Letter to the Editor:

The impact of The World Health Organization’s (WHO) 2008 Safe Surgery Saves Lives campaign has been significant. Further support for the initiative comes from the Joint Commission’s Universal Protocol requiring completion of a safety checklist before “all surgical and non-surgical invasive procedures.” Outside the operating room, pre-procedure checklists are used in GI Suites, Interventional Radiology units, and Vascular Labs. Labor & Delivery units should be no different. Parturients requesting a labor epidural deserve adherence to the Joint Commission’s safety standards also. Just as a surgical patient is “cleared for take-off” by completion of a checklist, a similar routine should be followed before the placement of a labor epidural. Our Labor Epidural Time Out (LETO) checklist (fig. 1), which was introduced in October 2011 and revised in May 2014, is used by all members of our Obstetric Anesthesia Team at MedStar Georgetown University Hospital.
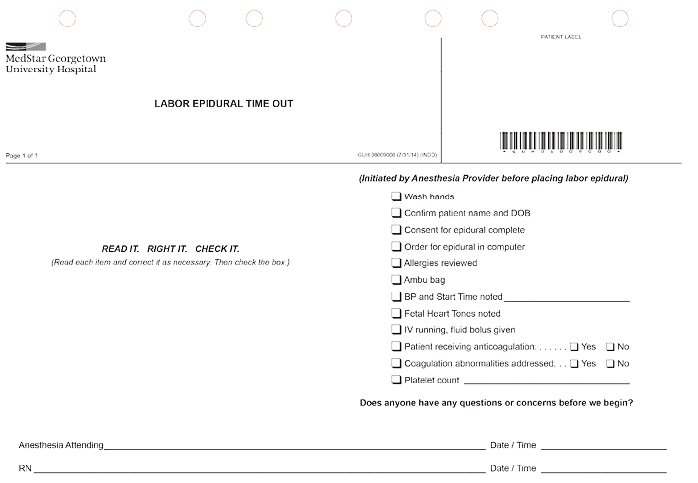
Example of the labor epidural time out checklist.
Year after year, the Joint Commission reports errors in team communication as a significant cause of sentinel events.1 Various communications tools that require minimal monetary resources to implement and little time to perform on a daily basis include the “Huddle,” “Time Out,” or “Pause for Cause.” These tools enhance communication among all team members and have been shown in various settings to improve patient outcomes. A recent meta-analysis of cohort studies utilizing safety checklists for surgery noted that, “. . . checklists appear to be associated with” a reduction in the risk of major complications.2 Conducting a randomized controlled study to unequivocally prove this point would not be pragmatic since omission of the safety checklist for half of all subjects would be required.
One measure of the utility of a checklist is determined by the frequency with which a patient’s care plan is modified as the checklist is completed. This is shown to occur as often as 48% of the time,3 which is consistent with our observations in the use of the LETO checklist. In our review of the use of the LETO checklist, hand washing was the most common item to be prompted by the checklist followed closely by completion of the consent for epidural. Their obvious importance and high “hit-ratios” do not indicate that other items are less valuable. Soon after we started using the LETO checklist, its usefulness was demonstrated when a latex allergy was noted as a team member was donning latex gloves.
Our LETO checklist was created by including items that are universal to pre-procedure checklists, such as identification of the patient, verification of their allergies, confirmation of a completed consent, and availability of emergency equipment (including resuscitation drugs). Items unique to laboring patients and placement of an epidural were then added. For example, we make note of the platelet count and pre-procedure blood pressure as well as asking about the use of anticoagulants and concerns regarding fetal heart tones. Hand washing was at the top of our list because it is the standard way to begin a sterile procedure—and we knew we needed a reminder if we were to achieve our goal of 100% compliance in this regard.
The WHO’s original surgical safety checklist is an excellent template. With 19 items, it is both thorough and efficient. More focused on pre-surgical issues, the WHO’s recommendation to “modify and revise” is advantageous when constructing a LETO checklist. Modifications that are contextually responsive as well as revisions highlighting changing circumstances and near-miss situations maintain its high level of utility. We found that we could make better use of recently adopted electronic medical records (EMR) in our Labor & Delivery Unit after a near-miss situation—a patient received an anticoagulant before her epidural catheter had been removed. If the order for the placement of the epidural had been entered into the computer at the appropriate time, our nurses, obstetricians, and pharmacy would have been alerted to the situation by the EMR before the anticoagulant had been given. We now include, “Order for epidural in computer?” as an item on our LETO checklist; just one example of the benefit of regular checklist modifications.
With the abundance of information to be processed before placing an epidural and the speed at which the entire team moves in response to the patient in obvious pain, a sense of urgency and confusion can develop. The ability of the checklist, once completed, to reduce distraction and uncertainty, is a welcome effect, allowing for a more complete focus on the task at hand.
We are now considering the formulation of a second part of the LETO checklist analogous to the debriefing portion of the Time Out performed in the operating room. After placement of the labor epidural, we should confirm the frequency of blood pressure measurements and the blood pressure parameters to be maintained. An estimate for the time of onset of the epidural, notification of an inadvertent dural puncture, or encouragement for the patient to notify the team if the block becomes one-sided should be communicated to everyone. Finally, assuring that the nurse is aware of the anesthesia team’s contact numbers would also be practical.
Laboring women anxious for pain relief can be intolerant of delays. Some physicians also occasionally consider a safety checklist too “cumbersome” or “time consuming”.4 Because these attitudes are not uncommon, it is understandable that there is wide variability in the completion of the checklist. Lapses in care that would be noted by a properly conducted safety checklist are unacceptable, but do occur. Since reading each item aloud, correcting any deficiency, and then checking the box is critical to its effectiveness, we have noted this on our LETO checklist form. Experts in human factors engineering recommend these structured communication processes along with continual revisions of the checklist content as most effective in assuring safety.5 They use the phrase “design trumps training” and believe that writing new policies or attempts at reeducating staff are weak responses to adverse events.6
We believe that combined with improvements in the mechanics of checklist completion, development of positive attitudes can be a powerful prevention to the silence that condones improper performance or complete disregard for a safety checklist. Ultimately, the key to success is a culture of safety that encourages and empowers all members to speak up for the safety of the patient.
Our 12-item LETO checklist has been well received by both nurses and anesthesiologists. While there is an ongoing desire to improve the checklist’s utility it should not blind us to the circumstances of our laboring patient. Labor can be anxiety-provoking, painful, and dangerous. Although safety is of utmost importance, the checklist can never be comprehensive. Careful consideration is required to balance the number of items on the checklist with the time needed for its completion. This, combined with regular revisions will play an important role in the utility, acceptance, and support of this safety initiative.
Joseph W. Myers, MD, is an Associate Professor of Anesthesiology at MedStar Georgetown University Hospital in Washington, DC. John Kwock, MD, is a CA3 Anesthesiology Resident at MedStar Georgetown University Hospital in Washington, DC. Disclosure: There are no financial gains associated with the writing or content of this article.
References
- The Joint Commission. Sentinel Event Data Summary. September 30, 2014. Available at: http://www.jointcommission.org/sentinel_event_statistics_quarterly/. Accessed December 9, 2014.
- Gillespie BM, Chaboyer W, Thalib L, John M, Fairweather N, Slater K. Effect of using a safety checklist on patient complications after surgery: A systematic review and meta-analysis. Anesthesiology 2014;120:1380-9.
- Myers JW, Gilmore BE, et al. The utility of the surgical safety checklist for wound patients. Int Wound J 2015; In Press.
- Stoelting RK. APSF survey helps to establish pre-induction checklist. APSF Newsletter 2013;28:1, 11-13.
- Dunn EJ, Mills PD, Neily J, Crittenden MD, Carmack AL, Bagian JP. Medical team training: Applying crew resource management in the Veterans Health Administration. Jt Comm J Qual Patient Saf 2007;33:317-25.
- Weinger MB, Gaba DM. A case report from the anesthesia incident reporting system. ASA Newsletter 2014;78(8):44-6. Available at: https://www.asahq.org/For-Members/Publications-and-Research/Periodicals/ASA-Newsletter.aspx. Accessed December 9, 2014.


 Issue PDF
Issue PDF