![]() Dear Q&A,
Dear Q&A,
What are the health hazards from UV exposure when UV radiation is used for infection control in the operating room? Could you comment on the effectiveness of sunscreen and Personal Protective Equipment in protecting patients and OR staff? What safety measures should be in place to monitor for photokeratitis, basal cell carcinoma, actinic keratitis, and melanoma?
Kathy Crysel, CRNA
Winston Salem, NC, 27157
![]() Dear Ms. Crysel,
Dear Ms. Crysel,
Thank you for your question regarding the hazards of using ultraviolet radiation in operating rooms to control infections.
The development of virulent bacteria that are resistant to multiple antimicrobial treatments is occurring around the world1 and one of the proposed solutions to minimize wound infections is exposure to ultraviolet radiation. Ultraviolet germicidal irradiation (UVGI) appears to be effective in reducing the risk of surgical site infection2-4 including MRSA. The routine use of ultraviolet radiation in orthopedic operating rooms is well known and has been recently investigated by National Institute for Occupational Safety and Health.5
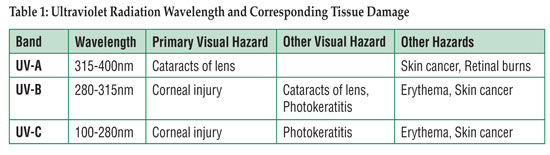
Ultraviolet radiation can be divided into 3 regions of the ultraviolet spectra as illustrated in Table 1. The most common wavelength in operating rooms because of its germicidal effects is 254 nanometers, in the UV-C range, which is also invisible to humans. All of the UV wavelengths can be responsible for health risks dependent upon the intensity and wavelength of the source, distance from the source, and length of exposure to the source. Table 1 also summarizes the hazards.5
Ocular damage generally begins with photokeratitis, but can also result in keratoconjunctivitis and photo-keratoconjunctivitis depending upon the dose and length of exposure. Symptoms may not be evident until 6-12 hours after exposure and may include an abrupt sensation of sand in the eyes, tearing, and eye pain, possibly severe. These symptoms generally resolve within 24-48 hours, leaving no permanent damage. Eye damage can be completely avoided by wearing protective eyewear in any and all cases where direct UVC energy may be present.
Cutaneous damage consists of erythema; it’s like sunburn with no tanning. Acute overexposure to UV-C energy can be incapacitating, but generally regresses after several days, leaving no permanent damage, possibly because of limited depth of skin penetration. Skin damage can be completely avoided by covering all exposed skin in any and all cases where direct UV-C energy may be present. While keratoacanthoma-like tumors appeared in rats exposed to UV-C, and squamous-cell carcinoma and fibrosarcoma appeared in mice, UV-C has not been shown to be associated with melanoma or basal cell carcinoma.6 There are no conclusive data to link UV-C to skin cancer in humans.
Exposure threshold limit values for UV radiation have been established by the American Conference of Governmental Industrial Hygienists.7 The Occupational Safety and Health Administration (OSHA) has not established a standard for safe exposure to ultraviolet light. However, the National Institute for Occupational Safety and Health (NIOSH) developed a permissible exposure limit at a wavelength of 254 nanometers (the peak intensity of most UV-C germicidal lamps) which is 0.2 watts/cm2 for 8 hours. The severity of effects from UV light are dependent upon the intensity and wavelength of the source, distance from the source, length of exposure to the source, sensitivity of the individual, and the presence of sensitizing agents.5
The National Institute for Occupational Safety and Health studied a Boston Hospital that used UV-C radiation produced by ceiling mounted UV lamps in orthopedic operating rooms. Personal dosimetry was employed to measure UV-C exposure in 3 orthopedic operating rooms. Orthopedic OR staff wore scrub shirts and a warm-up jacket or surgical gown to make 2 layers of personal protective equipment. Dosimetry measurements indicated safe levels of UV-C measured at the skin of the shoulder (under 2 levels of personal protective equipment). However, UV-C exposure was 6-28 times the NIOSH recommended exposure limit when dosimeters were placed on the surface of the personal protective equipment. Not all surgical hats, gowns, and masks protect adequately from UV-C radiation.
In summary
The severity of effects from UV light are dependent upon the intensity and wavelength of the source, distance from the source, length of exposure to the source, sensitivity of the individual, and the presence of sensitizing agents.5 Sun screen is not recommended as a reliable method of protection from UV-C. NIOSH recommends a UV-C and Personal Protective Equipment training program for employees who will be exposed to UV-C in the operating room. Personal Protective Equipment must be approved for use in the UV-C environment. The recommendations include establishment of a medical surveillance program for all OR personnel exposed to UVGI with periodic skin screenings.6
A. William Paulsen, Ph.D.
Chair, APSF Committee on Technology
Vice President of Education
South University, Savannah, GA
References
- McGeer A, Low D, Conly J, et al. Methicillin-resistant Staphylococcus aureus in Ontario. Can Commun Dis Rep 1997;23:45-6.
- Hart D. Bactericidal ultraviolet radiation in the operating room. Twenty-nine year study for control of infections. JAMA 1960;172:1019-28.
- Brown IW Jr., Moor GF, Hummel BW, Marshall WG Jr., Collins, JP. Toward further reducing wound infections in cardiac operations. Ann Thorac Surg 1996;62:1783-9.
- Ritter MA, Olberding EM, Malinzak RA. Ultraviolet lighting during orthopedic surgery and the rate of infection. J Bone Joint Surg 2007;89:1935-40.
- University of Rochester, Environmental Health and Safety: Industrial Hygiene Programs: UV Light. Ultraviolet light safety guidelines. Rochester, NY. September 21, 2009. Available at: http://www.safety.rochester.edu/ih/uvlight.html. Accessed April 28, 2010.
- Sylvain D, Tapp L. Health hazards evaluation report: UV-C exposure and health effects in surgical suite personnel, Boston, MA. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, NIOSH HETA No. 2007-0257-3082. 2009.
- ACGIH®Ultraviolet Radiation: TLV® Physical Agents. 7th Edition Documentation. Publication #7DOC-656. Available at http://www.acgih.org/store/ProductDetail.cfm?id=1359. Accessed May 11, 2010.
Numerous questions to the Committee on Technology are individually and quickly answered each quarter by knowledgeable committee members. Many of those responses would be of value to the general readership, but are not suitable for the Dear SIRS column. Therefore, we have created this simple column to address the needs of our readership.
The information provided is for safety-related educational purposes only, and does not constitute medical or legal advice. Individual or group responses are only commentary, provided for purposes of education or discussion, and are neither statements of advice nor the opinions of APSF. It is not the intention of APSF to provide specific medical or legal advice or to endorse any specific views or recommendations in response to the inquiries posted. In no event shall APSF be responsible or liable, directly or indirectly, for any damage or loss caused or alleged to be caused by or in connection with the reliance on any such information.


 Issue PDF
Issue PDF