 In 1996 the American College of Cardiology (ACC) and the American Heart Association (AHA) published the consensus opinion on guidelines for the perioperative evaluation of patients having noncardiac surgery.1 The guidelines were intended for physicians involved in the preoperative, operative, and postoperative care of these patients. The impact of these published guidelines is unknown; however, it is likely that contemporary care of patients presenting for noncardiac surgery has been favorably altered by adherence to these guidelines. Now, 6 years later, the task force has updated and widely published these guidelines.2 The stated goals of the task force guidelines are to “identify the most appropriate testing and treatment strategies to optimize the care of the patient, provide assessment of both short- and long-term cardiac risk, and avoid unnecessary testing in an era of cost containment.”
In 1996 the American College of Cardiology (ACC) and the American Heart Association (AHA) published the consensus opinion on guidelines for the perioperative evaluation of patients having noncardiac surgery.1 The guidelines were intended for physicians involved in the preoperative, operative, and postoperative care of these patients. The impact of these published guidelines is unknown; however, it is likely that contemporary care of patients presenting for noncardiac surgery has been favorably altered by adherence to these guidelines. Now, 6 years later, the task force has updated and widely published these guidelines.2 The stated goals of the task force guidelines are to “identify the most appropriate testing and treatment strategies to optimize the care of the patient, provide assessment of both short- and long-term cardiac risk, and avoid unnecessary testing in an era of cost containment.”
The updated guidelines are based on a literature search from 1995 to 2000, which identified 400 new articles. Twelve committee members representing the fields of cardiology, medicine, surgery, and anesthesiology reviewed these articles. Draft guidelines were prepared and submitted to the executive officers representing the ACC and the AHA. The final recommendations weigh the medical evidence for a given test, therapy or intervention, and assign a summary score (Table 1).
A stepwise approach to preoperative testing to assess coronary risk is presented (Figure 1). This algorithm was published in the 1996 guidelines and provides an orderly assessment of clinical markers, prior coronary evaluation and treatment, functional capacity, and surgery specific risk. The guidelines provide an excellent discussion of each parameter and its influence on the subsequent recommendation. Perhaps the greatest attribute of these guidelines is the combination of these complex factors into one organized flow chart. Such a presentation allows the clinician the opportunity to make rational outcome-based therapeutic decisions.
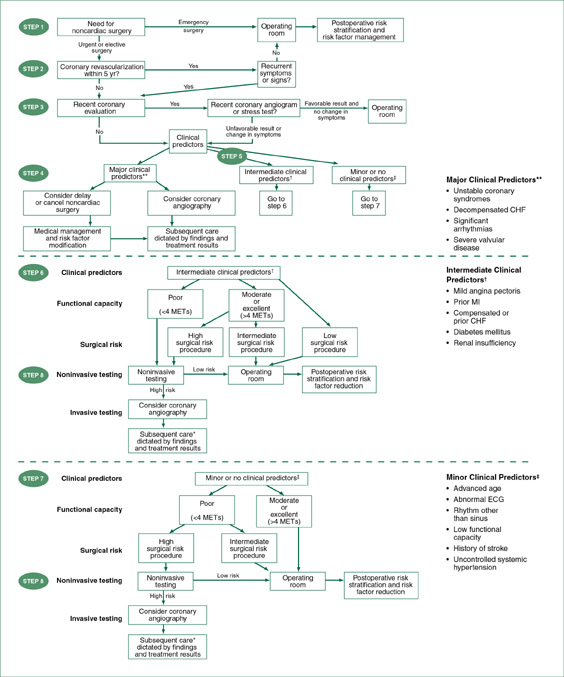
(Reprinted with permission from Anesth Analg 2002;94:1052-1064.) Figure 1. Stepwise approach to preoperative cardiac assessment. *Subsequent care may include cancellation or delay of surgery, coronary revascularization followed by noncardiac surgery, or intensified care.
Management of specific preoperative cardiovascular conditions is reviewed. The impact of hypertension, valvular heart disease, myocardial disease, arrhythmias, and conduction abnormalities and implantable pacemakers is discussed. In addition, several aspects of supplemental preoperative evaluation are also reviewed and recommendations using the relative grading scale are provided (Table 1). Specifically, there are recommendations for preoperative noninvasive evaluation of left ventricular function, 12-lead ECG, exercise stress testing, and coronary angiography. Clearly, these are disease states and evaluation tools that are of paramount importance to the practicing perioperative clinician.
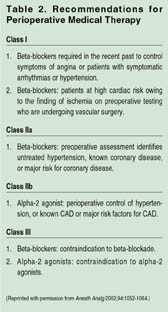
Several recent reports have focused on initiating medical therapy prior to surgery in an attempt to reduce perioperative morbidity and mortality. The guidelines review this literature and provide recommendations of beta-blockers and alpha-2 agonists (Table 2). The authors suggest that appropriate administration of beta-blockers reduces perioperative ischemia and cardiovascular risk. When possible, beta-blockers should be started days or weeks before elective surgery, with a target heart rate between 50 and 60 beats per minute (see Perioperative Beta-Blockade article, page 21 of the Summer 2002 issue of the APSF Newsletter).
As in the previous guidelines, there are recommendations for anesthetic considerations, intraoperative management, perioperative ischemia surveillance, and postoperative and long-term management. Not surprisingly, specific anesthetic techniques are recommended. Appropriate pain management and perioperative maintenance of body temperature are also highlighted as effective therapies for risk reduction.
The authors recognize that perioperative cardiovascular morbidity and modalities can never be entirely eliminated. Should a myocardial infarction (MI) occur, the mortality rate remains at 40% to 70%.3 Brief recommendations are made for a patient suffering a perioperative MI. These include consideration for prompt angioplasty, aspirin, beta-blockade, and possible angiotensin converting enzyme inhibitor therapy.
In summary, the updated ACC/AHA Guidelines for Perioperative Cardiovascular Evaluation for Noncardiac Surgery offers the clinician a well-organized, thoughtful, evidenced-based approach to these patients. These guidelines, provided to clinicians in all fields of perioperative care, can also be found on the internet at www.acc.org and www.americanheart.org.
Dr. Zvara is an Associate Professor in the Department of Anesthesiology at Wake Forest University School of Medicine, Winston-Salem, NC.
References
- Eagle KA, Brundage BH, Chaitman BR, et al. Guidelines for perioperative cardiovascular evaluation for noncardiac surgery. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Committee on Perioperative Cardiovascular Evaluation for Noncardiac Surgery. Circulation 1996;93:1278-317
- Eagle KA, Berger PB, Calkins H, et al. ACC/AHA Guideline Update for Perioperative Cardiovascular Evaluation for Noncardiac Surgery—Executive Summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Anesth Analg 2002;94:1052-64.
- Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. New Engl J Med 1995;333:1750-6.

