRI, serotonin reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressants. Source: Modified from Stanford et al.5,6,9
Table 1. Hunter Serotonin Toxicity Criteria
In the presence of a serotonergic agent, serotonin toxicity is established at a high confidence level if any one of the 5 conditions below are present:
| 1) | Spontaneous clonus |
| 2) | Tremor AND hyperreflexia |
| 3) | Inducible clonus AND agitation OR diaphoresis |
| 4) | Ocular clonus AND agitation OR diaphoresis |
| 5) | Hypertonicity AND temperature > 38° C AND Inducible clonus OR ocular clonus
From Ng et al.3 |
Once the diagnosis is confirmed, do not delay starting treatment. Treatment for Serotonin Toxicity involves the following:
- Immediate discontinuation of serotonergic drugs
- Supportive therapy
- Sedation with benzodiazepines
- Cooling therapy for hyperthermia if needed.
- Administration of serotonin receptor antagonists for moderate and severe toxicity. These medications include cyproheptadine, chlorpromazine, and the more potent olanzapine and ketanserin.
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2023, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. We hope that you are looking forward to the next APSF Newsletter publication in February, but until then, there is still so much more to talk about related to anesthesia patient safety. We are cracking open the APSF archives for our show today. For this episode and future similar shows, we will take a look at past articles that were published in the APSF Newsletter that you can find on our website. Keep in mind that things may have changed since the publication of these articles, but they are of interest from our archives.
Before we dive into the episode today, we’d like to recognize Edwards Lifesciences, a major corporate supporter of APSF. Edwards Lifesciences has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, Edwards Lifesciences – we wouldn’t be able to do all that we do without you!”
Have you ever administered Methylene Blue? Do you routinely administer this medication as part of your practice? That is the focus for our show today. Even if methylene blue administration is not part of your routine practice, we are going to be talking about Serotonin Syndrome. This is an important patient safety consideration since there are several serotonergic drugs that can cause serotonin syndrome depending on the interactions. Our featured article is from the June 2015 APSF Newsletter. It is “Methylene Blue and the Risk of Serotonin Toxicity” by Adair Locke. To follow along with us, head over to APSF.org and click on the newsletter heading. Fifth one down is Newsletter archives. Then, scroll down until you get to June 2015. The second article down is our featured article today. Don’t worry, I will include a link in the show notes as well.
Let’s start off by talking about Methylene Blue. This is an intravenous medication that has a similar structure to tricyclic antidepressant medications and acts as a potent monoamine oxidase inhibitor, especially MAO-A as well as on the nitric oxide cyclic GMP pathway. It is used as a marker dye during urologic procedures with increased use during periods of indigo carmine shortages. It is also used for treatment of hypotensive shock, vasoplegic syndrome, ifosfamide-induced encephalopathy, and methemoglobinemia. Methylene blue infusion is also used to localize parathyroid tissue during parathyroidectomy procedures. Intravenous administration is rapidly absorbed in nervous tissue and is present in high concentrations in brain tissue in rat models. All by itself, methylene blue administration is not associated with a high risk for serotonin toxicity. Be on the lookout for methylene blue administration in combination with other serotonergic agents which may lead to serotonin toxicity in the perioperative period.
Check out Figure 1 in the article. It is a visual representation of the Serotonin Toxicity Triangle which depicts the interactions between the different classes of serotonergic drugs that may produce serious serotonin toxicity. At the top of the triangle is the drug class, MAOIs, which includes methylene blue. MAOIs may interact with Serotonin reuptake inhibitors including Selective Serotonin Reuptake Inhibitors, Serotonin and Norepinephrine Reuptake Inhibitors and Tricyclic antidepressants and Serotonin Releasers to cause serotonin toxicity. The combination of serotonin reuptake inhibitors and serotonin releasers are less likely to cause serotonin toxicity. I will include the image in the show notes as well.
Use of methylene blue as a marker dye increased in 2015 due to a nationwide shortage of indigo carmine in the United States from manufacturing delays and a shortage of raw materials. Indigo carmine is well tolerated with side effects of an idiosyncratic drug reaction or mild vasopressor effect. It is used as a marker dye to confirm ureteral patency and to localize ureteral orifices, for lymph node and vessel delineation, and for tumor localization. If there is difficulty obtaining indigo carmine at your institution, you may need to use methylene blue.
Now, let’s review some of the serotonergic medications that you may see on a patient’s list of home medications:
- Selective serotonin reuptake inhibitors including fluoxetine, paroxetine, and escitalopram
- Serotonin-norepinephrine reuptake inhibitors including venlafaxine and duloxetine
- Tricyclic antidepressants including amitriptyline and clomipramine
Keep in mind that many common perioperative medications are weak serotonin reuptake inhibitors including the following:
- intravenous fentanyl
- transdermal fentanyl patch
- meperidine
- tramadol
- and methadone
The combination of these medications with other serotonergic medications and/or methylene blue has been associated with serotonin syndrome. We have talked about a lot of serotonergic medications on the show so far today, but if you want a complete list, I will include a link to the 2017 FDA Drug Safety Communication with updated information about the interaction between methylene blue and serotonergic medications. We hope that you will check it out after the show. It is important to review patient’s home medications carefully and be on the lookout for these serotonergic medications prior to administration of methylene blue.
Serotonin toxicity occurs when there are too high levels of synaptic serotonin. The degree of the toxicity depends on the concentration of serotonin in the synaptic spaces in nervous tissue. This concept helps to explain the following drug interactions.
- Serotonin releasers such as methamphetamine and serotonin reuptake inhibitors combined with MAO inhibitors may cause severe serotonin toxicity.
- Selective and non-selective serotonin reuptake inhibitors prevent clearance of serotonin from the intraneuronal synaptic space. MAO inhibitors prevent intraneural metabolism of serotonin leading to increased release of serotonin from neurons. This combination of mechanisms of action is what can cause severe serotonin toxicity in the setting of normal SRI dosing combined with a single administration of methylene blue leading to increased serotonin release and reduced synaptic serotonin clearance.
It’s time for us to dive into the literature to learn more about methylene blue and serotonin toxicity. We can’t go back too far through since this association has only been written about over the past 15-20 years. In 2006 and 2007, there were two surgical case series that described methylene blue associated CNS toxicity in patients who received intraoperative methylene blue. All of the patients who developed toxicity were taking serotonin reuptake inhibitors prior to surgery, but not all of the patients who were taking SRI ended up developing the clinical picture of CNS toxicity. By 2015, in the literature, there were 14 individual published case reports of likely or definite serotonin toxicity in patients taking SRIs who received methylene blue. In one of these cases, the outcome was fatal. In 2006, researchers Gillman and Ramsay performed in vitro studies and were the first to demonstrate that methylene blue acted as a highly potent reversible MAO-A inhibitor at nanomolar concentrations. Additional research revealed that even low dose methylene blue, less than 1mg per kg, could produce clinically significant MAO inhibition. By July 2011, following multiple reports of adverse perioperative events involving methylene blue administration, the FDA published a safety announcement which cautioned about the risk of central nervous syndrome dysfunction following methylene blue administration in patients taking serotonergic psychiatric medications. The resultant serotonin toxicity depends on the mechanism of action of the medications and ultimately the degree to which serotonin levels are increased. Let’s take a look at tricyclic antidepressant medications which have the combined actions of serotonin reuptake inhibition and norepinephrine reuptake inhibition. Clomipramine is the most potent at serotonin reuptake inhibition and would be the most likely to cause serotonin toxicity when combined with methylene blue administration. On the other hand, desipramine has very little serotonin activity and would be less likely to cause toxicity. Other antidepressants including mirtazapine and trazodone have little serotonin activity as well. However, the FDA warning was extended to all serotonergic drugs with the recommendation for discontinuation if methylene blue administration is anticipated in the perioperative period to help keep patients safe from developing toxicity.
We have been talking about serotonin syndrome and serotonin toxicity a lot today, but what does this look like clinically? The Hunter Serotonin Toxicity Criteria can be used to help with the diagnosis. If any one of the following 5 criteria are present in a patient who received a serotonergic agent, then there is a high confidence level for serotonin toxicity. Here are the conditions:
- Spontaneous clonus
- Tremor AND hyperreflexia
- Inducible clonus AND agitation OR diaphoresis
- Ocular clonus AND agitation OR diaphoresis
- Hypertonicity AND temperature > 38° C AND Inducible clonus OR ocular clonus
Remember, this syndrome is associated with significant morbidity and mortality. Patients may develop altered mental status, autonomic hyperactivity, and neuromuscular abnormalities. Be on the lookout for the following clinical signs. It is important to keep in mind that these clinical signs may be non-specific, and evaluation may be challenging during and after surgery and anesthesia.
- Tremor
- Nervousness
- Agitation
- Mydriasis
- mood dysphoria
- hyperreflexia
- inducible clonus
Severe serotonin toxicity involves the following:
- Confusion
- Muscle rigidity
- Sustained clonus
- Hyperthermia with temperatures greater than 38.5°C.
It is important to keep in mind that these clinical signs may be non-specific. Evaluation may be challenging during and after surgery and anesthesia since benzodiazepines and muscle relaxants can mask symptoms. The differential diagnosis may include postoperative delirium, malignant hyperthermia, anticholinergic crisis, neuroleptic malignant syndrome, acute alcohol withdrawal, and metabolite-mediated opiate toxicity. In the setting of any combination of SRI or other serotonergic agent and methylene blue administration, it is critical to consider serotonin toxicity. The next step is to use the Hunter Serotonin Toxicity Scale and once the diagnosis is confirmed, do not delay with starting treatment. I will include the Hunter Scale in the show notes as well.
Treatment for Serotonin Toxicity involves the following:
- Immediate discontinuation of serotonergic drugs
- Supportive therapy
- Sedation with benzodiazepines
- Cooling therapy for hyperthermia if needed.
- Administration of serotonin receptor antagonists for moderate and severe toxicity. These medications include cyproheptadine, chlorpromazine, and the more potent olanzapine and ketanserin.
Preoperative planning for patients on psychiatric medications is important since discontinuation of their medication may not be feasible. Another option is the use of indocyanine green as a marker dye to identify ureters using near infrared light. Preoperative oral phenazopyridine and vitamin B complex may also be considered as alternatives to methylene blue administration.
If methylene blue may be used during surgery, the suggestion is for discontinuation of the serotonergic psychiatric drug 2 weeks prior to surgery for clearance of the active ingredient and its active metabolites. Fluoxetine or Prozac has an even longer half-life and should be discontinued 5 weeks prior to methylene blue administration. Patients with liver disease may need a longer washout period since many serotonergic drugs undergo hepatic metabolism.
What about life-threatening situations such as vasoplegia with cardiopulmonary bypass, methemoglobinemia, ifosfamide-induced encephalopathy, and cyanide poisoning? If the patient is taking an SRI, can methylene blue be administered? This is the time to weigh the risks and benefits. Methylene blue administration may be considered if the benefits outweigh the risks and patients will need to be monitored carefully for CNS toxicity for 24 hours.
The author leaves us with a call to action that anesthesia professionals must remain knowledgeable about the interaction between methylene blue and other serotonergic medications, stay vigilant for signs of serotonin toxicity, and be ready to provide treatment when necessary.
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
Did you know that you can find us on twitter, Instagram, and Linked In! See the show notes for more details and we can’t wait for you to tag us in a patient safety related tweet or like our next post on Instagram or connect with us on Linked In!! Follow along with us for anesthesia patient safety pictures and stories all week long!!
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2023, The Anesthesia Patient Safety Foundation

