Disclaimer: Viewers of this material should review the information contained within it with appropriate medical and legal counsel and make their own determinations as to relevance to their particular practice setting and compliance with state and federal laws and regulations. The APSF has used its best efforts to provide accurate information. However, this material is provided only for informational purposes and does not constitute medical or legal advice. This response also should not be construed as representing APSF endorsement or policy (unless otherwise stated), making clinical recommendations, or substituting for the judgment of a physician and consultation with independent legal counsel.
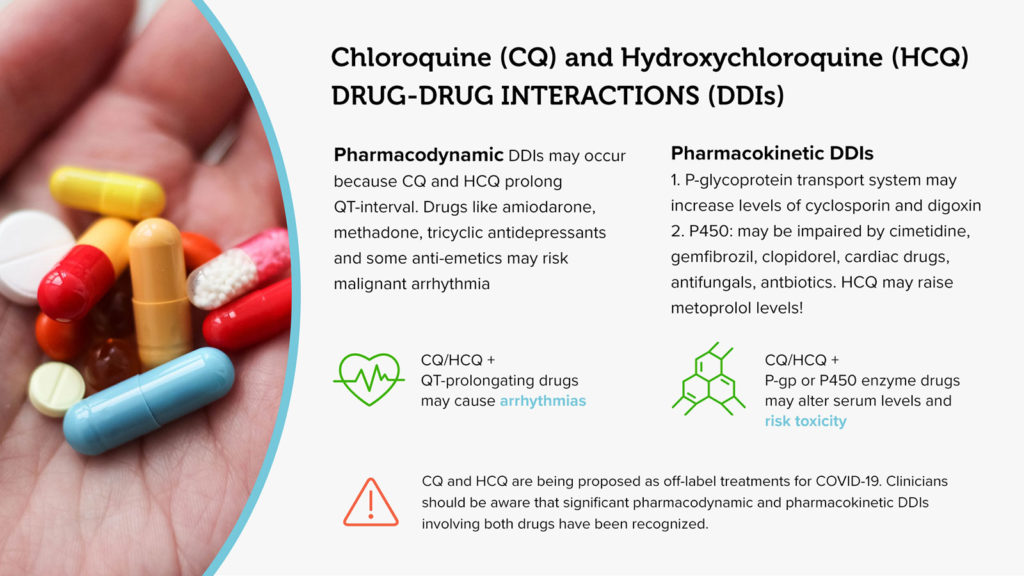
COVID-19 is a rapidly emerging and devastating pandemic disease. Recently, chloroquine (CQ) and hydroxychloroquine (HCQ) have been suggested for possible off-label use for patients suffering from a more severe clinical course. Both drugs have been in widespread use for many years for several indications, including off-label use for rheumatological diseases such as lupus. Their package inserts list a number of drug-drug interactions (DDIs).(1,2) Unfortunately, because the drug sheets pre-date 2002, the drug interaction information is a scattered array of post-marketing reports with little information to elucidate underlying mechanisms. Therefore, without comment on the appropriateness, efficacy, or possible drug dosing regimens of chloroquine and/or hydroxychloroquine therapy for COVID-19, we briefly summarize and provide patient safety information on the clinically relevant CQ/HCQ drug-drug interactions.
- PHARMACODYNAMIC DDIs
In general, pharmacodynamic DDIs occur when there is a synergistic or antagonistic effect of two or more drugs at a specific receptor site. Both CQ/HCQ package inserts list interactions that are attributable to this type of DDI.
- Cardiac and Arrhythmogenic Effects – including QT prolongation, QRS widening, and Negative Inotropy
It is noteworthy that both CQ and HCQ have multiple cardiac effects including meaningful prolongation of the QT interval.(1) As such, combinations of these medications with other QT-prolonging medications, such as methadone, quinolones, tricyclic antidepressants, amiodarone, anti-emetics (e.g. promethazine, haloperidol, droperidol, ondansetron), and numerous others can increase the risk of developing a toxic arrhythmia such as ventricular fibrillation. Curiously, one of the regimens being suggested for treatment of COVID-19 is a combination of HCQ and azithromycin, a combination which raises this potential concern regarding additive/synergistic QT prolongation.
- PHARMACOKINETIC DDIs
- P-glycoprotein Activity
The P-glycoprotein (P-gp) transport system is an efflux transporter found most notably in gut luminal and blood-brain barrier endothelial cells. CQ and HCQ are both inhibitors of this transporter/pump.(3) Some of the drug interactions specifically listed in the package inserts, i.e. both drugs increasing cyclosporine levels and HCQ increasing digoxin levels, are almost certainly attributable to CQ and HCQ inhibiting P-gp activity, insofar as both cyclosporine and digoxin are well-known substrates of this cellular pump. Additionally, the peer-reviewed literature contains several reports documenting the interaction of chloroquine and cyclosporine.(4)
As immunologically-challenged patients are considered to be at increased risk for a more frequent and more severe COVID-19 clinical course, clinicians should be especially cognizant of these potential DDIs.
- Cytochrome P450 Activity
The cytochrome (CYP) P450 system is the main family of enzymes responsible for Phase I (oxidative metabolism) of numerous drugs. These drugs undergo metabolism by several enzymes. The major metabolic enzymes of chloroquine include CYP2C8 and CYP3A4/5.(5) Hydroxychloroquine is a substrate of CYP2C8, CYP3A4/5, and CYP2D6 and has been demonstrated to elevate metoprolol levels via CYP2D6 inhibition.(6) Polymorphisms in these enzymes may also alter disposition.(7)
Cimetidine is a CYP450 pan-inhibitor. Enzymatic inhibition by cimetidine occurs only after several days. Predictably then, chloroquine/cimetidine and/or hydroxychloroquine/cimetidine co-administration results in possible increases in both CQ and HCQ levels.(8)
Although the package inserts and peer-reviewed literature are silent on the matter, clinicians should also be cognizant that co-administration of inhibitors of CYP2C8 (gemfibrozil and clopidogrel) and inhibitors of CYP 3A4/5 (verapamil, diltiazem, azole anti-fungal agents, most macrolide antibiotics, and ciprofloxacin, among others) may potentially raise the blood levels of CQ and HCQ.
Clinical Considerations
Both chloroquine and hydroxychloroquine are complex drugs from a pharmacokinetic and pharmacodynamics perspective. Due to the large volume of distribution and strong tissue binding properties of these drugs, the terminal half-life is 1-2 months.(9) With the numerous DDIs that are currently known and that are potential, use of these agents with other drug therapy requires consideration for patient safety. Studies are currently on going to demonstrate value for COVID-19 treatment.
References
- Chloroquine phosphate: https://www.accessdata.fda.gov/drugsatfda_ docs/label/2009/083082s050lbl.pdf, last accessed March 22, 2020.
- Hydroxychloroquine sulphate (Plaquenil): https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/009768s037s045s047lbl.pdf, last accessed March 22, 2020.
- Tiberghien F, Loor F. Ranking of P-glycoprotein substrates and inhibitors by a calcein-AM fluorometry screening assay. Anticancer Drugs. 1996 Jul;7(5)568-78.
- Nampoory MR, Nessim J, Gupta RK, Johny KV. Drug interaction of chloroquine with ciclosporin. 1992;62(1):108-9.
- Kim KA, Park JY, Lee JS, Lim S. Cytochrome P450 2C8 and CYP3A4/5 are involved in chloroquine metabolism in human liver microsomes. Arch Pharm Res. 2003 Aug;26(8):631-7.
- Somer M, Kallio J, Pesonen U, Pyykko K, Huupponen R, Scheinin M. Influence of hydroxychloroquine on the bioavailability of oral metoprolol. British Journal of Clinical Pharmacology. 2000 May;49(6)549-554.
- Lee JY, Vinayagamoorthy N, Han K, Kwok SK, Ju JH, Park KS, Jung SH, Park SW, Chung YJ, Park SH. Association of polymorphisms of cytochrome P450 2D6 with blood hydroxychloroquine levels in patients with systemic lupus erythematosus. Arthritis Rhematol. 2016 Jan;68(1):184-90.
- Furst DE. Pharmacokinetics of hydroxychloroquine and chloroquine during treatment of rheumatic diseases. 1996 Jun:5 Suppl 1:S11-5.
- Titus EO. Recent developments in the understanding of the pharmacokinetics and mechanism of action of chloroquine. Therapeutic Drug Monitoring. 1989;11(4)369-79.