Disclaimer: We aim to present letters from our readership that may generate further discussion on managing patients with COVID-19. Given the novelty of COVID-19, best-available clinical evidence is limited and supported from anecdotal reports from China, South Korea, Italy and other sites, and from studies of previous epidemics like SARS and MERS. The opinions expressed are those of the authors and not the APSF. These materials are presented for informational and educational purposes only and do not establish a standard of care or constitute medical or legal advice. The APSF does not support or endorse any specific idea, product, equipment, or trademarked technique. We strongly promote consistency with your governing bodies and organizations such as the CDC, WHO, ASA, AANA, and AAAA. Readers are reminded to consult with their institutions and medical/legal advisors regarding any of the views and opinions expressed by the authors.

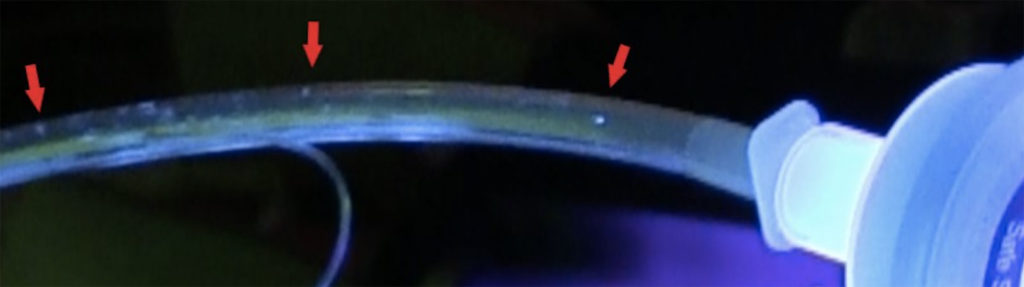
Figure 1. Glo Germ particles inside of the elbow connector of the anesthesia circuit are shown (red arrows).
Glo Germ (Flo Germ, Moab, UT) is a commercially available fluorescent marker. It consists of 5 mm particles. It is sold in powder form and oil-based suspension of a melamine copolymer resin.1 It is used in conjunction with ultraviolet light (UV) (black light) which allows for visualization of small particles in the environment. This formulation has been used to educate healthcare workers regarding the proper technique for donning and doffing of personal protective equipment (PPE) and has allowed for the observation that personnel contamination with infectious materials of different kinds can occur.2,3 Contamination of anesthesia workspace has been previously studied with a similar fluorescent marker called DAZO (CAE, Quebec, Canada).4
We present our experiment in which we used fluorescent marker in its liquid form to demonstrate spread of small 5 mm particles within the anesthesia circuit towards the anesthesia machine to identify areas of potential contamination with infectious particles. We hypothesized that if larger particles such as fluorescent marker can travel towards the anesthesia machine during mechanical ventilation, so would a much smaller particle, such as aerosolized COVID 19.

Figure 2. Glo Germ particles observed in inspiratory and expiratory limb of the anesthesia circuit (red arrows).
For the purpose of creating aerosolized fluorescent marker, we used a stretch of oxygen tubing connected to a size E oxygen tank and regulator. The opposite end of the tubing was connected to the base of the nebulizer chamber, and then to a simplified T-piece, which was introduced into a simulator right mainstem bronchus. To create the aerosolization of fluorescent marker, we used a 50:50 mix of liquid and glycerin in the nebulizer chamber. In order for the mixture to aerosolize, we dialed the oxygen flow to between 6-10L/minute and waited about 1 minute before we noticed a smoke like haze coming through a T-piece. The experiment was done solely under visual inspection under UV light and we did not have means to measure particle size.
In order to test the spread of particles in the ventilator of the anesthesia machine, we turned the machine to ventilator with the following settings: volume controlled ventilation, respiratory rate 12 breaths per minute, tidal volume 500 ml, positive end-expiratory pressure (PEEP) 5-10 cm H2O, and inspiratory flow of 2L/min.
Images show that particles that are 5 mm in size will travel through the anesthesia circuit to the exhalation valves and potentially into the machine if no filters are used. We show fluorescent marker particles in the elbow connector of the anesthesia circuit, inspiratory and expiratory limb of the anesthesia circuit, endotracheal tube before High Efficiency Particulate Air (HEPA) filter and also inside the HEPA filter (Figure 1-4) (Draeger, TX).
A pleated hydrophobic HEPA filter placed at the Y connector presumably prevented spread of the particles beyond the HEPA filter. This of course does not indicate that the HEPA filter is equally effective for much smaller particles, such as COVID-19, but it does demonstrate the effectiveness of HEPA filter to stop fluorescent marker spread towards the anesthesia machine. Other studies have demonstrated effectiveness of pleated hydrophobic HEPA filters down to a much smaller particle size, and therefor HEPA filters are the filters suggested for anesthesia professionals to use for COVID 19 patients.5
Our observations are limited by the non-physiologic aerosolization of the fluorescent marker. We did aerosolize fluorescent marker first and observed for 30 minutes whether just the oxygen flow at 10L/min without ventilation would drive the particles towards the anesthesia machine. That did not occur. This simulation also does not mimic humidity and temperature of a human being. This may be of relevance to small particle movement. Another limitation is the fluorescent marker particle size, which is larger by a factor of over 10 as compared to viral particles. We propose that smaller particles would be even more likely to travel towards the anesthesia machine.
Dr. Mojca Remskar Konia is currently a Professor in The Department of Anesthesiology at the University of Minnesota. She has no conflict of interest.
Dr. Asish Abraham is currently a first-year anesthesia resident in The Department of Anesthesiology at the University of Minnesota. He has no conflict of interest.
Dr. Janet Hume is currently an Assistant Professor in The Division of Pediatric Critical Care Medicine at the University of Minnesota. She has no conflicts of interest.
Dr. Gwenyth Fisher is an Associate Professor in The Division of Pediatric Critical Care Medicine at the University of Minnesota. She has no conflicts of interest.
References
- Oberyszyn AS, Robertson FM. Novel rapid method for visualization of extent and location of aerosol contamination during high-speed sorting of potentially biohazardous samples. Cytometry 2001; 43: 217-222.
- Osei-Bonsu K, Masroor N, Cooper K, et al. Alternative doffing strategies of personal protective equipment to prevent self-contamination in health care setting. Am J Infection Control 2019; 47: 534-539.
- Poller B, Hall S, Bailey C, et al. VIOLET: a fluorescence-based simulation experience for training healthcare workers in the use of personal protective equipment. J Hospital Infection 2018; 99: 229-235.
- Birnbach D, Rosen LF, Fitzpatrick M, et al. The use of novel technology to study dynamics of pathogen transmission in the operating room. Anesth Analg 2015; 120: 844-
- Wikles AR. Measuring the filtration performance of breathing system filter using sodium chloride particles. Anesthesia 2002; 57: 162-68.

 Articles
Articles