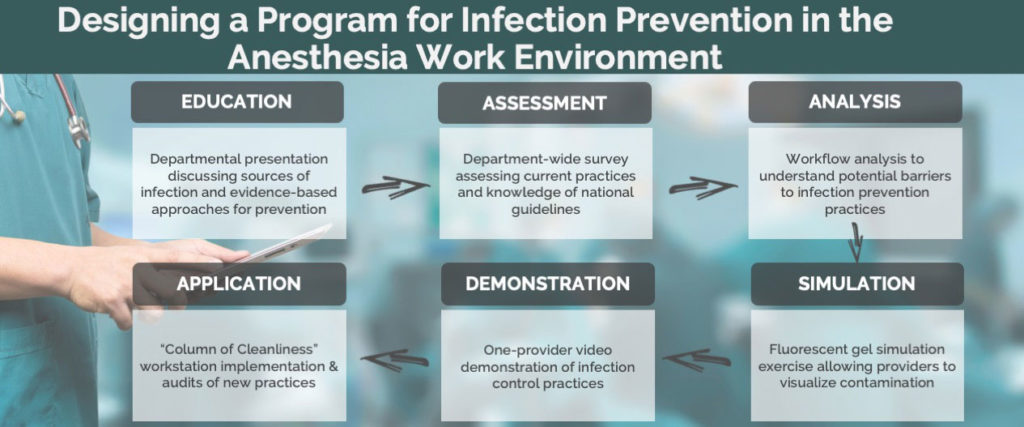
Intraoperative bacterial and viral contamination of the anesthesia work environment (AWE) has been directly linked to 30-day postoperative infections. At MedStar Georgetown University Hospital, we have implemented a multi-step program to educate providers on infection control practices to decrease bacterial and viral transmission in the AWE. This program is a combination of education, simulation, and demonstration allowing our anesthesia professionals to better understand and implement infection control practices.
Introduction
Intraoperative bacterial and viral contamination of the anesthesia work environment (AWE) has been directly linked to 30-day postoperative infections.1 Proven sites of contamination include patient skin, anesthesia professional’s hands, anesthesia equipment (including intravenous (IV) stopcocks), and the anesthesia workspace.1-5 At Medstar Georgetown University Hospital (MGUH) we have implemented a multistep program to education anesthesia professionals on infection control practices and to provide tools to decrease bacterial and viral transmission in the AWE.
Review
The first step in our infection prevention program included a mandatory department Grand Rounds by a nationally recognized authority. This presentation discussed the complex and alarming issue of healthcare-associated infections (HAIs) and how it applies to anesthesia professionals during the peri-operative period. The lecture also included potential sources of bacterial pathogen transmission and evidence-based approaches to address this problem.
Following this presentation, our hospital’s Division of Infection Prevention distributed a survey on infection control practices to our department. This was intended to evaluate our baseline knowledge of infection prevention and included questions regarding hand hygiene, IV port disinfection, glove use, and AWE cleanliness. The survey indicated that providers are frequently unfamiliar with national guidelines on hand hygiene and glove use. The survey (in person faculty meeting, 70% response rate) results displayed a lack of knowledge and awareness of infection control practices.
Next, we invited the MedStar National Center for Human Factors in Healthcare (MNCHFH) to observe and perform a workflow analysis. Two members conducted independent observations in our operating rooms over 3 days. These observations totaled 8.5 hours and were taken in 5 randomly selected operating rooms and 2 randomly selected endoscopy suites. The surveyors stayed throughout each anesthetic as well as during setup and turnover of each operating room surveyed. They observed anesthesiologists, CRNAs, SRNAs, anesthesia technicians and operating room nurses as well as the environmental services team and surveyed various types of anesthesia. During their analysis they documented elements of workflow, tool and end user goodness-of-fit, and cross-disciplinary team communication. The observations identified three areas in need of improvement – reduction of pathogen burden, reduction of pathogen transmission, and promoting a culture of safety. They found that several items, such as IV ports/stopcocks, anesthesia cart drawers, and anesthesia machine knobs, in the AWE were contaminated throughout each case. These contaminated areas and equipment were likely due to gaps in hand hygiene as well as a lack of environmental cleaning during and after the case. In addition, their data showed a 20% compliance with hand hygiene guidelines6-7 and a 10% compliance with guidelines on glove use8. Though there was a 50% compliance rate with IV port decontamination, in most cases, the contact time and friction used was insufficient for total decontamination. Furthermore, greater than 75% of port accessing occurred with contaminated hands or gloves. Lastly, they noted that alcohol-based hand rub and glove boxes were not in the field of view during anesthesia workflow.
The next step in our program included a department-wide DAZOÒ Fluorescent Marking Gel (Ecolab – St. Paul, MN) simulation exercise. DAZOÒ is a clear, transferrable liquid that can be seen only under ultraviolet light. This substance was applied in the mouth and axilla of a mannequin to represent potential sources of bacteria. The department was split into groups of 6 consisting of a combination of anesthesiologists, CRNAs, SRNAs, residents, and anesthesia technicians. Each small group was asked to demonstrate an induction of general anesthesia. Members of the department had no prior knowledge of the theme of the exercise. Ultraviolet light was used to observe areas that the DAZOÒ had spread to by the end of each case. This simulation demonstrated that the most frequently contaminated objects in the AWE include the facemask, monitor buttons, APL valve, medication syringes, IV tubing and injection ports.
Using the information and data gathered, a video demonstrating best practices for infection control was created (see Media 1). This video is a one-provider demonstration of infection control practices during the induction, maintenance, and emergence of a general anesthetic. It includes information on appropriate hand hygiene, glove use, and IV port / syringe tip decontamination for aseptic medication administration. In addition, it demonstrates methods to decrease pathogen burden and transmission in the AWE.
After demonstrating and educating the department on appropriate infection control practices, each operating room and satellite location was equipped with a “Column of Cleanliness” aimed to decrease the transmission of bacteria and viruses. This “Column of Cleanliness” is an infection control workstation, which includes IV port and syringe tip decontamination tools along with hand sanitizer and an airway bucket.
The workstation was implemented at MGUH in November 2018. After using these workstations for several months, two separate audits (see Table 1) were performed two months apart. During each of these audits, randomly selected operating rooms were observed without the anesthesia professional’s knowledge. The completion of specific infection control tasks by the provider was documented. These tasks included proper workstation set up, hand hygiene, glove use, IV port and syringe tip decontamination, and more.
Table 1 – Comparison of Audit #1 and #2
| Audit #1 N = 102 |
Audit #2 N = 98 |
|
| Workstation Set Up | 89.2 % | 100% |
| Hand Hygiene Avg. | 29.2% | 75.6% |
| Proper Glove Use Avg. | 88.6% | 98.7% |
| IV Port / Syringe Decontamination | 19% | 82.7% |
| Dirty Airway Basket Use | 40.9 % | 64.3% |
| AWE Wipe Down by Provider | 19.8% | 67.3% |
| Hand Hygiene Avg. – average performance of hand hygiene before touching the patient, after touching the patient, touching patient’s surroundings, performing clean aseptic procedures, exposure to bodily fluids. Proper Glove Use Avg. – average performance of glove use according to WHO guidelines. IV port/Syringe decontamination – both the IV port and syringe are separately decontaminated before use. Dirty Airway Basket Use – dirty airway equipment is directly placed in the basket to avoid further contamination of AWE. AWE Wipe Down by Provider – anesthesia provider wipes down the anesthesia machine, reservoir bag, and monitors after each induction. (statistical analysis not performed) | ||
The first audit showed that providers were using the workstation equipment and were practicing appropriate glove use. However, hand hygiene and IV port decontamination were not being done as frequently. During the second audit, both hand hygiene and IV port decontamination rates had improved significantly.
Following the audits, the MNCHFH re-visited the operating rooms to re-evaluate workflow, infection control practices, and usage of the infection control workstation. The same two individuals conducted six hours of observation. In addition, they conducted interviews with the anesthesia professionals regarding the newly implemented workstation and other elements of the anesthesia infection prevention program. They found that most providers had changed their practice to include hand hygiene, glove use, and IV port/syringe tip decontamination; however, the workflow was still not optimal. Often, providers were changing the location of the workstation throughout the case.
Lastly, a follow up survey was distributed to the department. Survey responses were collected during a two-month period by either in-person interviews or written questionnaires. Questions pertained specifically to the infection control workstation and potential improvements that could help compliance with appropriate infection prevention practices. Most providers felt that relocation of the workstation and glove boxes would continue to improve compliance. While having the workstation and glove boxes in the provider’s field of view (towards the patient) is essential, many felt that relocation of both items should be based on individual workflow to maximize use. Following a consensus, glove boxes are now located on the top of the anesthesia machine and the workstations are now located on top of the Pyxis machine. Both items are easily accessible and within reach of the provider throughout the entire case. Lastly, hand sanitizer dispensers have been installed at the entrance and exit of each operating room door.
Discussion
It is evident that anesthesia professionals have not yet adopted infection prevention guidelines into their practice. As surgical site infections account for nearly 20% of all HAIs9, it is imperative that each anesthesia professional embraces these guidelines. Bacterial and viral transmission is multi-factorial and it’s crucial that we recognize and address each contributing source.
Hand hygiene is one key component that is desperately missing in our current routine. The World Health Organization (WHO) recommends 5 moments of hand hygiene (see Table 2).6 Besides keeping equipment, such as a hand sanitizer, in a convenient and easily accessible location, it is clear that providers must also be re-educated on the 5 moments. We have increased our hand hygiene compliance by demonstrating the 5 moments in our best practices video while also providing hand sanitizers on our “Column of Cleanliness”.
Table 2 – World Health Organization 5 Moments of Hand Hygiene
| 1. Before Touching a Patient |
| 2. Before Clean / Aseptic Procedures |
| 3. After Body Fluid Exposure / Risk |
| 4. After Touching a Patient |
| 5. After Touching Patient Surroundings |
An increase in glove use has unfortunately caused a decrease in hand hygiene in anesthesia practice. The WHO recommends that gloves should be worn during exposure to blood or body fluids as well as when in contact with “potential infectious material”. They have also noted that the excessive use of gloves in unnecessary situations does not lead to a reduction of bacterial transmission and may lead to missed opportunities for hand hygiene.8
Another opportunity for improvement is IV port decontamination. Each hub must be scrubbed with alcohol pads for at least 10-15 seconds to fully decontaminate the port.10 As studies have directly linked virulent pathogens on the IV port to post-operative infections, we must take all measures to ensure that each port is scrubbed sufficiently before administering medications.1-5 Our initial lack of compliance and inadequate disinfection resulted from the unavailability of supplies. Each of our operating rooms is now supplied with disinfecting caps that scrub the hub of the IV port as well as disinfecting caps to scrub the tips of syringes11.
Lastly, increased environmental cleaning during and between cases is essential in preventing bacterial and viral transmission between patients. We have implemented the use of disposable laryngoscopes, removable keyboard covers, and single use tape rolls. We also administer ultraviolet light treatment during “off” hours to our operating rooms. Lastly, we have incorporated a wipe down of the AWE and any contaminated areas or equipment after induction of each anesthetic and after completion of each case with Sani-Cloth germicidal, disposable wipes.
At MGUH, it was evident that both a lack of provider awareness and accessibility to infection prevention tools were hindering the implementation of infection control guidelines. Infection prevention requires a multi-prong approach, which includes provider awareness, education, and acceptance. In addition to supplying the “Column of Cleanliness” to each of our operating rooms, we have implemented this system to the 8 other anesthesia departments within MedStar Health. We plan to continue our infection prevention mission by conducting a study to evaluate our current process. This study includes 1,000 randomly selected patients and will identify and track bacterial pathogens in the operating room during and between cases. We hope to use this information to further identify obstacles or issues that lead to sub-optimal infection prevention practices in the anesthesia work environment. We recognize the challenge to comply completely with guidelines and practices, but we must continue to change the culture on how we view infection prevention in our specialty so we can continue to increase patient safety and improve outcomes.
Mausam Kuvadia, MD, MedStar Georgetown University Hospital, Hospital for Special Surgery
Russell Wall, MD, MedStar Georgetown University Hospital
Andjela Pehar, MD, MedStar Georgetown University Hospital
Kevin Nishida, MD, MedStar Georgetown University Hospital
Nellie Darling, MS, Georgetown University School of Medicine
Financial Disclosures: None.
Conflicts of Interest: None.
References
- Loftus RW, Brown JR, Koff MD, et al. Multiple reservoirs contribute to intraoperative bacterial transmission. Anesth Analg. 2012;114:1236‐1248. doi:10.1213/ANE.0b013e31824970a2
- Loftus RW, Koff MD, Brown JR, et al. The epidemiology of Staphylococcus aureus transmission in the anesthesia work area. Anesth Analg. 2015;120:807‐818. doi:10.1213/ANE.0b013e3182a8c16a
- Loftus RW, Koff MD, Burchman CC, et al. Transmission of pathogenic bacterial organisms in the anesthesia work area. Anesthesiology. 2008;109:399‐407. doi:10.1097/ALN.0b013e318182c855
- Loftus RW, Koff MD, Brown JR, et al. The dynamics of Enterococcus transmission from bacterial reservoirs commonly encountered by anesthesia providers. Anesth Analg. 2015;120:827‐836. doi:10.1213/ANE.0000000000000123
- Loftus RW, Koff MD, Birnbach DJ. The dynamics and implications of bacterial transmission events arising from the anesthesia work area. Anesth Analg. 2015;120:853‐860. doi:10.1213/ANE.0000000000000505
- WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care. Geneva: World Health Organization; 2009.
- Boyce JM, Pittet D; Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep. 2002;51(RR-16):1‐CE4.
- World Health Organization. Glove use information leaflet. [Accessed May 22, 2020]; Available from: http://www.who.int/gpsc/5may/Glove_Use_Information_Leaflet.pdf.
- Ban KA, Minei JP, Laronga C, et al. American College of Surgeons and Surgical Infection Society: Surgical Site Infection Guidelines, 2016 Update. J Am Coll Surg. 2017;224:59‐74. doi:10.1016/j.jamcollsurg.2016.10.029
- Simmons S, Bryson C, Porter S. “Scrub the hub”: cleaning duration and reduction in bacterial load on central venous catheters. Crit Care Nurs Q. 2011;34:31‐35. doi:10.1097/CNQ.0b013e3182048073
- Loftus RW, Brindeiro BS, Kispert DP, et al. Reduction in intraoperative bacterial contamination of peripheral intravenous tubing through the use of a passive catheter care system. Anesth Analg. 2012;115:1315‐1323. doi:10.1213/ANE.0b013e31826d2aa4
- Birnbach DJ, Rosen LF, Fitzpatrick M, Carling P, Munoz-Price LS. The use of a novel technology to study dynamics of pathogen transmission in the operating room. Anesth Analg. 2015;120:844‐847. doi:10.1213/ANE.0000000000000226
- Birnbach DJ, Rosen LF, Fitzpatrick M, Carling P, Arheart KL, Munoz-Price LS. Double gloves: a randomized trial to evaluate a simple strategy to reduce contamination in the operating room. Anesth Analg. 2015;120:848‐852. doi:10.1213/ANE.0000000000000230
- Fernandez PG, Loftus RW, Dodds TM, et al. Hand hygiene knowledge and perceptions among anesthesia providers. Anesth Analg. 2015;120:837‐843. doi:10.1213/ANE.0000000000000408
- Koff MD, Loftus RW, Burchman CC, et al. Reduction in intraoperative bacterial contamination of peripheral intravenous tubing through the use of a novel device. Anesthesiology. 2009;110:978‐985. doi:10.1097/ALN.0b013e3181a06ec3

 Articles
Articles