Editorial Reply
The minimum anesthesia machine checkout between each case should include a functional test of the ventilation and breathing circuits. The automated machine checkout procedure really only looks for leaks and possibly measures breathing circuit compliance. To perform a functional test remove the breathing bag from the bag arm and place it on the breathing circuit elbow where the mask or endotracheal tube is usually connected. Switch to ventilator mode and fill the bellows with oxygen. While the breathing bag is being mechanically ventilated, you will see if the machine is able to deliver positive pressure ventilation to the bag. Comparing the set tidal volume to the measured exhaled tidal volume after 7 or more breaths would have identified the problem in this case before the machine was used with the patient. The exhaled volume being much less than the volume set to be delivered. This functional test would also identify a leak in the breathing circuit in some machines or a leak in the breathing circuit plus low pressure side of the machine in others. As the ventilator bellows descend and then rise, if they continue to rise to lower and lower levels the breathing circuit is losing more gas then is entering from the common gas outlet. In the Aisys machine, if the waste anesthetic gas disposal system is not functioning properly and total gas flow is set to 1 or more liters/minute the positive end expiratory pressure will rise to displayed 12 cmH2O or greater. Depending upon where the machine measures and displays pressure, it may have been possible to observe a severe obstruction by looking at the inspiratory pressure or the inspiratory pressure waveform.
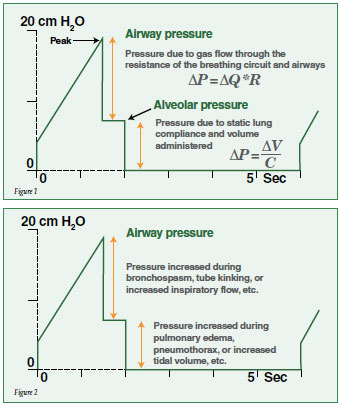
The pressure waveform in the volume control mode with inspiratory pause is a great way to separate airway resistance from alveolar pressure as pictured below. Normally the peak pressure is only a little higher than alveolar pressure. However, in Figure 1 there is significantly increased resistance in the breathing circuit and it appears as a large spike in the pressure. The peak pressure is a function of airway resistance times flow, indicating how a change in resistance can be observed from the waveform if the inspiratory flow remains constant. The airway flow can be increased by changing the I:E ratio from 1:1 to 1 to 10 for example.
When the inspiratory pressure is maintained constant (inspiratory pause) there is no more flow of gas into the lungs and the volume remains constant. This means that the airway pressure is equal to the alveolar pressure. The alveolar pressure is then related to the volume in the lungs divided by the static compliance of the lungs. If the tidal volume remains constant, then changes in alveolar pressure are related to changes in pulmonary compliance. A functional check of the breathing circuit should be performed before the start of every case.
Dr; Paulsen is Chair of the APSF Committee on Technology and Professor of Medical Sciences Frank Netter School of Medicine Quinnipiac University, Hamden, CT.


 Issue PDF
Issue PDF