Episode #131 Keeping Patients Safe in the Electrophysiology Lab
January 3, 2023Welcome to the next installment of the Anesthesia Patient Safety podcast hosted by Alli Bechtel. This podcast will be an exciting journey towards improved anesthesia patient safety.
It is our first episode of 2023! Our featured article today is from the February 2022 ASPF Newsletter. It is called “Anesthetic Safety Considerations for Off-site Cardiology Procedures” by Todd Novak and Chelsea Zur.
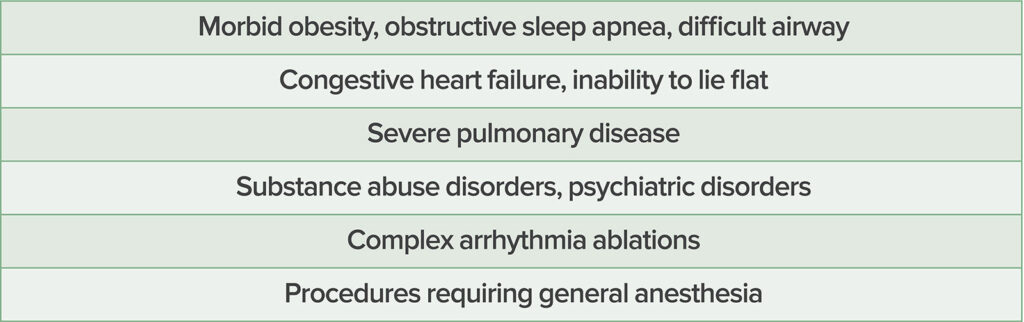
Check out Table 1 in the article for a list of the patients who may need preprocedural evaluation in the preoperative anesthesia clinic.
Table 1: High-Risk Patient Factors That May Warrant Preprocedural Anesthesia Evaluation Prior to Their Off-Site Cardiology Procedure
Check out Table 2 in the article for a review of anesthetic agents and their electrophysiologic effects that may be used for sedation and general anesthesia during EP procedures.
- Sevoflurane will increase the QTc and enhance ectopic atrial rhythms. It has no effect on SA and AV nodes and no effect on accessory pathway. It is considered safe to use.
- Desflurane increases the QTc, has inhibitory effects on the AV node, and causes tachycardia. Considerations for desflurane use include that it is sympathomimetic and possibly arrhythmogenic.
- Propofol effects include the following: inhibitory or no effects on the SA and AV node, no effect on the accessory pathway, and bradycardia. Propofol may not be suitable for ectopic atrial tachycardia ablation and suppresses electrical storm.
- Midazolam effects include possible vagolysis and tachycardia.
- Rocuronium and Vecuronium have minimum effects on automaticity. Keep in mind that neuromuscular blockade should be avoided during phrenic nerve pacing.
- Succinylcholine has inhibitory effects on AV node and tachycardia or bradycardia may be seen following administration.
- Remifentanil has inhibitory effects on the SA and AV nodes and bradycardia may occur. It may not be the optimal medication choice for AVRT and AVNRT ablation in pediatric patients.
- Fentanyl increases vagal tone, but may be used for EP procedures when combined with midazolam.
- Sufentanil increases the QTc interval and has no effect on the accessory pathway.
- Dexmedetomidine enhances vagal activity, decreases norepinephrine release, decreases sympathetic tone, and may cause bradycardia. It is an antiarrhythmic for pediatric patients and may not be appropriate for EP procedures.
- Finally, Ketamine has minimal effects on the SA and AV nodes and increases atrial conduction time. It may cause increased heart rate with possible increased blood pressure as well.
Be sure to check out the APSF website at https://www.apsf.org/
Make sure that you subscribe to our newsletter at https://www.apsf.org/subscribe/
Follow us on Twitter @APSForg
Questions or Comments? Email me at [email protected].
Thank you to our individual supports https://www.apsf.org/product/donation-individual/
Be a part of our first crowdfunding campaign https://www.apsf.org/product/crowdfunding-donation/
Thank you to our corporate supporters https://www.apsf.org/donate/corporate-and-community-donors/
Additional sound effects from: Zapsplat.
© 2023, The Anesthesia Patient Safety Foundation
Hello and welcome back to the Anesthesia Patient Safety Podcast. My name is Alli Bechtel, and I am your host. Thank you for joining us for another show. Happy New Year! It is 2023 and we are so excited that you are joining us to learn more about anesthesia patient safety this year. Let’s start the new year off with a review of important patient safety considerations during off-site cardiology procedures.
Before we dive into the episode today, we’d like to recognize BD, a major corporate supporter of APSF. BD has generously provided unrestricted support to further our vision that “no one shall be harmed by anesthesia care”. Thank you, BD – we wouldn’t be able to do all that we do without you!”
Do you provide anesthesia care for patients undergoing off-site cardiology procedures? Does your anesthesia group provide anesthesia care for patients undergoing EP and interventional cardiology procedures? Go ahead and turn up the volume because here we go. Our featured article today is from the February 2022 ASPF Newsletter. It is called “Anesthetic Safety Considerations for Off-site Cardiology Procedures” by Todd Novak and Chelsea Zur. To follow along with us, head over to APSF.org and click on the Newsletter heading. Fifth one down is newsletter archives. Then click on the February 2022 Newsletter and scroll down until you get to our featured article today. I will include a link in the show notes as well.
Novak and Zur kick off the article by introducing the scope of off-site cardiology procedures. There have been significant advancements in electrophysiology and interventional cardiology which means that there are more complex procedures and more complex patients with multiple co-morbidities that require anesthesia care. Plus, these procedures are often performed off-site and remote from the operating rooms in an environment that may be unfamiliar with limited space and physical barriers between the anesthesia professional and the patient. You may need to work around the fluoroscopic equipment or video screens or even the proceduralist depending on the procedure. There are significant threats to anesthesia patient safety at these locations as evidenced by evidence from the ASA closed claims database. This article helps to further our understanding of the challenges related to providing anesthesia care during these procedures so that we may be prepared to help keep patients safe.
Let’s start at the beginning with the preoperative evaluation. The preoperative evaluation should include the following:
- History and physical exam
- Review of allergies with particular attention to iodinated contrast
- Medication reconciliation with particular attention to anticoagulants and heart failure medications. Keep in mind that for most procedures except ablation procedures beta-blockers and antiplatelet medications are often continued.
For high-risk patients and high-risk procedures, patients may need to be evaluated in a preoperative anesthesia clinic. Check out Table 1 in the article which reveals the high-risk patient factors that may benefit from an appointment in the preoperative anesthesia clinic before their cardiology procedure. Here is the list.
- Morbid obesity, obstructive sleep apnea, and difficult airway
- Congestive heart failure or inability to lie flat
- Severe pulmonary disease
- Substance abuse disorder, psychiatric disorders
- Complex arrhythmia ablations
- Procedures requiring general anesthesia
Most patients undergoing an offsite cardiology procedure are followed by a cardiologist and have had a comprehensive workup prior to the procedure which may include a 12-lead electrocardiogram, echocardiogram, and cardiac monitoring. Patients with a cardiovascular implantable electronic device will need a device interrogation to review the manufacturer, current settings, indication for placement, and dependence on the device. There is no consensus from the most recent 2020 Practice Advisory from the American Society of Anesthesiologists for the preoperative time frame for the device interrogation prior to an elective procedure. The majority of ASA members and consultants recommend interrogation within 3-6 months prior to the planned procedure. The preoperative laboratory evaluation depends on the procedure and bleeding risk and may include a complete blood count, type and screen, coagulation studies, and basic metabolic panel especially if contrast is going to be used during the procedure.
Now that we have completed the preoperative evaluation, let’s head into the electrophysiology lab. There are several ablation techniques that may be used, and it is important to be prepared for complications. The most common complication involves vascular access injuries leading to cardiac perforation and tamponade. If perforation occurs, rapid action is needed with reversal of anticoagulation and pericardiocentesis. Anesthesia professionals must be prepared to act quickly to administer blood products and initiate vasopressor infusions. It is important to have a plan in place for emergent transport to the operating room in case of cardiovascular collapse requiring surgical intervention. Having the logistics figured out ahead of time is critical for unstable patients. Be on the lookout for other complications that may include cerebrovascular accident, heart block, pulmonary edema, phrenic nerve palsy, esophageal perforation, and pulmonary hemorrhage.
Large-bore intravenous access, arterial catheters, and or central lines may be needed depending on the patient and procedure and if needed, will need to be placed prior to the start of the procedure since once the patient is draped, it may be difficult to access the patient in case of emergency. Consideration for arterial line placement may be for patients who may be hemodynamically unstable or for long procedures. The electrophysiologist may obtain arterial access and monitoring from this line is possible, but the waveform may become dampened or be inaccurate if the device occludes that lumen of the arterial sheath. As a result, you may want to consider placing your own invasive blood pressure monitoring line to ensure accurate blood pressure monitoring with arterial blood gas sampling throughout the procedure if needed. Communication with the electrophysiologist prior to the procedure is important to make sure that there is a plan for accurate blood pressure monitoring during the procedure. Providing safe anesthesia care during these procedures also requires navigating around the large pieces of equipment for cardiac mapping and fluoroscopic imaging in the room and surrounding the patient. There is a risk for accidental removal of the endotracheal tube, intravenous lines and monitoring since the operating table and the fluoroscopic C-arm are controlled by the electrophysiologist. One strategy to mitigate this risk is to add extensions to the lines.
Next up, let’s review catheter-based ablations which are used for the treatment of supraventricular tachycardia, atrial flutter, atrial fibrillation, and ventricular tachycardia. The treatment involves creating a transmural lesion that permanently removes the arrhythmogenic cardiac tissue without causing damage to nearby structures. Shorter duration procedures such as for SVT and atrial flutter ablations may be performed with sedation by a qualified nurse under supervision by the electrophysiologist and without an anesthesia professional. For more complex and longer procedures that involve mapping and ablating, anesthesia care may include monitored anesthesia care or general anesthesia with an anesthesia professional. Keep in mind that anesthetic medications may suppress arrhythmia inducibility. This is another time when it is important to communicate with the electrophysiologist and work together to determine an appropriate anesthetic plan.
Table 2 in the article is a great reference to review anesthetic agents and their electrophysiologic effects. We are going to review it now.
- Sevoflurane will increase the QTc and enhance ectopic atrial rhythms. It has no effect on SA and AV nodes and no effect on accessory pathway. It is considered safe to use.
- Desflurane increases the QTc, has inhibitory effects on the AV node, and causes tachycardia. Considerations for desflurane use include that it is sympathomimetic and possibly arrhythmogenic.
- Propofol effects include the following: inhibitory or no effects on the SA and AV node, no effect on the accessory pathway, and bradycardia. Propofol may not be suitable for ectopic atrial tachycardia ablation and suppresses electrical storm.
- Midazolam effects include possible vagolysis and tachycardia.
- Rocuronium and Vecuronium have minimum effects on automaticity. Keep in mind that neuromuscular blockade should be avoided during phrenic nerve pacing.
- Succinylcholine has inhibitory effects on AV node and tachycardia or bradycardia may be seen following administration.
- Remifentanil has inhibitory effects on the SA and AV nodes and bradycardia may occur. It may not be the optimal medication choice for AVRT and AVNRT ablation in pediatric patients.
- Fentanyl increases vagal tone, but may be used for EP procedures when combined with midazolam.
- Sufentanil increases the QTc interval and has no effect on the accessory pathway.
- Dexmedetomidine enhances vagal activity, decreases norepinephrine release, decreases sympathetic tone, and may cause bradycardia. It is an antiarrhythmic for pediatric patients and may not be appropriate for EP procedures.
- Finally, Ketamine has minimal effects on the SA and AV nodes and increases atrial conduction time. It may cause increased heart rate with possible increased blood pressure as well.
Whew, that was quite a list and a great review. Let’s keep the momentum going with another list to review and that is the different types of ablation procedures including radiofrequency ablation, cryoballoon ablation, and epicardial ablation.
First up, radiofrequency ablation is the most widely used technique and may be used for a wide variety of arrhythmias. With this technique, electromagnetic energy is converted to thermal energy leading to irreversible thermal injury to the myocardial tissue. Injury to nearby tissues from high temperatures at the electrode-tissue interface is prevented by active cooling with saline administration at the tip of the catheter. An important safety consideration during AF ablations which involve the left atrium is to place an esophageal temperature probe to continuously monitor temperature and minimize the risk of esophageal injury as well as other nearby structures. The goal is to maintain the temperature below 38.5 degrees Celsius in order to decrease the risk for esophageal ulceration and left atrial-esophageal fistula formation. Monitoring the patient’s fluid status is important as well since several liters of saline may be administered throughout the procedure as part of the active cooling process. Keep an especially close eye on patients with reduced right and left ventricular function.
Next up, we have cryoballoon ablation. This is a newer technique using new technology to freeze the endocardium leading to decreased transmission of the aberrant electrical signals. It is mainly used for AF ablations. During the procedure, a balloon-tipped catheter is placed into a pulmonary vein and when the balloon is inflated, there is circumferential freezing of the surrounding tissue. Phrenic nerve palsy is one of the most common complications following cryoballoon ablation. In order to help keep patients safe, it is important to avoid neuromuscular blockade so that phrenic nerve stimulation can be performed to help avoid this complication.
Finally, we have epicardial ablation which may be used for ventricular arrhythmias and during hybrid surgical-catheter technique for atrial fibrillation. The hybrid approach is a newer technique that involves treatment of the epicardium and the endocardium with combined surgical and catheter-based approaches. Epicardial ablations are performed under general anesthesia. There are several unique complications of this procedure to be on the lookout for and be prepared to treat for including hemopericardium, intra-abdominal bleeding, phrenic nerve injury, coronary artery disruption, and pericarditis. You will need to act quickly to diagnose and treat patients who develop hypotension during the procedure to help keep them safe.
We made it out of the EP lab, and it is time to head into the catheterization laboratory, but you will have to tune in next week for the exciting conclusion. There is still so much more to talk about for keeping patients safe during off-site cardiology procedures.
If you have any questions or comments from today’s show, please email us at [email protected]. Please keep in mind that the information in this show is provided for informational purposes only and does not constitute medical or legal advice. We hope that you will visit APSF.org for detailed information and check out the show notes for links to all the topics we discussed today.
We are looking forward to another great year of APSF newsletters, articles between issues, podcasts, and so much more in 2023 and we hope you will continue to tune in. If you get a chance, we hope that you will share this podcast and the APSF newsletter with any of your friends or colleagues who are interested in anesthesia patient safety. Did you know that you can subscribe to receive the APSF Newsletter by email. This ensures that you receive expedited access by email to our current APSF Newsletter issue. What are you waiting for? Head over to ASPF.org and click on the newsletter heading. The last one down is Subscribe via email. Then, you just need to provide your name and email address before looking forward to receiving our next APSF Newsletter. I will include the link in the show notes as well. Thank you for starting the new year by joining us for this show.
Until next time, stay vigilant so that no one shall be harmed by anesthesia care.
© 2023, The Anesthesia Patient Safety Foundation